Abstract
Objectives
To determine the average serum periostin level in children with asthma between 6 and 16 y of age, and to find out if the levels correlated with markers of eosinophilic inflammation, asthma control, and severity.
Methods
Children under follow-up at a tertiary care centre were enrolled. Children with conditions causing elevated serum periostin other than asthma, or history of systemic steroid use in the past 6 mo were excluded. Serum total IgE and periostin were estimated by ELISA.
Results
The median (IQR) serum periostin level was 52.6 (45.4, 58.3) ng/mL. Levels did not vary with age, gender, duration of symptoms, positive family history, or history of exacerbations in the last 6 mo. There was no significant correlation with anthropometric parameters or their z scores, or markers of eosinophilic inflammation in blood including serum total IgE, eosinophil percentage or absolute eosinophil count. There was no difference in median periostin levels of children with different asthma symptom control or asthma severity.
Conclusions
In a group of 26 Indian children with physician-diagnosed asthma, serum periostin showed no significant correlation to markers of eosinophilic inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma continues to be the most prevalent childhood chronic disease in the world [1]. However, there has been a paradigm shift in how asthma is viewed in recent years. Better understanding of the inflammatory pathways at play has resulted in the concept of asthma phenotypes and endotypes, the latter being classified as T2-high (eosinophilic) and Non-T2-high or T2-low (non-eosinophilic). A multitude of biomarkers have come to the forefront, promising less cumbersome delineation of these endotypes, with possibilities for asthma therapy being tailored to an individual [2].
Currently, there is no clear evidence in favor of any single biomarker. Periostin, an extracellular matrix protein expressed in a number of body tissues, holds great promise as a marker of T2-high inflammation. It plays a role in wound and fracture healing, bone formation, fibrosis, angiogenesis, atherosclerosis, tumorigenesis, and metastasis [3,4,5]. In asthma, periostin is associated with greater bronchial hyper-reactivity, higher serum IgE, eosinophilic inflammation, and subepithelial fibrosis [6].
Studies have discovered widely different values for serum periostin in adult subjects and contradictory findings exist regarding the accuracy of serum periostin in predicting airway eosinophilia [7,8,9,10,11]. Highly variable values have been found in pediatric studies as well. Effects of age, gender, and growth have also not been explored adequately [12,13,14,15]. In a number of studies, children with asthma have been found to have higher serum periostin levels compared to healthy controls [16,17,18,19]. However, uncertainty persists regarding correlation between serum periostin and eosinophilic markers in children [20,21,22,23]. There is a paucity of studies in the pediatric age group, more so in Indian population.
Therefore, the current study was planned to find out the average serum periostin level in a group of Indian children with asthma. The authors hypothesized that childhood asthma being more commonly eosinophilic, serum periostin level might correlate with markers of the same and also with asthma control and severity, within the study group.
Materials and Methods
An observational, cross-sectional study was conducted at the pediatric pulmonology unit of a tertiary care center in Chandigarh, India. Children between 6 and 16 y of age, with physician-diagnosed asthma, based on symptoms including wheeze, shortness of breath, chest tightness and cough, and documented expiratory airflow limitation defined as FEV1 (forced expiratory volume in 1 second)/FVC (forced vital capacity) < 0.90 [24], were screened. Children with known heart, kidney or bone disease, atopic dermatitis, or malignancy; use of systemic steroids in 6 mo; features suggesting acute infection; known cause of hypereosinophilia or elevated serum IgE levels other than asthma, were excluded.
The primary outcome measure was serum periostin level. The secondary outcome measures were absolute eosinophil count (AEC), eosinophil percentage, total serum IgE and the assessed asthma symptom control, and asthma severity.
As the study was conducted during the COVID-19 pandemic, patients were first contacted by telephone. Eligible and willing participants were requested to physically visit the department. Written informed consent was taken from the parents or legally authorized representatives at the visit. The authors aimed to enrol 25 children as study subjects.
A printed questionnaire was used to record history including demography, presence and duration of asthma symptoms, number of exacerbations and emergency visits in the last 6 mo, previous hospitalizations, dose and frequency of asthma medications, and family history of chronic diseases with specific mention of asthma and atopy. Asthma symptom control was assessed and severity was defined for patients who had controlled symptoms, according to the GINA (Global Initiative for Asthma) recommendations, 2020 [24].
Vital signs, anthropometric parameters and systemic findings were recorded. The z scores for height, weight, and BMI (body mass index) for age were calculated using IAP (Indian Academy of Pediatrics) growth charts [25].
Blood samples were collected from all subjects. One aliquot of 2 mL was processed for a CBC (complete blood count) and differential count including AEC using an automated coulter analyzer. Another 4 mL of blood was collected in a plain vial for estimation of serum total IgE and serum periostin. The sample was allowed to clot at room temperature for 10–20 min, centrifuged at 3000 r.p.m. for 20 min for separation of serum, which was stored at −20ºC. Periostin level was estimated using a sandwich ELISA (enzyme-linked immunosorbent assay), manufactured by Bioassay Technology Laboratory, Shanghai, China, with a sensitivity of 0.251 ng/mL. Serum IgE levels were measured using an ELISA manufactured by Calbiotech, Inc, El Cajon, California, USA.
Data analysis was done using SPSS version 26, IBM Corp. Continuous data with normal distribution were presented as mean and standard deviation (SD) and with non-normal distribution, as median and interquartile range (IQR). Categorical data were presented as proportions (%). Pearson and Spearman correlation tests were used for determining correlation between parametric and nonparametric continuous variables, respectively and the correlation coefficients have been reported (r and rs). The entire population was classified based on asthma control and asthma severity and means and medians were compared across these groups. Comparison was done using independent samples t-test, Mann–Whitney U test and Kruskal–Wallis test. A p value of less than 0.05 was taken to be significant for all statistical tests.
The study protocol was approved by the institute ethics committee, including the changes made later, which allowed screening patients on phone, to ensure participant safety during the COVID-19 pandemic.
Results
During the study period, from August 2019 to December 2020, 75 children were screened. Eighteen had already stopped asthma treatment, 19 expressed their inability to visit during the pandemic, and 8 children met the exclusion criteria. The remaining 30 were called for physical visit. Out of these, 26 reported and were enrolled.
The mean (SD) age of the population was 11.7 (2.6) y. There were 17 (65.4%) boys and 9 (34.6%) girls. Symptom onset in 22 (84.6%) children was before 6 y of age. Median (IQR) duration of symptoms was 8.6 (4.9, 11.4) y.
All subjects were using short-acting beta-agonists (SABA) as rescue therapy. Table 1 provides number of children who had ever used inhaled corticosteroids (ICS) and long-acting beta-agonists (LABA) and those who were using them at enrollment. ICS used by the group included budesonide and fluticasone, whereas LABA included salmeterol and formoterol. The mode of drug delivery was metered dose inhaler in all patients. Over the last 6 mo, there had been a total of 9 exacerbations, experienced by 8 (30.8%) children. Proportions of children with controlled, partially controlled, and uncontrolled asthma, as well as, proportions with mild, moderate, and severe disease among those who had controlled asthma are mentioned in Table 1.
No child had leucocytosis or leucopenia. The mean (SD) eosinophil percentage was 6.6 (3.6)%, whereas the mean (SD) AEC was 504 (302)/mm3. The median (IQR) serum total IgE was 216.2 (159.0, 233.5) IU/mL, respectively. Serum total IgE showed a significant positive correlation with eosinophil percentage (rs = 0.441, p = 0.024) and AEC (rs = 0.453, p = 0.02). The median (IQR) serum periostin level in the present group was 52.6 (45.4, 58.3) ng/mL.
There was no significant correlation between serum periostin level and age or duration of symptoms, any of the anthropometric parameters or their z scores. There was no significant difference between median periostin levels on the basis of gender, positive family history, current or past ICS use, or history of exacerbations in the last 6 mo.
There was no significant correlation between serum periostin level and eosinophil percentage, AEC, or serum total IgE (Table 2). There was no significant difference in mean eosinophil percentage, mean AEC or median serum total IgE compared between children with periostin levels above and below the group median.
There was no significant difference in the median periostin levels of children with and without blood eosinophilia, taking an AEC cutoff of 500 cells/mm3 or of those with serum IgE levels above and below the group median (216.2 IU/mL).
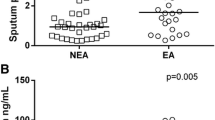
The median serum periostin levels compared across subgroups based on asthma symptom control and asthma severity, showed no significant difference. This is summarized in Fig. 1.
Discussion
ELISA was used to estimate serum periostin levels in a group of Indian children with asthma. There is a lot of heterogeneity in the assay methods used and the study population in terms of age and inclusion criteria in previously reported studies. Relatively higher values have been reported in the studies which have not used ELISA [12, 15]. Periostin levels in the present study population were comparable to those reported in Egypt, Finland, and Turkey [18, 19, 21]. The study conducted by Nejman-Gryz et al. in Poland enrolled children in the age group closest to the present study [20]. Periostin levels estimated by them were slightly lower. The possible reasons for this difference could be the subjects belonging to different populations and also, the cohort in Poland having a relatively milder phenotype.
An effect of age has been observed in many studies. An inverse correlation with age has been explained by a putative role of periostin in growth, manifesting with higher levels during greater bone turnover. It follows logically from this hypothesis, that the levels be correlated with anthropometric parameters as well. In the present study, no significant correlation was observed with age, or with height, weight, BMI or their z scores for age, which could be because of the smaller sample size and insufficient power. Also, median periostin levels were not significantly different between boys and girls. A significant effect of gender on serum periostin has also been seen, although in a few studies. In a group of children with uncontrolled asthma, boys had higher periostin values, whereas the values were higher in girls in a longitudinally followed cohort of children with significant parental history, but only at 11 y of age [15, 23].
In the present study, serum periostin levels did not correlate with blood eosinophil percentage, AEC, or serum total IgE. Till now, correlation of serum periostin with airway eosinophilia has not been consistent in literature. According to Jia et al., serum periostin was a better predictor of eosinophilia in sputum and endobronchial biopsies compared to blood eosinophils, serum IgE, and FeNO in adults with severe uncontrolled asthma [9]. Contrary to this, Wagener et al. showed that blood eosinophils and FeNO were better at predicting sputum eosinophilia than serum periostin in adults with asthma [11]. Simpson et al. also found blood eosinophils more accurate than serum periostin in this regard [10]. More studies in the pediatric population are required, using direct markers of airway inflammation, in sputum, bronchoalveolar lavage fluid, etc. If serum periostin, indeed, turns out to be a reliable predictor of airway eosinophilia, it will greatly simplify the conundrum of whether or not a patient would respond to inhaled steroids, and might further help in objective assessment of T2-high inflammation during therapy.
Evidence exists regrading a positive correlation of serum periostin levels with increasing asthma severity [18, 19]. Similar relationship with asthma control status has not been seen [19, 22]. On the other hand, Habernau Mena et al. showed mean periostin levels to be lower among children with severe asthma in a group of patients with uncontrolled asthma [23]. In the present cohort, serum periostin levels did not show any particular correlation with either asthma control status or severity grade. However, much importance cannot be assigned to this, as the subgroups in the present study were very small.
The present study is unique because it is the first study on serum periostin in Indian children. Physician-diagnosed asthma was used as inclusion criterion rather than using self-reported symptoms. None of the present study subjects had symptoms suggestive of allergic rhinitis or atopic dermatitis, which often coexist with asthma, and have been found to be independently associated with serum periostin.
The authors acknowledge certain limitations in the present study. The sample size was small, which would have limited the power to pick up significant relationships, more so, while doing subset analysis. The design was cross-sectional, whereas a longitudinal study would be better at exploring the effect of age. The present study did not have a control population, and so, serum periostin levels of healthy children could not be compared to those of the children with asthma. The authors also could not perform certain investigations like spirometry, sputum induction, and cytology and FeNO, which could have helped in more objective assessment of lung function and airway eosinophilia.
Conclusions
In a group of 26 Indian children with physician-diagnosed asthma, the median (IQR) serum periostin was 52.6 (45.4, 58.3) ng/mL, and had no significant correlation to markers of eosinophilic inflammation.
Data Availability
On reasonable request.
References
Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59:469–78.
Kuruvilla ME, Lee FE, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019;56:219–33.
Idolazzi L, Ridolo E, Fassio A, et al. Periostin: the bone and beyond. Eur J Intern Med. 2017;38:12–6.
Bonnet N, Garnero P, Ferrari S. Periostin action in bone. Mol Cell Endocrinol. 2016;432:75–82.
Liu AY, Zheng H, Ouyang G. Periostin, a multifunctional matricellular protein in inflammatory and tumor microenvironments. Matrix Biol. 2014;37:150–6.
Chiappori A, De Ferrari L, Folli C, Mauri P, Riccio AM, Canonica GW. Biomarkers and severe asthma: a critical appraisal. Clin Mol Allergy. 2015;13:20.
Okamoto M, Hoshino T, Kitasato Y, et al. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur Respir J. 2011;37:1119–27.
Kanemitsu Y, Matsumoto H, Izuhara K, et al. Increased periostin associates with greater airflow limitation in patients receiving inhaled corticosteroids. J Allergy Clin Immunol. 2013;132:305–12.
Jia G, Erickson RW, Choy DF, et al. Bronchoscopic Exploratory Research Study of Biomarkers in Corticosteroid-refractory Asthma (BOBCAT) Study Group. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol. 2012;130:647–54.
Simpson JL, Yang IA, Upham JW, et al. Periostin levels and eosinophilic inflammation in poorly-controlled asthma. BMC Pulm Med. 2016;16:67.
Wagener AH, de Nijs SB, Lutter R, et al. External validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthma. Thorax. 2015;70:115–20.
O’Connell P, Gaston B, Bonfield T, Grabski T, Fletcher D, Shein SL. Periostin levels in children without respiratory disease. Pediatr Pulmonol. 2019;54:200–4.
Fujitani H, Kasuga S, Ishihara T, at al. Age-related changes in serum periostin level in allergic and non-allergic children. Allergol Int. 2019;68:285–6.
Nakamura Y, Yokoyama Y, Nakajima K, Enomoto T, Fujiwara K, Takeuchi H. Serum periostin levels in adolescents. Asian Pac J Allergy Immunol. 2020. https://doi.org/10.12932/AP-010620-0868.
Anderson HM, Lemanske RF Jr, Arron JR, at al. Relationships among aeroallergen sensitization, peripheral blood eosinophils, and periostin in pediatric asthma development. J Allergy Clin Immunol. 2017;139:790–6.
Song JS, You JS, Jeong SI, at al. Serum periostin levels correlate with airway hyper-responsiveness to methacholine and mannitol in children with asthma. Allergy. 201570:674–81.
Inoue T, Akashi K, Watanabe M, et al. Periostin as a biomarker for the diagnosis of pediatric asthma. Pediatr Allergy Immunol. 2016;27:521–6.
El Basha NR, Osman HM, Abdelaal AA, Saed SM, Shaaban HH. Increased expression of serum periostin and YKL40 in children with severe asthma and asthma exacerbation. J Investig Med. 2018;66:1102–8.
Yavuz ST, Bagci S, Bolat A, Akin O, Ganschow R. Association of serum periostin levels with clinical features in children with asthma. Pediatr Allergy Immunol. 2021;32:937–44.
Nejman-Gryz P, Górska K, Krenke K, et al. Periostin concentration in exhaled breath condensate in children with mild asthma. J Asthma. 2021;58:60–8.
Knihtilä H, Kotaniemi-Syrjänen A, Pelkonen AS, Savinko T, Malmberg LP, Mäkelä MJ. Serum chitinase-like protein YKL-40 is linked to small airway function in children with asthmatic symptoms. Pediatr Allergy Immunol. 2019;30:803–9.
Licari A, Brambilla I, Sacchi L, Marseglia G, Ciprandi G. Periostin, type 2 biomarker, is not associated with asthma control grade in asthmatic allergic children. Respir Med. 2019;151:118–20.
Habernau Mena A, Del Pozo AV, Rodríguez Vidigal FF, Bobadilla GP. Role of Periostin in Uncontrolled Asthma in Children (DADO study). J Investig Allergol Clin Immunol. 2017;27:291–8.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2020. Available at: https://www.ginasthma.org. Accessed on 1 Oct 2020.
Indian Academy of Pediatrics Growth Charts Committee, Khadilkar V, Yadav S, Agrawal KK, et al. Revised IAP growth charts for height, weight and body mass index for 5- to 18-year-old Indian children. Indian Pediatr. 2015;52:47–55.
Funding
None.
Author information
Authors and Affiliations
Contributions
KK, MS, JLM, PCV, SVA contributed to the study conception and design; KK performed the material preparation, data collection, and analysis, and wrote the first draft of the manuscript; all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. MS will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institute Ethics Committee (Date 15/10/2019/No INT/IEC/2019/002167).
Consent to Participate
Written informed consent was obtained from the parents or legal guardians.
Consent to Publication
Written informed consent was obtained from the parents or legal guardians regarding the publication of data.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, K., Singh, M., Mathew, J.L. et al. Serum Periostin Level in Children with Asthma. Indian J Pediatr 90, 438–442 (2023). https://doi.org/10.1007/s12098-022-04282-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04282-1