Abstract
Asthma is the most common disease of childhood globally and acute asthma is the most significant risk factor for asthma-related death and chronic complications. This article will aim to synthesize the most up-to-date research and translate it into a more practical guide to managing acute asthma on a more daily basis. The use of clinical severity score is reviewed alongside the use of history and clinical findings in making objective assessments of patients presenting with acute asthma. Practical evidence-based pathways and a stepwise approach are provided for management of acute asthma in the home, outpatient, emergency, and intensive care settings. In doing so, popular myths are dispelled and practices in relation to management of acute asthma and use of asthma related medications are clarified. Having a standardized approach to management of acute asthma will bring us one step closer to reducing exacerbations and achieving the goal of having zero tolerance towards exacerbations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a common chronic disease of childhood. While it is known that acute attacks are preventable, acute asthma exacerbations are still the commonest reason for emergency visits and hospitalizations [1]. Asthma is still a contributor to mortality and in India, there were an estimated 82,000 deaths that occurred due to asthma across 2015 [2]. Early and effective care thwarts the severity of the episodes. This article will focus on effective management of acute asthma in children.
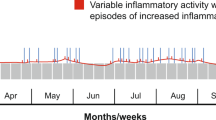
While acute asthma can be the initial presentation of asthma in a child, it usually occurs in children with pre-existing diagnosis of asthma. An acute asthma attack can be defined as increasing respiratory symptoms (cough, wheeze, or breathlessness) associated with fall in lung function [3]. Some of the common triggers for exacerbations include viral infections, exposure to allergens (such as house dust mite), and environmental pollutants such as smoke. Poorly controlled asthma increases the risk for exacerbations.
The hallmarks of acute asthma are severe bronchospasm, airway inflammation, mucus plugging, and ventilation–perfusion (V/Q) mismatch. Thus, the principles of management are based on (i) rapid reversal of airway obstruction (bronchodilators and anti-inflammatory medications) (ii) correction of hypoxia by oxygen administration, and (iii) prevention of relapses [1].
The management of acute asthma follows a stepwise escalation of care based on symptoms. This article will look at acute asthma management at different settings including home, outpatient departments, emergency rooms, and intensive care units. While this is a continuum, early and appropriate management can decrease the number of children requiring intensive care.
Management of Acute Asthma at Home
Families with children already diagnosed with asthma should ideally have a clear, documented plan for management of exacerbations along with adequate supplies of medications [4]. Any occurrence of respiratory symptoms such as cough, wheeze, difficulty in breathing, and tightness of chest should trigger action at home. Sometimes, parents may notice fast breathing or suprasternal and/or subcostal in-drawing as the only signs. Symptom-based initiation of care has reduced acute care visits to hospital.
Parents should have access to a short-acting β2-agonist (SABA) inhaler. The first step is to give 2–4 puffs of salbutamol through a metered dose inhaler (MDI) with a spacer. The dose varies between two to ten puffs in various programmes, but there is enough evidence to show that four puffs of a SABA through an MDI with spacer is equivalent to 2.5 mg (0.5 mL) of salbutamol via a nebulizer [5]. The early administration of SABA and review by parents is more important than the actual dose of SABA that is administered. The child should be re-evaluated 15 to 20 min after administration and the dose should be repeated if there is persistence of symptoms. If there is an improvement after delivering SABA, the child returns to receiving daily regular medication as prescribed. If the symptoms persist after two or three such doses, parents are advised to seek medical help. If the breathlessness worsens, the child is unable to speak in sentences, is very combative or drowsy, parents should be advised to seek immediate medical care in a clinic or an emergency unit. Similarly, children at high risk of asthma-related death [asthma-related pediatric intensive care (PICU) admissions in the past, hospitalizations, or emergency visits in the past year] should seek immediate medical care.
The debate between use of home nebulizers versus an MDI with spacer for acute exacerbations surprisingly continues. Studies have shown equivalence in efficacy between both methods and the superiority of an MDI with spacer in many ways; it is cheaper, easily portable, faster to administer, and environmentally friendly. Children with nebulizers prescribed at home have higher mortality because these families tend to delay seeking help [6].
Most children who require only a few doses of SABA at home do not require oral steroids. However, children who have had significant asthma exacerbations in the past or have had previous PICU admissions for asthma should have a course of oral prednisolone on standby. A dose of 1–2 mg/kg body weight is prescribed in 1 to 2 divided doses for 3 to 5 d and it should be used as soon as possible when the child has a partial or no response to SABA. Doubling or even quintupling the dose of baseline ICS during an exacerbation has not been shown to be useful [7].
Management of Acute Asthma in an Outpatient Clinic
Children are often seen in outpatient clinics with acute asthma. Having a simple algorithmic chart (such as in Fig. 1) in the clinic is helpful to maintain a consistent stepwise approach to asthma management. Clinics are also advised to have a pulse oximeter and oxygen available.
Assessment
The assessment starts with a good quick history. Important components of the history include time of onset and progression of symptoms, medications given during this episode, response to SABA if given at home, and use of SABA in the recent past. Sometimes it is possible to identify the trigger for the exacerbation (viral infection or exposure to an allergen, etc.). It is also vital to get a history of high-risk factors associated with increased morbidity and mortality such as previous PICU admissions, history of recent hospitalizations, oral steroid use, and history of rapidly progressive courses of illnesses. These high-risk children will need to be referred to a hospital after initial stabilization [8]. Clinical examination including sensorium, vitals, saturations, and a respiratory examination are essential. Several clinical scoring systems are validated for assessing severity of asthma exacerbation. One such commonly used scoring system is shown in Table 1 [9].
Treatment
Children with mild-to-moderate exacerbations can be treated in the outpatient setting. The first step is to give them 4–8 puffs of salbutamol through an MDI with spacer. Three such similar doses can be given at 20-min intervals. It is again important to note that compressor-driven nebulizers do not offer any advantage over MDI with spacer. However, if a child is hypoxic and oxygen is available, then an oxygen-driven nebulizer with salbutamol can be given. Paradoxical hypoxia with administration of SABA occurs due to V/Q mismatch but continuing the medication will correct it over time.
In children with mild-to-moderate exacerbations, oral prednisolone is initiated if there is no response to 2 to 3 doses of salbutamol. Initially given for 3 to 5 d, it can be extended after reviewing the child. Trials of oral dexamethasone for 1 to 2 d have been studied in an attempt to improve adherence (due to the less frequent regimen), and early studies have shown similar responses and relapse rates between dexamethasone and prednisolone [10]. Nebulized inhaled corticosteroids are being studied in acute asthma but are not recommended as either an additive or replacement to oral steroids at present. Combinations of nebulized ICS with salbutamol are not recommended.
In children with severe asthma exacerbations, a SABA is given as described above but arrangements for transfer to a hospital should be initiated early. It is vital that the child receives a SABA and systemic steroids prior to transfer. There is enough data to show that early introduction of steroids reduces the need for intensive care and reduces the length of stay in hospital. Similarly, children with mild-to-moderate exacerbation will also need to be transferred if they have not responded to SABA and oral steroids, or if they are persistently hypoxic. The exact timing of transfer of these children will also depend on the home medications that the child received. If the child has already received multiple doses of SABA at home, then early transfer is recommended.
Management of Acute Asthma in the Emergency Department
For the purposes of this review, only the management of moderate-to-severe acute exacerbations of asthma in the emergency department (ED) will be discussed, as the management of mild asthma will follow the same algorithm as detailed in Fig. 1.
Assessment
In the ED, a quick history (including risk factors as listed before) will be followed by a structured ABCDE (airway, breathing, circulation, disability, and exposure) approach. Based on the patient's clinical condition, a detailed history and examination can then be taken.
Children can be risk stratified using the scoring system as detailed earlier. However, in the emergency setting, moderate exacerbations may be quickly characterized by findings such as tachypnea, presence of an expiratory wheeze, significant use of accessory muscles, and oxygen saturations that are stable between 92 and 95%. Similarly, severe exacerbations are characterized by the inability to complete short sentences, presence of both an inspiratory and expiratory wheeze, and oxygen saturations that are typically less than 92%.
Treatment of Acute Moderate Asthma in the ED
Management follows a stepwise approach. Salbutamol is always the first choice of medication and given preferably using an MDI with spacer (as discussed previously). Children are given 4–8 puffs over three cycles in 20-min intervals over an hour. Nebulizers are used only if the child is hypoxic. Children are then reassessed and if required are given an additional cycle of salbutamol but this time with the addition of ipratropium. Systematic reviews have shown the benefit of using treatment with 2 to 3 doses of combined ipratropium and salbutamol in reducing hospital admissions and improving lung function in children with moderate-to-severe asthma exacerbations [11].
Systemic glucocorticoids also form the other mainstay of management of asthma exacerbations, and are given as soon as possible. These can be administered orally or parenterally (IV or IM). Oral prednisone is the preferred choice but if a child is not tolerating medications orally, then IV hydrocortisone or IV/IM dexamethasone may be considered.
Treatment of Patients Presenting with Severe Exacerbation of Asthma to ED
In the context of severe exacerbations, the stepwise approach is accelerated. Patients are generally given nebulized salbutamol, ipratropium, and early systemic steroids all together to try and prevent further worsening of the clinical status. Given that severe exacerbations generally mean that the child has reduced levels of oxygenation (< 92%), oxygen-driven nebulizers may be preferred over the use of MDI with spacer. The nebulizations are repeated every 20 min.
It is important to reassess patients after every step in the process. If there is an inadequate response to the treatment provided so far, an arterial blood gas may be performed. Hypoxia is seen in moderate-to-severe asthma. In early stages of acute asthma, arterial \({\mathrm{CO}}_{2}\)(\({\mathrm{PaCO}}_{2}\)) is low due to hyperventilation and this will rise progressively with increasing severity and respiratory failure. Hence, if a child presenting to ED has a normal \({\mathrm{PaCO}}_{2}\), it is already a red flag.
Intravenous magnesium sulphate can be started in the ED. It acts as a surrogate for calcium, causing smooth muscle relaxation and bronchodilation. It is inexpensive, has minimal adverse effects, and is readily available. Studies have consistently shown that the use of magnesium sulphate reduces hospital admissions, leads to shorter admission stays, and improves respiratory function [12]. Even though it is generally safe, patients need to be closely monitored for hypotension.
Failure to improve following the above actions, and children presenting with cyanosis, lethargy, inability to maintain respiratory effort, and altered mental status indicating impending respiratory failure should be transferred to PICU. Intubation and use of noninvasive ventilation (NIV) are usually initiated in PICU. However, if it is not possible to transfer the patient to PICU immediately, or there is an impending respiratory/cardiac arrest, intubation can be considered in the ED setting.
Children who (i) improve, (ii) are not hypoxic, and (iii) able to tolerate 3–4 hourly SABA can be discharged home with follow-up plans.
Management of Acute Asthma in Intensive Care
Some children with acute severe asthma still unfortunately need intensive care. Some of the risk factors for PICU admission are previous PICU admissions, need for mechanical ventilation, history of rapidly progressive episodes, history of uncontrolled asthma with poor compliance to controllers, and history of seizures during an acute asthma episode. Children with acute asthma who do not respond to standard therapy with medications are candidates to be transferred to PICU with a lower threshold kept for children with the risk factors mentioned above.
In many instances, PICU is more for intense cardiorespiratory monitoring when medications are escalated. A continuous monitoring of saturations, heart rate, respiratory rate, and blood pressure is advisable. If not already done, children with severe episodes will need arterial blood gas analysis to assess severity and prognosticate need for further invasive treatment. Regular monitoring of serum electrolytes and magnesium is also required.
SABAs are still the mainstay of treatment. Oxygen-driven nebulized salbutamol by the standard small volume nebulizer (SVN) is continued. The dose of 5 mg can be repeated back-to-back using SVN. When available, some units will use continuous nebulizations with large volume nebulizers which can run for an hour or more without refills. The only documented advantage of continuous nebulization is reduced requirement of manpower to refill the nebulizations. Although there is a theoretical advantage, use of levosalbutamol has not shown any significant advantage over normal racemic salbutamol [13]. Though it is not very evidence based, most units will also use ipratropium nebulizations 4 to 6 hourly [14]. Oxygen to maintain saturations above 92% is delivered by face mask or non-rebreather mask, if required. Steroids are given intravenously (IV) and methylprednisolone is preferred due to its decreased mineralocorticoid effect. However, hydrocortisone can be used as well. Intravenous (IV) magnesium sulphate (\({\mathrm{MgSO}}_{4}\)), if not already initiated has to be started and continued. Serum magnesium levels need to be intermittently monitored.
If a child has still not responded to management, then further escalation of medications has diminishing advantages. If the bronchospasm is very intense, preventing delivery of SABA to the peripheral airways, IV SABA (terbutaline or salbutamol) can be started [15]. There is evidence that this can decrease the number of intubations required [16]. However, arrhythmias, hypotension, and hypokalemia are complications that need to be monitored for.
Another medication that has been in use for acute asthma is IV aminophylline. Though its use has little evidence, it is used in many centers globally in a bid to avoid intubation when the patient is refractory to previous medications. It is not part of standard guidelines due to its narrow therapeutic index, unpleasant side-effects (vomiting and dysrhythmias), and requirement of serum level monitoring. Some of the other therapies tried but rarely used are nebulized MgSO4, heliox, and IV ketamine. Ketamine is the drug of choice for sedation during intubation. None of them are part of protocols though.
Noninvasive ventilation (NIV) in the forms of continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP) are being increasingly used in acute asthma. NIV decreases the work of breathing and can be used as a temporary measure to avoid intubation when the pharmacotherapy is yet to attain its maximum benefit [17]. It is used in children who have persistent hypoxia despite being on high-flow oxygen with/without hypercarbia and in children with increased work of breathing (WOB), and those who are tiring out. Children need to be awake, cooperative, and must have spontaneous respiration to be benefitted. While it is known that clinical scores improve with NIV, the evidence for NIV in asthma is still building. While it is good to start with CPAP in children with just hypoxia, BiPAP can be used in children with hypercarbia too. Pressures are started low and titrated up as tolerated. The main limitations of NIV are that it (i) requires patient cooperation, (ii) impairs clearing of airway secretions, (iii) causes gastric distention and breathing limitation, (iv) can delay intubation which can prove harmful, and (v) needs an experienced nurse or therapist to initiate and monitor.
High-flow nasal cannula (HFNC) oxygen is being increasingly used in PICU instead of NIV. While the feasibility and safety of HFNC has been demonstrated, its efficacy is still being studied. Early studies have shown it can delay initiation of NIV and impede delivery of aerosolized medications [18].
The step to mechanically ventilate children with asthma is fraught with difficulties and must be taken only after careful consideration of the indications, facilities, and the manpower experience available. The absolute indications are for those who have a respiratory arrest, cardiac arrest, or coma. The rest are relative indications based on clinical judgement and expertise available. These are (i) refractory hypoxemia in spite of high FiO2 or NIV, (ii) significant respiratory acidosis refractory to maximal therapy, (iii) severe WOB with tiring, and (iv) altered sensorium [19]. Intubation should be performed by the most experienced person available. Pneumothorax, pneumomediastinum, and hypotension are commonly encountered complications soon after. There is no consensus on the mode of ventilation preferred after intubation. The pressure control mode and pressure-limited volume guarantee modes are generally used. Goals of ventilation include maintaining adequate oxygenation, accepting permissive hypercapnia (respiratory acidosis) if pH > 7.2. Using slow rates and prolonged expiratory times minimizes air trapping [19]. The level of peak end expiratory pressure (PEEP) used is controversial. Generation of auto-PEEP by patients and eventual air leak syndromes occur. Traditionally, a low PEEP is preferred but alternatively using higher PEEP just below the level of auto-PEEP can lead to a reduced WOB in the child [1].
Principles of Tapering of Medications
There is sparce information on this. In the PICU setting, the underpinning principle is “the last medication started will be the first to be stopped.” Hence, IV salbutamol is to be tapered before IV magnesium, etc. The nebulized SABA and steroids will be the last to taper. The SABA can be gradually reduced from hourly to four-hourly and then to PRN [(pro re nata)—when necessary]. Steroids are given for prolonged periods for moderate-and-severe episodes. No tapering of oral steroids is required if they are given for less than 14 d. A summary of the commonly used medications and their doses/regimens is provided in Table 2 [20].
Conclusion
Using the above approaches to manage asthma exacerbations in a stepwise and aggressive manner will reduce progression of disease and lead to good results. Whilst asthma exacerbations are viewed as minor inconveniences, it is now known that they are strong prognostic factors for increased morbidity and mortality in childhood asthma. Therefore, an attitude of ZERO TOLERANCE towards occurrence of acute asthma exacerbations needs to be developed [21].
References
Pardue Jones B, Fleming GM, Otillio JK, Asokan I, Arnold DH. Pediatric acute asthma exacerbations: Evaluation and management from emergency department to intensive care unit. J Asthma. 2016;53:607–17.
Kumar P, Ram U. Patterns, factors associated and morbidity burden of asthma in India. PLoS One. 2017;12:e0185938.
O'Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW. START Investigators Group. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009;179:19–24.
Global Initiative For Asthma. GINA Report, Glob Strat Asthma Manag Prevention. 2021. Available at: https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf. Accessed on 20 July 2021.
Moriates C, Feldman L. Nebulized bronchodilators instead of metered-dose inhalers for obstructive pulmonary symptoms. J Hosp Med. 2015;10:691–3.
Sears MR, Rea HH, Fenwick J, Gillies AJ, Holst PE, O’Donnell TV, Rothwell RP. 75 deaths in asthmatics prescribed home nebulisers. Br Med J (Clin Res Ed). 1987;294:477–80.
Jackson DJ, Bacharier LB, Mauger DT, et al. Quintupling inhaled glucocorticoids to prevent childhood asthma exacerbations. N Engl J Med. 2018;378:891–901.
Gregory S, Kenan H. Acute asthma exacerbations in children younger than 12 years: Overview of home/office management and severity assessment. In: UpToDate. 2021. Available at: https://www.uptodate.com/contents/acute–asthma–exacerbations–in–children–younger–than–12–years–emergency–department–management#H43. Accessed on 5 July 2021.
Qureshi F, Pestian J, Davis P, Zaritsky A. Effect of nebulized ipratropium on the hospitalization rates of children with asthma. N Engl J Med. 1998;339:1030–5.
Wei J, Lu Y, Han F, Zhang J, Liu L, Chen Q. Oral dexamethasone vs. oral prednisone for children with acute asthma exacerbations: a systematic review and meta-analysis. Front Pediatr. 2019;7:503.
Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Paediatr Respir Rev. 2013;14:234–5.
Shan Z, Rong Y, Yang W, et al. Intravenous and nebulized magnesium sulfate for treating acute asthma in adults and children: a systematic review and meta-analysis. Respir Med. 2013;107:321–30.
Qureshi F, Zaritsky A, Welch C, Meadows T, Burke BL. Clinical efficacy of racemic albuterol versus levalbuterol for the treatment of acute pediatric asthma. Ann Emerg Med. 2005;46:29–36.
Wade A, Chang C. Evaluation and treatment of critical asthma syndrome in children. Clin Rev Allergy Immunol. 2015;48:66–83.
Wong JJ, Lee JH, Turner DA, Rehder KJ. A review of the use of adjunctive therapies in severe acute asthma exacerbation in critically ill children. Expert Rev Respir Med. 2014;8:423–41.
Doymaz S, Schneider J, Sagy M. Early administration of terbutaline in severe pediatric asthma may reduce incidence of acute respiratory failure. Ann Allergy Asthma Immunol. 2014;112:207–10.
Howell JD. Acute severe asthma exacerbations in children younger than 12 years : Intensive care unit management. UptoDate. 2021. Available at: https://www.uptodate.com/contents/acute-severe-asthma-exacerbations-in-children-younger-than-12-yearsintensive-care-unit-management. Accessed on 24 July 2021.
Chao KY, Chien YH, Mu SC. High-flow nasal cannula in children with asthma exacerbation: A review of current evidence. Paediatr Respir Rev. 2021;40:52–7.
Kline-Krammes S, Patel NH, Robinson S. Childhood asthma: a guide for pediatric emergency medicine providers. Emerg Med Clin North Am. 2013;31:705–32.
Leung JS. Paediatrics: how to manage acute asthma exacerbations. Drugs in Context. 2021;10. https://doi.org/10.7573/dic.2020-12-7
Saglani S, Fleming L, Sonnappa S, Bush A. Advances in the aetiology, management, and prevention of acute asthma attacks in children. Lancet Child Adolesc Health. 2019;3:354–64.
Author information
Authors and Affiliations
Contributions
SM: Manuscript writing and editing; MBR: Overall concept, manuscript writing, and editing. MBR will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahesh, S., Ramamurthy, M.B. Management of Acute Asthma in Children. Indian J Pediatr 89, 366–372 (2022). https://doi.org/10.1007/s12098-021-04051-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-021-04051-6