Abstract
Hyperbilirubinemia is a common occurrence in neonates; it may be physiological or pathological. Conjugated hyperbilirubinemia may result from medical or surgical causes, and can result in irreversible liver damage if untreated. The aim of imaging is the timely diagnosis of surgical conditions like biliary atresia and choledochal cysts. Abdominal ultrasound is the first line imaging modality, and Magnetic resonance cholangiopancreatography (MRCP) also has a role, especially in pre-operative assessment of choledochal cysts (CDCs). For biliary atresia, the triangular cord sign and gallbladder abnormalities are the two most useful ultrasound features, with a combined sensitivity of 95%. Liver biopsy has an important role in pre-operative evaluation; however, the gold standard for diagnosis of biliary atresia remains an intra-operative cholangiogram. Choledochal cysts are classified into types according to the number, location, extent and morphology of the areas of cystic dilatation. They are often associated with an abnormal pancreaticobiliary junction, which is best assessed on MRCP. Caroli’s disease or type 5 CDC comprises of multiple intrahepatic cysts. CDCs, though benign, require surgery as they may be associated with complications like cholelithiasis, cholangitis and development of malignancy. Severe unconjugated hyperbilirubinemia puts neonates at high risk of developing bilirubin induced brain injury, which may be acute or chronic. Magnetic resonance imaging of the brain is the preferred modality for evaluation, and shows characteristic involvement of the globus pallidi, subthalamic nuclei and cerebellum – in acute cases, these areas show T1 hyperintensity, while chronic cases typically show hyperintensity on T2 weighted images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unconjugated hyperbilirubinemia is a common occurrence in neonates; it is most often physiological or due to breast-milk jaundice (a benign entity). However, neonatal jaundice that results from underlying cholestasis (with resultant conjugated hyperbilirubinemia) is always pathological and needs prompt evaluation. In underdeveloped countries, the burden of severe neonatal jaundice is relatively high, and these neonates are at risk of developing bilirubin induced brain injury.
Neonatal cholestasis (NCS) may result from surgical or medical causes. The most important causes in India are biliary atresia (which constitutes approximately one-third of cases), idiopathic neonatal hepatitis (NH), infections like urinary tract infections/ sepsis and congenital infections, metabolic causes like tyrosinemia, galactosemia and alpha-1 antitrypsin deficiency, and choledochal cysts including Caroli’s disease [1,2,3]. Other causes include paucity of interlobular bile ducts and progressive familial intrahepatic cholestasis.
Conjugated hyperbilirubinemia is defined as serum direct/ conjugated bilirubin level of more than 1.0 mg/dl for a total serum bilirubin (TSB) of upto 5 mg/dl, and more than 20% of the TSB when the TSB is >5 mg/dL [1]. Joint recommendation guidelines by the North American and European Societies for Pediatric Gastroenterology, Hepatology and Nutrition for the evaluation of cholestatic jaundice in infants [4] state that in any neonate with jaundice present after the age of 14 d, the minimum evaluation includes a full history, clinical examination, evaluation of stool color and a fractionated bilirubin measurement. In neonatal cholestasis, the consensus statement of the Pediatric Gastroenterology chapter of Indian Academy of Pediatrics [1] recommends a complete liver function test, thyroid function test and a sepsis screen followed by specific radiological and histopathological tests.
NCS, if persistent and untreated, invariably leads to irreversible liver damage and chronic liver disease. Patients should be referred to a tertiary-care centre and evaluated in a timely fashion. Late referral of these patients is a major problem [1, 5]; we need to increase awareness among clinicians, nursing and other healthcare personnel. The aim of evaluation is to diagnose surgical causes and treatable medical causes.
Biliary Atresia
Biliary atresia (BA) is the most common surgical cause of neonatal cholestasis, and early diagnosis of this severe and progressive cholangiopathy is critical for its successful management. The initial surgical management of these cases is by Kasai’s portoenterostomy (PE), which is best performed in children less than 3 mo of age. The outcome of surgery becomes significantly worse with increasing age of the child [6].
The pathogenesis of BA is complex and incompletely understood [7]; theories include genetic predisposition, viral or toxin-mediated injury. The most common form is the non-syndromic form; but syndromic forms may occur associated with other malformations (like asplenia, polysplenia, preduodenal portal vein, interrupted inferior vena cava) and laterality defects (e.g., situs inversus).
The Kasai classification system divides biliary atresia into three types depending on whether involvement is of the common bile duct (CBD)- type I, common hepatic duct (CHD)- without or with CBD/ cystic duct –types IIa and IIb, respectively, and the most common form– type III - involvement of extrahepatic bile ducts along with intrahepatic ducts till the level of porta hepatis. The findings on imaging reflect the level(s) of involvement.
Abdominal ultrasound (US) is the first-line imaging technique given its safety, easy availability, short scan times, high resolution images (using high frequency linear transducers) and no need for sedation in small children.
According to a recent meta-analysis [8] which studied the accuracy of various ultrasound findings in the diagnosis of BA, the triangular cord sign and gallbladder abnormalities (Figs. 1 and 2) are the two most useful features, with a combined sensitivity of 95%. The triangular cord (TC) sign [9, 10] refers to the visualisation of an echogenic ‘cord-like’ structure at the porta hepatis, which is thought to represent the fibrous ductal remnants. A positive TC is taken as a measurement of the echogenic anterior wall of the right portal vein (EARPV) of more than 4 mm on a longitudinal scan [10]. Modifications of technique have been described [11]; a positive TC has the highest specificity among US findings in BA (upto 97%), though its sensitivity is relatively low at approximately 74% [8, 12].
Ultrasound findings suggestive of Biliary atresia (different patients): High resolution ultrasound images using a high frequency linear transducer show the gallbladder (GB) ghost triad (a- GB length 14 mm), positive triangular cord sign (b- the echogenic anterior wall of right portal vein is 5 mm when measured on this longitudinal image), dilated right hepatic artery (c), and a small GB pre-feed (d) not contracting significantly post feed (e)
Biliary atresia in a 2-mo-old female: Ultrasound showed a small, hyperechoic gallbladder (a), 12 mm in length, with a small lumen and irregular wall, a positive triangular cord sign (b) measuring 5 mm, increased subcapsular blood flow on colour doppler (c) and enlarged hepatic artery – 3 mm (d) . HIDA scan (e) showed no excretion into the bowel even on delayed phase. Liver biopsy (f) showed bile duct proliferation. Biliary atresia was confirmed on intra-operative cholangiogram and Kasai’s procedure performed
In cases of BA, the gallbladder (GB) is often small or absent. A ‘pseudo-gallbladder’ or gallbladder ‘ghost triad’ [13, 14] has been described, which refers to a GB of reduced length (<1.9 cm or 1.5 cm in different studies), with an irregular contour and lack of a normal mucosal lining. The absence of GB is highly specific for diagnosing BA [8]. It is important to keep the child fasting, ideally for 4 h, before US evaluation. GB contractility has also been evaluated in neonates [15] and for differentiating BA from non-BA causes of NCS [16], and lack of normal post-feed GB contraction supports a diagnosis of BA. Other US findings that suggest BA are enlarged right hepatic artery [17] – more than 1.5 mm, ratio of hepatic artery to portal vein diameter of >0.45, presence of hepatic subcapsular blood flow [18] (Fig. 2), and visualization of a porta hepatis microcyst [19]. Secondary changes may be seen due to associated liver disease – splenomegaly, liver enlargement etc.
Table 1 summarizes the US findings suggestive of BA.
Magnetic resonance cholangiopancreatography (MRCP) is best reserved as a problem-solving modality, due to its high cost and need for sedation. Various studies [20,21,22,23] have reported sensitivities and specificities as high as 99% and 95%, respectively. The visualization of the right and left hepatic ducts, along with CHD and CBD in their entirety, may help exclude BA as a diagnostic consideration. However, false positives and false negatives do occur. GB abnormalities and MR-Triangular cord thickness (MR-TCT: maximum diameter of periportal signal change on MRI) have been described, and the combination of US and MRCP may be useful in problem cases as it results in better diagnostic performance [22] .
Hepatobiliary scintigraphy or Hepatobiliary iminodiacetic acid scan (HIDA scan) has been used to differentiate BA from other causes of NCS. Though excretion of tracer into the bowel is helpful to exclude BA; the absence of tracer excretion in non-specific, and limits the usefulness of the scan. The administration of phenobarbital for 3–5 d before hand enhances biliary excretion of the isotope, at the expense of time delay.
Liver biopsy, interpreted by an experienced pathologist, has an important role in the pre-operative diagnosis of BA [1, 3, 4]. Ductular proliferation, bile duct and ductular bile plugs and portal fibrosis are useful in distinguishing BA from NH. When interpreted in conjunction with the clinical and imaging findings, liver biopsy has been reported to have a sensitivity of 89–99%, specificity of 82–98% and accuracy of upto 95% in the diagnosis of BA.
It is important to remember that no single technique can enable a definitive pre-operative diagnosis of BA; rather, a combination of findings is used to suspect it. The gold standard for diagnosis of BA remains an intra-operative cholangiogram.
Cystic Biliary Atresia
Cystic biliary atresia (CBA) is a distinct, and relatively uncommon subtype of BA [7, 24]. It assumes great significance because it can easily mimic a choledochal cyst (CDC) on imaging; whereas the surgical approach and management of the two entities, as well as the long term prognosis, is very different. Patients with CBA require a Kasai’s PE, rather than a cyst excision (as for CDC); and need to be operated early to prevent liver damage.
Some sonographic features that point towards a diagnosis of CBA, in a patient with a cyst at the porta, include absence of intrahepatic ductal dilatation and presence of BA features like TC sign or GB abnormality (Fig. 3). Sludge/ calculi within the cyst are more often seen in cases with CDC [25].
Cystic biliary atresia in a 3-mo-old female: Ultrasound abdomen revealed a small gallbladder (a) and a positive triangular cord (b), suggesting biliary atresia. In addition, a heterogeneously hypoechoic lesion was seen at the porta (c). Axial MRI- single-shot T2 weighted (HASTE) images confirmed a cystic structure at porta (d). CHD at the porta was not seen on MRI, the lower CBD could be traced on the axial MRI images (arrows in e,f). HIDA scan showed no excretion into the bowel. Liver biopsy (g) was also suggestive of biliary atresia. However, child expired before surgery
Neonatal Hepatitis
Non-surgical causes of NCS include idiopathic neonatal hepatitis (INH), which constitutes almost one-third of cases in India [1]. INH is actually a diagnosis of exclusion, after work-up for metabolic and infective causes turns out negative. On imaging, these cases will show a normal GB length, morphology and post-feed contraction, and absence of other features which suggest BA (Fig. 4). Some cases may show GB wall thickening, or periportal edema. A HIDA scan that shows excretion of tracer into bowel is helpful, as it virtually excludes BA. However, cases with severe NH may also fail to show excretion into the bowel.
Neonatal hepatitis in a 1-mo-male: Ultrasound showed a normal gallbladder length (a) of more than 19 mm, with normal contraction post feeding. Triangular cord sign was negative (b), and hepatic artery was not dilated- measured 1 mm (c). HIDA scan showed excretion into the bowel on the 4-h image (d). Patient responded to conservative management
Neonatal hepatitis may also be associated with underlying infection, notably congenital infections like cytomegalovirus (CMV), toxoplasmosis, rubella, syphilis and herpes virus.
Alagille Syndrome
Alagille syndrome (AS) is a multisystem disorder which is an important familial cause of NCS. Affected individuals show paucity of interlobular bile ducts (PILBD), typical facies, along with cardiac, ocular and skeletal abnormalities. Certain imaging findings may overlap with cases of BA– for instance, patients with AS may show a small GB on ultrasound or non-visualization of the extrahepatic biliary tree on MRCP [26]. However, findings like TC sign and enlarged hepatic artery are not usually seen in AS. Accurate differentiation from BA is important as management differs – Kasai’s PE does not benefit cases of AS; and may, in fact, cause worsening. Many cases can be managed conservatively, or may need liver transplant.
PILBD may also occur in isolation in patients, without the syndromic association with AS.
Choledochal Cysts
Choledochal cysts (CDC) are congenital disorders presenting with cystic dilation of the biliary tract; the exact cause is not known. One hypothesis is that CDCs arise due to duct plate malformations, which is generally used to explain the pathogenesis of Caroli’s disease. Another hypothesis is based on the digestive effect of the pancreatic juice refluxing into the biliary tract because of the abnormal pancreaticobiliary junction (APBJ) – the incidence of APBJ in CDCs is upto 96% [27, 28]. Presence of strictures in the distal CBD has also been proposed as a cause of CDC.
CDCs are more common in female children and prevalent in Asian countries. Though benign, they can lead to multiple complications such as cholangitis, cholelithiasis, malignant transformation etc. On imaging, it may be challenging to differentiate them from cystic variety of biliary atresia.
Imaging Modalities
US is the first line investigation due to its lack of radiation, high resolution images, wide availability and portability. It enables diagnosis and also detects sludge or calculi, wall thickening, nodularity or mass lesions. However, it may not depict the entire anatomy of the biliary system, which is important to classify the type of CDC. Also, US is generally incapable of demonstrating the pancreaticobiliary junction and the status of the main pancreatic duct and pancreatic parenchyma. CT scan is generally not employed because of its poor contrast resolution and radiation exposure.
MRI is the modality of choice for the evaluation of CDC. MRCP can provide excellent depiction of the entire biliary tract including the pancreaticobiliary junction, and can detect complications. Optionally, MRI contrasts such as Gd-BOPTA and Gd-EOB-DTPA- which get excreted into the biliary tract- can be used to demonstrate the biliary communication of the cystic structures. This is particularly valuable in Caroli’s disease and to differentiate CDC from cystic biliary atresia. The presence of sludge and the excretion of contrast into the cystic structure practically rules out the diagnosis of CBA. The role of HIDA scan is limited in the context of CDC.
Classification
Since the first classification system for CDC proposed by Alonso-Lej in 1959, there have been revisions proposed by Todani et al. in 1977 and 1997 [29,30,31]. The most widely used classification system is the one proposed by Todani et al. It includes 5 main types, along with subtypes. Recently, a rare type of isolated dilatation of cystic duct has also been included in the classification of CDC as type 6. On imaging, the typical appearance of CDC is disproportionate dilatation of extrahepatic biliary tree of varying lengths with minimal or no dilatation of intrahepatic biliary tree. This is unlike biliary dilatation due to obstructive causes, in which the dilatation is usually proportionate. Even in types where there is intrahepatic involvement, the dilatation is usually cystic or saccular as opposed to tubular dilatation which is seen in obstructive causes.
Type 1 Choledochal Cyst
They are the most common type constituting upto 90% of CDC. There are three subtypes described, based on the morphology of the dilatation and the length of involvement. The characteristic feature of this type is single or focal extrahepatic cyst. Type 1A shows cystic dilatation (Fig. 5), 1B shows segmental dilatation and 1C shows fusiform dilatation (Fig. 6). Usually, the intrahepatic biliary tree remains normal in type 1, except in type 1C where the dilatation can extend into the intrahepatic part which is because of increase in pressure. Hence, type 1C can mimic obstructive dilatation and even type 4A CDC. Features such as saccular dilatation of the intrahepatic part of biliary tree and narrowing at the hilar region are usually seen in type 4A, whereas the intrahepatic dilatation in type 1C is seen in continuity with the extrahepatic dilatation without any narrowing in between.
Type 2 Choledochal Cyst
Type 2 cases are rare and constitute only 3% of all CDC [32]. They are seen as outpouchings from the extrahepatic biliary tree, and are not associated with APBJ. It is not always possible to show the communication between the diverticulum and biliary tree on imaging. Hence, type 2 CDC can mimic cystic variety of biliary atresia. However, presence of other tell-tale signs of biliary atresia (triangular cord sign, abnormal gallbladder etc) should go against the diagnosis of type 2 CDC.
Type 3 Choledochal Cyst
Type 3 CDC is due to dilatation of intraduodenal part of bile duct, also known as choledochocele. These cases constitute only upto 5% of all CDCs, and are not associated with APBJ [32]. Based on the size of the cyst, treatment can be either by endoscopic retrograde cholangiopancreatography (ERCP) guided sphincterotomy or sphincteroplasty.
Type 4 Choledochal Cyst
Type 4 CDCs constitute upto 40% of all cases– the second most common type of CDC. There are two subtypes, namely type 4A, which forms the majority of type 4 cases (Fig. 7) and is characterised by multiple cysts involving both the intra and extrahepatic biliary tree with associated APBJ; and type 4B- multiple cysts in extrahepatic bile duct, which is rare. As discussed before, the appearance of type 4A cysts can be very similar to type 1C. Hilar narrowing is frequently seen with type 4A, and can be used to differentiate these two entities.
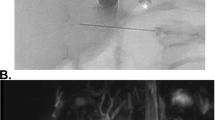
T2 weighted MRI images showing dilatation of CBD along with multiple saccular dilatations of intrahepatic biliary tract. There is also abrupt change in caliber between the dilated part and the peripheral normal intrahepatic biliary tract (arrow). These features are characteristic of type 4A choledochal cyst
Type 5 Choledochal Cyst
Type 5 CDC or Caroli’s disease is an uncommon type of CDC characterised by multiple intrahepatic cysts (Fig. 8). About 50% of patients have associated hepatic fibrosis- these constitute Caroli’s syndrome. Both these entities belong to a spectrum of developmental biliary disorders called ductal plate malformations. Involvement of larger bile ducts results in Caroli’s disease, and involvement of smaller peripheral bile ducts can result in peribiliary cysts, biliary hamartomas or hepatic fibrosis, depending on the site of involvement. On imaging, Caroli’s disease can mimic hepatic cysts. Presence of intraluminal portal vein sign/central dot sign (ectatic ducts surrounding portal vein radicles) and characteristic distribution help in diagnosing Caroli’s disease. ERCP or MRCP with hepatobiliary contrast agents can demonstrate the communication of cysts with biliary tree, supporting the diagnosis. Rarely, the involvement can be limited to one lobe or even segment. It can be associated with other disorders such as cystic renal diseases and medullary sponge kidney. Because of long standing biliary stasis, complications such as cholangitis, stone formation or malignant transformation can occur.
T2 weighted MRI images showing multiple focal dilatations (arrow) of the intrahepatic biliary tract of both the lobes of liver with some of them showing debris level within. The CBD is not dilated and the background liver parenchyma is normal. These features are suggestive of Caroli’s disease or type 5 choledochal cyst
Type 6 Choledochal Cyst
This is a relatively new and extremely rare entity, which was not a part of Todani’s classification. It is characterised by the isolated involvement of cystic duct. Only a few case reports have been published.
Table 2 summarizes the classification of CDCs.
Complications
Choledochal cysts are benign, however can lead to potentially fatal complications, which necessitate surgical resection of the cysts. Complications range from cholangitis, stone formation, development of malignancy and pancreatitis. CDC types 4A and 5, in long standing cases, can lead to cirrhosis. Development of malignancy in CDC is a dreaded complication which can occur in 10 to 30% of patients [33,34,35]. It is more commonly seen with types 1, 4A and 5; cholangiocarcinoma is the most common type of malignancy. Close follow-up is necessary in patients with CDC because of their susceptibility to develop malignancy even after resection of the cysts [36].
Bilirubin Induced Brain Injury
Circulating high levels of unconjugated bilirubin can lead to serious brain damage with persistent disabilities and even mortality. Thirteen percent of cases of neonatal hyperbilirubinemia are at risk of development of kernicterus [37]; however with improved perinatal care, the incidence is decreasing. Preterms are more susceptible to bilirubin injury as compared to term infants [38].
Bilirubin induced brain injury is predominantly of two forms, acute or chronic bilirubin encephalopathy; chronic bilirubin encephalopathy is also termed as kernicterus. A third form of bilirubin-induced neurologic dysfunction (BIND) is also evolving as a clinical entity synonymous with subtle kernicterus and no specific MRI findings are described for the same [39].
The pathogenesis of brain damage by bilirubin is complex. It is the free, unbound circulating bilirubin, not bound to albumin, which can exit into the extravascular spaces of the brain and cause neurotoxicity. However, no definite threshold levels are established and actual neurotoxicity would depend on several factors such as duration of exposure of brain tissues to unbound bilirubin, predisposition of developing brain, bilirubin oxidation within the CNS, gestational age and birth weight [40]. Since laboratory techniques for measuring actual unbound bilirubin are not readily available, surrogate markers such as total serum bilirubin levels and total serum bilirubin to serum albumin ratios are commonly used to guide the management.
Imaging Findings
MRI is the modality of choice to evaluate the brain parenchymal changes due to bilirubin toxicity. The MRI protocol should include T1, T2 and diffusion weighted sequences in multiple planes (axial, coronal and sagittal). T2* weighted imaging and MR spectroscopy are additional sequences which are routinely performed in cases of neonatal encephalopathy [41].
Most common sites depicting signal abnormalities include posteromedial borders of globus pallidi. Other sites less frequently involved are subthalamic nuclei, hippocampus, putamen, cranial nerve nuclei and cerebellum (cortex and dentate nuclei). Thalami are typically spared which helps to distinguish from other metabolic and ischemic disorders.
In acute forms, the neurological manifestations occur within 2–5 d of age with severe hyperbilirubinemia and can present in initial, intermediate or advanced phases. In initial phase, neonate presents with lethargy, poor sucking and hypotonia which progresses to hypertonia, opistotonus, recurrent apnea, fever and high pitched cry in advanced phase. On MRI performed in first few days or weeks of acute encephalopathy, the signal intensity of globus pallidi and subthalamic nuclei is hyperintense on T1, and iso-to-hyperintense on T2 weighted images (Fig. 9). These areas do not show diffusion restriction. Signal abnormalities are bilateral and symmetric. MR spectroscopy studies have revealed increased levels of glutamine and glutamate along with decreased levels of choline and N-acetyl-aspartate [42, 43] .
Acute bilirubin encephalopathy. MRI brain, T1 weighted images (a, b, c) show bilateral symmetric, hyperintense signal in globus pallid (white arrows), subthalamic nuclei (black arrows) and brainstem (thin arrows) . T2 weighted image (d) show hyperintensity in bilateral globus pallidi (arrows). DWI at b-1000 (e) and corresponding ADC image (f), show no areas of diffusion restriction
Chronic form is characterised by permanent neurological sequelae which manifest in first year of life with hearing loss, upward gaze pareses and movement disorders of dystonia or choreoathetosis. Dental enamel dysplasia is frequently associated. On MRI, the globus pallidi and subthalamic nuclei show uniform, symmetric T2 hyperintense signal (Fig. 10).
Use of other imaging modalities such as single-photon emission computed tomography (SPECT) and cranial ultrasound have been reported, however no definite specific imaging features are described to be characteristic of kernicterus. In older children who had neonatal kernicterus with MRI signal abnormalities, SPECT revealed areas of decreased blood flow to basal ganglia regions [44]. Cranial USG findings described are increased basal ganglia and white matter echogenicity, lenticulostriate vasculopathy (LSV) and caudothalamic hyperechogencity/cysts [45].
Bilirubin induced brain injury is preventable, and management of neonatal hyperbilirubinemia using appropriate phototherapy and exchange transfusions have significantly decreased the prevalence of kernicterus.
References
Bhatia V, Bavdekar A, Matthai J, Waikar Y, Sibal A. Management of neonatal cholestasis: consensus statement of the pediatric gastroenterology chapter of Indian academy of pediatrics. Indian Pediatr. 2014;51:203–10.
Poddar U, Thapa BR, Das A, Bhattacharya A, Rao KLN, Singh K. Neonatal cholestasis: differentiation of biliary atresia from neonatal hepatitis in a developing country. Acta Paediatr. 2009;98:1260–64.
Rastogi A, Krishnani N, Yachha SK, Khanna V, Poddar U, Lal R. Histopathological features and accuracy for diagnosing biliary atresia by prelaparotomy liver biopsy in developing countries. J Gastroenterol Hepatol. 2009;24:97–102.
Fawaz R, Baumann U, Ekong U, et al. Guideline for the evaluation of cholestatic jaundice in infants: joint recommendations of the north American Society for Pediatric Gastroenterology, hepatology, and nutrition and the European Society for Pediatric Gastroenterology, hepatology, and nutrition. J Pediatr Gastroenterol Nutr. 2017;64:154–68.
De Bruyne R, Van Biervliet S, Vande Velde S, Van Winckel M. Clinical practice: neonatal cholestasis. Eur J Pediatr. 2011;170:279–84.
Serinet M-O, Wildhaber BE, Broué P, et al. Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics. 2009;123:1280–6.
Asai A, Miethke A, Bezerra JA. Pathogenesis of biliary atresia: defining biology to understand clinical phenotypes. Nat Rev Gastroenterol Hepatol. 2015;12:342–52.
Zhou L, Shan Q, Tian W, Wang Z, Liang J, Xie X. Ultrasound for the diagnosis of biliary atresia: a meta-analysis. Am J Roentgenol. 2016;206:W73–82.
Choi SO, Park WH, Lee HJ, Woo SK. “Triangular cord”: a sonographic finding applicable in the diagnosis of biliary atresia. J Pediatr Surg. 1996;31:363–6.
Lee H-J, Lee S-M, Park W-H, Choi S-O. Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology. 2003;229:395–400.
Zhou L-Y, Wang W, Shan Q, et al. Optimizing the US diagnosis of biliary atresia with a modified triangular cord thickness and gallbladder classification. Radiology. 2015;277:181–91.
Humphrey TM, Stringer MD. Biliary atresia: US diagnosis. Radiology. 2007;244:845–51.
Aziz S, Wild Y, Rosenthal P, Goldstein RB. Pseudo gallbladder sign in biliary atresia—an imaging pitfall. Pediatr Radiol. 2011;41:620–6.
Tan Kendrick APA, Phua KB, Ooi BC, Tan CEL. Biliary atresia: making the diagnosis by the gallbladder ghost triad. Pediatr Radiol. 2003;33:311–5.
Jawaheer G, Pierro A, Lloyd DA, Shaw NJ. Gall bladder contractility in neonates: effects of parenteral and enteral feeding. Arch Dis Child Fetal Neonatal Ed. 1995;72:F200–2.
Ikeda S, Sera Y, Akagi M. Serial ultrasonic examination to differentiate biliary atresia from neonatal hepatitis--special reference to changes in size of the gallbladder. Eur J Pediatr. 1989;148:396–400.
Kim WS, Cheon J-E, Youn BJ, et al. Hepatic arterial diameter measured with US: adjunct for US diagnosis of biliary atresia. Radiology. 2007;245:549–55.
Lee MS, Kim M-J, Lee M-J, et al. Biliary atresia: color doppler US findings in neonates and infants. Radiology. 2009;252:282–9.
Koob M, Pariente D, Habes D, Ducot B, Adamsbaum C, Franchi-Abella S. The porta hepatis microcyst: an additional sonographic sign for the diagnosis of biliary atresia. Eur Radiol. 2017;27:1812–21.
Norton KI, Glass RB, Kogan D, Lee JS, Emre S, Shneider BL. MR cholangiography in the evaluation of neonatal cholestasis: initial results. Radiology. 2002;222:687–91.
Kim YH, Kim M-J, Shin HJ, et al. MRI-based decision tree model for diagnosis of biliary atresia. Eur Radiol. 2018;28:3422–31.
Sung S, Jeon TY, Yoo S-Y, et al. Incremental value of MR cholangiopancreatography in diagnosis of biliary atresia. PLoS One. 2016;11:e0158132.
Liu B, Cai J, Xu Y, et al. Three-dimensional magnetic resonance cholangiopancreatography for the diagnosis of biliary atresia in infants and neonates. PLoS One. 2014;9:e88268.
Caponcelli E, Knisely AS, Davenport M. Cystic biliary atresia: an etiologic and prognostic subgroup. J Pediatr Surg. 2008;43:1619–24.
Zhou L-Y, Guan B-Y, Li L, et al. Objective differential characteristics of cystic biliary atresia and choledochal cysts in neonates and young infants. J Ultrasound Med. 2012;31:833–41.
Han S, Jeon TY, Hwang SM, et al. Imaging findings of Alagille syndrome in young infants: differentiation from biliary atresia. Br J Radiol. 2017;90:20170406.
Edil BH, Olino K, Cameron JL. The current management of choledochal cysts. Adv Surg. 2009;43:221–32.
Miyano T, Yamataka A. Choledochal cysts. Curr Opin Pediatr. 1997;9:283–8.
Alonso-Lej F, Rever WB, Pessagno DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg. 1959;108:1–30.
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9.
Todani T. Congenital choledochal dilatation: classification, clinical features, and long-term results. J Hepato-Biliary-Pancreat Surg. 1997;4:276–82.
Lewis VA, Adam SZ, Nikolaidis P, et al. Imaging of choledochal cysts. Abdom Imaging. 2015;40:1567–80.
Lee HK, Park SJ, Yi BH, Lee AL, Moon JH, Chang YW. Imaging features of adult choledochal cysts: a pictorial review. Korean J Radiol. 2009;10:71–80.
Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009;52:434–40.
Liu Q-Y, Lai D-M, Gao M, et al. MRI manifestations of adult choledochal cysts associated with biliary malignancy: a report of ten cases. Abdom Imaging. 2013;38:1061–70.
Ono S, Fumino S, Shimadera S, Iwai N. Long-term outcomes after hepaticojejunostomy for choledochal cyst: a 10- to 27-year follow-up. J Pediatr Surg. 2010;45:376–8.
Bhutani VK, Zipursky A, Blencowe H, et al. Neonatal hyperbilirubinemia and rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013;74:86–100.
Watchko JF. Bilirubin-induced neurotoxicity in the preterm neonate. Clin Perinatol. 2016;43:297–311.
Wisnowski JL, Panigrahy A, Painter MJ, Watchko JF. Magnetic resonance imaging of bilirubin encephalopathy: current limitations and future promise. Semin Perinatol. 2014;38:422–8.
Watchko JF, Tiribelli C. Bilirubin-induced neurologic damage--mechanisms and management approaches. N Engl J Med. 2013;369:2021–30.
Shroff MM, Soares-Fernandes JP, Whyte H, Raybaud C. MR imaging for diagnostic evaluation of encephalopathy in the newborn. Radiographics. 2010;30:763–80.
Sarı S, Yavuz A, Batur A, Bora A, Caksen H. Brain magnetic resonance imaging and magnetic resonance spectroscopy findings of children with kernicterus. Pol J Radiol. 2015;80:72–80.
Oakden WK, Moore AM, Blaser S, Noseworthy MD. 1H MR spectroscopic characteristics of kernicterus: a possible metabolic signature. Am J Neuroradiol. 2005;26:1571–4.
Okumura A, Hayakawa F, Maruyama K, Kubota T, Kato K, Watanabe K. Single photon emission computed tomography and serial MRI in preterm infants with kernicterus. Brain Dev. 2006;28:348–52.
Gkoltsiou K, Tzoufi M, Counsell S, Rutherford M, Cowan F. Serial brain MRI and ultrasound findings: relation to gestational age, bilirubin level, neonatal neurologic status and neurodevelopmental outcome in infants at risk of kernicterus. Early Hum Dev. 2008;84:829–38.
Acknowledgement
The authors acknowledge Dr. Rama Anand and Dr. Suvasini Sharma for help with the images.
Author information
Authors and Affiliations
Contributions
All three authors contributed to the Manuscript preparation and editing. Dr. Rama Anand, Director-Professor and HOD, Department of Radio-Diagnosis, Lady Hardinge Medical College will act as guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abbey, P., Kandasamy, D. & Naranje, P. Neonatal Jaundice. Indian J Pediatr 86, 830–841 (2019). https://doi.org/10.1007/s12098-019-02856-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-019-02856-0