Abstract
Objective
Avoidable hospitalization (AH) has been widely studied as a possible measure of primary health care performance. Since studies evaluating AH in migrant children, particularly in Europe, are lacking, the aim of this study was to investigate the role of maternal citizenship on the risk of AH in children.
Methods
The cohort study included all live newborns recorded in the Medical Birth Register (MBR) of Friuli-Venezia Giulia Region (Italy) in the years 1989–2012, followed from 30 d after their birth up to the 14th year of life. Cox regression models were used to estimate Hazard Ratios (HRs) for any AH and for specific conditions.
Results
Among the 213,635 children included in the cohort, authors identified 23,011 AHs in 16,744 children, most of which occurred between 1 and 4 y of age. Children born to mothers from High Migration Pressure Countries had a higher risk of AH for any condition (HR 1.35; 95% CI = 1.27–1.44) than children born to Italian mothers. The risks were higher concerning gastroenteritis (HR 1.74; 1.57–1.94), upper respiratory tract infections (HR 1.58; 1.35–1.84), asthma (HR 1.53; 1.12–2.06) and bacterial pneumonia (HR 1.18; 1.01–1.37). There were no differences in urinary tract infections, short term complications of diabetes and perforated appendix.
Conclusions
Despite the inclusiveness and universality of the Italian healthcare system, children born to immigrant mothers experienced more need of avoidable hospital care than children born to Italian mothers. Access barriers to primary care are plausible causes for the observed disparities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent decades, Italy, like other European Union countries, has experienced a dramatic increase in immigration, especially from low-income countries. At the beginning of 2016, there were 5,026,153 regular immigrants registered in Italy, accounting for 8.3% of the total resident population [1]. Therefore, monitoring health status of immigrants and their access to healthcare services is an important public health issue in European countries.
Migrants can face many barriers to their use of health services, which can hamper the patient’s access to the healthcare and/or lower its quality. These barriers may relate to patients’ characteristics, such as language or cultural issues (socio-economic status, beliefs, attitudes and practices regarding their personal health, perceived health) but may also depend on the healthcare service provided by the host country [2]. A plentiful literature about the unequal access to healthcare by migrants and by ethnic and linguistic minorities is available in long-standing host countries, such as the United States and Canada [3, 4]. On the other hand, information on the use of health services by migrants in most EU countries is limited [5]. A review of the European literature on utilization of healthcare services by migrants [6], found that overall migrants tend to have lower utilization of preventive care, more contacts per patient to general practitioner, and same or higher level of use of specialist care as compared to non-migrants. Hospitalization rates were higher than or equal to non-migrants, whereas results about emergency room access were inconclusive [6].
In Italy, primary health care (PHC) is the first point of contact with the National Healthcare System (NHS) for most people. It is mainly provided by general practitioners (GPs) and it brings health care as close as possible to where people live and work. Being free-access and responding to a vast variety of health needs, PHC can effectively prevent the need for emergency/inpatient care and ensures a reduction of health disparities within the population [7]. Thus, examining the access to PHC by vulnerable groups (such as the immigrant population) seems especially important. Hospitalization for Ambulatory Care Sensitive Conditions (ACSCs), thereafter called Avoidable Hospitalization (AH), has been used extensively as an indicator of the accessibility and overall effectiveness of PHC [8, 9]. ACSCs are defined as conditions for which “the provision of timely and effective outpatient care can help to reduce the risks of hospitalization by either preventing the onset of an illness or condition, controlling an acute episodic illness or condition, or managing a chronic disease or condition” [10].
Many studies have shown that AH rates can be influenced by several factors, most notably by socioeconomic variables. People with little formal education and low incomes are more likely to be hospitalized for an ACSC [10,11,12] as are residents of rural areas [12, 13] and people without medical insurance [14, 15]. A recent review on AH among migrants and ethnic minority groups [16] found that most ethnic minority groups in the US (Black/African Americans, Hispanic, others) and New Zealand (Maori, Pacific Islanders) had higher AH rates than White/European groups. It was also showed that almost no study considered migratory status as the exposure variable, none was set in Europe, and just a few studies adopted a longitudinal design. Finally, only a small fraction of studies included children in their study populations, showing similar results to those found in adults.
To the best of authors’ knowledge, no study has been conducted so far on the relationship between migratory status and AH in children in Europe, where accessibility to PHC should in principle be granted to everyone due to the universality and equity of the national health systems. Therefore, authors aimed to examine the extent to which maternal migratory status can influence the risk of AH in their children, using a large population-based birth cohort of children born in Friuli-Venezia Giulia Region (North-East Italy).
Material and Methods
This study was conducted in the Friuli-Venezia Giulia (FVG) region of north-eastern Italy. The region has a population of approximately 1.2 million and 10,000 births per year (Italian National Institute of Statistics, unpublished data (http://www.demo.istat.it)).
FVG is covered by a regional integrated healthcare system developed in the 1980s with the goal of automatically collecting and pooling data on healthcare funded by the National Health Service using a unique anonymous ID regional code.
The authors used a population-based birth cohort study design. The underlying study population consisted of all children born and resident in FVG in the period 1989–2012, identified using the regional Medical Birth Register (MBR) and followed up for a maximum of 14 y.
Three different data sources have been used in this study: 1) the MBR that contains socio-demographic data on the parents, and details of the pregnancy, labor, delivery and the newborn at birth; 2) the regional Hospital Discharge Records database, collecting data on inpatient care episodes occurring within or outside of the region, with up to 6 diagnostic codes from the International Classification of Diseases, Ninth Revision (ICD-9) (available from 1990 onward); 3) the cause of death register. The anonymous ID regional code allowed authors to cross-link the three data sources together at individual level.
For the purpose of this study, authors developed a definition of AH based on two previously published definitions: the one created by Agency for Healthcare Research and Quality, a US Federal Agency for Health Care System Improvement (AHRQ) as a list of Pediatric Quality Indicators [17], which is one of the most commonly adopted by recent works, besides the one developed by Pirani et al. [18], which is the only one used in an Italian setting. The definition of AH included the following eight groups of conditions identified using the diagnoses included in the regional Hospital Discharge Records database: 1) gastroenteritis; 2) diabetes short-term complications; 3) epileptic seizures and epilepsy; 4) ear and upper respiratory tract infections (URTIs); 5) bacterial pneumonia; 6) asthma; 7) perforated appendix; 8) urinary tract infections (UTIs). The complete list of the ICD-9 diagnosis included, and the associated age ranges restrictions, is reported in Table 1. The authors considered the eight groups of ACSCs and the overall measure of AH for each child.
Maternal citizenship information available on the MBR has been used as a proxy for migrant status. Completeness of MBR in providing data on maternal citizenship was almost 100%. For the purpose of the analysis, maternal citizenships were grouped into 3 different categories: 1) Italy; 2) Low Migratory Pressure Countries (LMPCs): not Central-Eastern Europe, North America, Oceania, Israel and Japan; 3) High Migratory Pressure Countries (HMPCs): Balkans and Eastern Europe, Central/South America, Africa and Asia (except for Israel and Japan). Mothers who were citizens of HMPCs are hereafter called “HMPC mothers”, and those who were citizens of LMPCs are hereafter called “LMPC mothers”.
Information was obtained from the MBR on all possible determinants, i.e. sex, birth order, number of older siblings (none or 1+), maternal age at child’s birth (< 25, 25–29, 30–34, 35–39, 40+), maternal education (lower than high school, high school, university), twin pregnancy (yes/no), gestational age (< 37wk, ≥ 37wk), pregnancy course (normal, pathological) and birth weight (< 2500, ≥ 2500).
Every child born in FVG between 01/01/1989 and 12/31/2012 has been enrolled in the cohort, with the exception of abortions, stillbirths, and early (within 30 d) neonatal deaths. Follow-up started at 30 d of age and ended with the earliest of the following events: emigration from FVG; death (retrieved from the cause of death register); turning 14 y old; end of the study period (12/31/2012); first AH (first hospitalization for any ACSC regarding the overall definition, and first hospitalization for each group of ACSC for each of the eight groups of ACSC conditions).
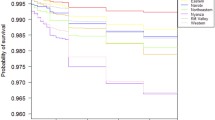
Cox proportional hazard models were used to measure the association between Maternal Citizenship and AHs. Italian citizenship was chosen as the reference group and compared to High and Low Migratory Pressure Countries. Model outputs included Hazard Ratios (HRs) with their 95% confidence intervals (CI) for AHs both as overall and for each group of conditions separately. All HRs were adjusted for sex and year of birth. In a distinct model, authors also adjusted for maternal education, which they used as a proxy of socioeconomic status (SES) [19]. Finally, in a third model, authors adjusted for the following perinatal covariates: maternal age, number of former deliveries, pregnancy course, twin pregnancy, birth weight and gestational age.
Results
The authors enrolled 214,845 newborns from the Friuli-Venezia Giulia region during the period 1989–2012. After exclusion of abortions, stillbirths, and early (within 30 d) neonatal deaths, 213,635 newborns were left in the birth cohort.
Table 2 shows the distribution of covariates used for the adjustments. Children born to Italian mothers were 191,345 (89.77%); those born to HMPC mothers were 20,441 (9.59%). Among the latter, those coming from Eastern Europe were the biggest subgroup (5.25%), followed by those coming from Africa (2.33%). Finally, children born to LMPC mothers were the remaining 1376 (0.65%). Maternal education was distributed as follows: 34,402 (16.28%) of the children had mothers with a university level, 100,384 (47.5%) with a high-school level, and 76,530 (36.22%) with a lower than high-school level. Maternal age was <25y for 22,859 (10.7%) children, 25–29 years for 60,733 (28.43%) children, 30–34 years for 78,159 (36.59%) children, 35–39 years for 43,130 (20.19%) children, and > 39 for 8754 (4.1%) children.
With a total of 1,902,041 person-years of follow-up, an overall number of 16,744 children with at least one AH were identified. Three thousand four hundred seventy children experienced at least one discharge for epileptic seizures and epilepsy, 4543 for gastroenteritis, 3248 for urinary tract infection (UTI), 2884 bacterial pneumonia, 2866 ear and upper respiratory tract infection (URTI), 724 asthma, 435 perforated appendix, and 580 diabetes short-term complications. More than a half of AHs (53.34%) regarded children aged 1–4 y, 29% in children aged 0–1 y, while 17.67% in children aged 5–14 y.
The main findings of our study are shown in Table 3. Children with an Italian mother accounted for a total of 1,770,796 person-years and experienced 15,397 AHs. Children with an HMPC mother accounted for a total 114,365 person-years and experienced 1235 AHs, while children with a LMPC mother experienced only 61 AH events. After adjusting for sex and year of birth, children with a HMPC mother were at higher risk of AH compared to children with an Italian mother [Hazard Ratio (HR) = 1.44, 95% CI: 1.36–1.54], while children with a LMPC mother had a lower risk (HR = 0.54, 95% CI: 0.42–0.69).
These results did not change significantly after adjusting for maternal education level (children with a HMPC mother: HR = 1.40, 95% CI: 1.32–1.49; children with a LMPC mother: HR = 0.57, 95% CI: 0.44–0.73), and perinatal covariates (children with a HMPC mother: HR = 1.35, 95% CI: 1.27–1.44; children with a LMPC mother: HR = 0.54, 95% CI: 0.42–0.70).
When examining results for specific groups of ACSCs, after adjusting for the full set of the above-mentioned covariates, children with a HMPC mother were at substantially higher risk of undergoing hospitalizations for gastroenteritis (HR = 1.74, 95% CI: 1.57–1.94), URTI (HR = 1.58, 95% CI: 1.35–1.84), bacterial pneumonia (HR = 1.18, 95% CI: 1.01–1.37) and asthma (HR = 1.53, 95% CI: 1.12–2.06), compared to children with an Italian mother. On the other hand, the risk of hospitalization for diabetes short-term complications, epilepsy, perforated appendix and UTI didn’t differ significantly in the two groups. The small number of AH events for children whose mother was a citizen of LMPCs did not allow to analyze specific groups of ACSCs in this group.
Discussion
To the best of authors’ knowledge, this is the first study conducted in Europe to examine the impact of migratory status on the risk of avoidable hospitalization among children. All children included in the present study were born and resident in Italy and were entitled to benefit from primary healthcare. However, children with an immigrant mother from HMPCs (who represent the vast majority of children with a foreign mother) were at higher risk of experiencing avoidable hospitalizations, compared to children with an Italian mother. The present results suggest that disadvantage related to migration in terms of the access to timely and effective PHC can be relevant even in countries with a universal healthcare coverage like Italy. On the other hand, authors found that children born to foreign mothers from high-income countries had a lower risk of undergoing AH compared to children whose mother was Italian. This could be explained by the fact that people coming from developed countries and choosing to settle down in Italy are comparatively healthier and/or benefit from a better familiar and social support, even in comparison with children born to Italian mothers, like previous researches have shown [20].
The present results were in line with previous studies on AH in children comparing different ethnic groups. Studies from the US [12, 21,22,23,24,25,26] and, to a lesser extent, from New Zealand [21, 27], found that ethnic minorities had generally higher overall AH rates than their White/European counterparts, although with variances when considering different ethnic groups. Almost all the studies from the US showed the highest AH rates for the Black race or African American ethnicity [12, 23, 24, 26, 28]. Hispanics too had higher AH rates than Whites/EU [22, 23, 28], while the Asian group had similar or lower rates than Europeans [28]. In New Zealand, both Maori and Pacific Islanders had higher AH rates than the majority group [21, 27]. Again, the Asian group experienced rates lower than or similar to the latter [21]. However, the existing literature investigates the role of “ethnicity”, a concept that cannot be considered a synonymous of migrant status in countries where migration is well established, like the US and New Zealand [29]. Furthermore, prior studies were mainly set in the US, a country that does not guarantee universal healthcare access, and healthcare coverage is, in general, lower than most of the European high-income countries. This difference may increase discrepancies in access to PHC, and consequently, in rates of AH.
Few studies among those published on children included socioeconomic status (SES) as a possible confounder of the association between race/ethnicity and AH rates [12, 22, 23, 26, 28]. In these studies, the proxy for SES was always at area- or ZIP code-level, except for individual insurance status or source of payment. Only one study tried to assess if the AH rates among different ethnic groups would have been modified by the adjustment for SES [22], showing that disparities by race and ethnicity persisted even among persons within the same insurance classification. Although not directly comparable, the present study found similar results, since adjusting for individual-level SES covariates (maternal education) attenuated disparities among migrants and natives but significant differences persisted.
The increased overall risk of AH found in children born to immigrant mothers was mostly due to hospitalizations for gastroenteritis, ear and upper respiratory tract infections, and asthma. As for the overall AH definition, European studies on hospital admissions for gastroenteritis and URTI are lacking among migrants. In the US, Chang and Pope [14] found a lower risk of gastroenteritis among Blacks, whereas Russo [30] found a higher risk among Hispanics, but similar rates among Blacks and Asiatic. Only for asthma, some specific European literature was available. The increased risk of asthma found among children born to immigrant mothers in the present study is coherent with UK literature underlying higher asthma-related hospitalization rates among ethnic minorities (especially Blacks vs. Whites) [31], even though other two studies conducted in Sweden found a lower risk of asthma-related hospitalization among children born outside Sweden [32] and among children born to immigrant mothers [33].
The present study has a longitudinal design with an open birth cohort approach. This design has important strengths; first, by enrolling all the region’s newborns during the follow-up period authors accounted for the great dynamism of the immigrant population. Second, by linking the MBR with the regional hospital discharge records database at an individual level authors obtained the exact person-time at risk and avoided biases due to the numerator-denominator mismatch in ecological cross-sectional studies [34]. Another strength of this design lies in that all exposures and outcomes were first recorded separately and subsequently pooled using record linkage, so the findings are unaffected by any interview or recall bias. Furthermore, a birth cohort has the advantage of excluding the influence of different duration of stay in the host country among migrants on the outcome, that would be especially relevant in a population of children. Another strength worth noting is the assessment of SES’ influence, which allowed authors to separate it from the role played by migrant status, the main exposure variable. The authors used maternal education as a proxy variable for SES, which has been proven to be a constant, reliable measure of SES, showing good correlation with it [19]. Finally, authors analyzed a large and clearly defined population, with a total of 1,902,041 person-years of follow-up and an overall number of 16,744 children that experienced at least one AH.
In authors’ opinion, the main limitation of this study lies in the choice of maternal migratory status as the exposure variable. While using a birth-cohort provides the advantages discussed above, it also means that all children born abroad were excluded from this study. By choosing maternal citizenship as exposure variable, authors looked at migration as a social phenomenon having consequences that go beyond one’s actual place of birth, and which can extend to the so called “second generation”, but authors did not account for the subgroup of children actually migrating themselves (i.e., born abroad and then moved in). In Italy, immigrants can obtain citizenship by marriage or, on demand, after a period of at least 10 y of legal residence provided eligibility criteria are met [35]. By considering maternal citizenship as the exposure variable, it can be reasonably sure that authors accounted for most of the mothers who migrated more recently, which are possibly those most affected by migration, but on the other hand authors classified those immigrant mothers who acquired Italian citizenship at some point before giving birth to the enrolled children as Italians. Moreover, authors were not able to measure the time of arrival of mothers and their length of stay, neither they accounted for the role played by paternal citizenship. On the other hand, the children’s citizenship, not available in the MBR, would not have been an optimal choice either, since children having at least one Italian parent do have Italian citizenship, and thus they would have all been indiscriminately grouped with Italians. Finally, authors have not sub-grouped children by maternal geographical areas (i.e., Eastern Europe, South America, Africa, Asia) due to the relatively low number of AH among children born to HMPC mothers.
Recent studies indicate that even among countries with universal healthcare like EU countries, integration policies adopted towards migration can influence migrants’ health. In those European countries scoring higher in the Migrant Integration Policies Index (MIPEX), migrants have been found to report better health in comparison to countries with poorer integration policies [36, 37]. Italy has been found to score better than most of its European neighbors both in terms of integration policies and migrants’ self-rated health [37]. As to healthcare, legislation enacted in 1998 (Legislative Decree No. 286/1998 on Immigration and Aliens) grants legal immigrants access to health services in the same way as Italian citizens. Therefore, regular immigrants are entitled to access to primary care, ambulatory care, hospital care, rehabilitation and emergency care as Italian citizens do. However, like this study also suggests, much work remains to be done in order to meet health needs of socially disadvantaged population groups and to achieve actual implementation of universality and equity in healthcare.
In conclusion, children born to mothers from High Migratory Pressure Countries experienced more need for avoidable hospitalizations than those born to Italian mothers. This indicates that maternal migration can have an impact on the children’s access to primary healthcare even in countries with universal healthcare and inclusive health systems. The present results also underlined the persistence of social barriers to health services related to being born to mothers with personal histories of recent immigration. Although ethnic minorities and migrant children are considered as vulnerable health-care groups, research concerning avoidable hospitalization is lacking in the European context and this warrants further studies allowing temporal and spatial comparisons, as well as a deep understanding of the specific causes and mechanisms underlying, because of the possible implications for future public health policies.
References
ISTAT - Indicatori demografici sintetici [Internet]. Available at http://dati.istat.it. Accessed 19 Nov 2019.
Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23:325–48.
Asanin J, Wilson K. “I spent nine years looking for a doctor”: exploring access to health care among immigrants in Mississauga, Ontario, Canada. Soc Sci Med. 2008;66:1271–83.
Pérez-Escamilla R, Garcia J, Song D. Health care access among Hispanic immigrants: ¿Alguien Está Escuchando? [Is anybody listening?]. NAPA Bull. 2010;34:47–67.
Rechel B, Mladovsky P, Devillé W. Monitoring migrant health in Europe: a narrative review of data collection practices. Health Policy. 2012;105:10–6.
Norredam M, Nielsen SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe--a systematic review. Eur J Pub Health. 2010;20:555–63.
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502.
van Loenen T, van den Berg MJ, Westert GP, Faber MJ. Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract. 2014;31:502–16.
Thygesen LC, Christiansen T, Garcia-Armesto S, Angulo-Pueyo E, Martínez-Lizaga N, Bernal-Delgado E. Potentially avoidable hospitalizations in five European countries in 2009 and time trends from 2002 to 2009 based on administrative data. Eur J Pub Health. 2015;25:35–43.
Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) Spring. 1993;12:162–73.
Agabiti N, Pirani M, Schifano P, et al. Income level and chronic ambulatory care sensitive conditions in adults: a multicity population-based study in Italy. BMC Public Health. 2009;9:457.
Shi L, Samuels ME, Pease M, Bailey WP, Corley EH. Patient characteristics associated with hospitalizations for ambulatory care sensitive conditions in South Carolina. South Med J. 1999;92:989–98.
Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care. 1998;36:804–17.
Chang CF, Pope RA. Potentially avoidable hospitalizations in Tennessee: analysis of prevalence disparities associated with gender, race, and insurance. Public Health Rep. 2009;124:127–37.
Friedman B, Basu J. Health insurance, primary care, and preventable hospitalization of children in a large state. Am J Manag Care. 2001;7:473–81.
Dalla Zuanna T, Spadea T, Milana M, et al. Avoidable hospitalization among migrants and ethnic minority groups: a systematic review. Eur J Pub Health. 2017;27:861–8.
AHRQ - Quality Indicators [Internet]. Available at: http://www.qualityindicators.ahrq.gov/modules/pdi_overview.aspx. Accessed 19 Nov 2019.
Pirani M, Schifano P, Agabiti N, Davoli M, Caranci N, Perucci CA. Potentially avoidable hospitalisation in Bologna, 1997–2000: temporal trend and differences by income level. Epidemiol Prev. 2006;30:169–77.
Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–84.
Malmusi D, Borrell C, Benach J. Migration-related health inequalities: showing the complex interactions between gender, social class and place of origin. Soc Sci Med. 2010;71:1610–9.
Craig E, Anderson P, Jackson G, Jackson C. Measuring potentially avoidable and ambulatory care sensitive hospitalisations in New Zealand children using a newly developed tool. N Z Med J. 2012;125:38–50.
Gaskin DJ, Hoffman C. Racial and ethnic differences in preventable hospitalizations across 10 states. Med Care Res Rev MCRR. 2000;57:85–107.
Hale N, Probst J, Robertson A. Rural area deprivation and hospitalizations among children for ambulatory care sensitive conditions. J Comm Health. 2016;41:451–60.
Lessard LN, Alcala E, Capitman JA. Pollution, poverty, and potentially preventable childhood morbidity in Central California. J Pediatr. 2016;168:198–204.
Matheson D, Reidy J, Tan L, Carr J. Good progress for children coupled with recalcitrant inequalities for adults in New Zealand’s journey towards universal health coverage over the last decade. N Z Med J. 2015;128:14–24.
Shi L, Lu N. Individual sociodemographic characteristics associated with hospitalization for pediatric ambulatory care sensitive conditions. J Health Care Poor Underserved. 2000;11:373–84.
Tan L, Carr J, Reidy J. New Zealand evidence for the impact of primary healthcare investment in Capital and Coast District Health Board. N Z Med J. 2012;125:7–27.
Hakim RB, Bye BV. Effectiveness of compliance with pediatric preventive care guidelines among Medicaid beneficiaries. Pediatrics. 2001;108:90–7.
Bhopal RS. Migration, Ethnicity, Race, and Health in Multicultural societies. 2nd ed. Oxford, USA: Oxford University Press; 2014.
Russo CA, Andrews RM, Coffey RM. Racial and ethnic disparities in potentially preventable hospitalizations, 2003: statistical brief #10. Healthc Cost Util Proj HCUP Stat Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. Available at: http://www.ncbi.nlm.nih.gov/books/NBK63497/. Accessed 19 Nov 2019.
Netuveli G, Hurwitz B, Levy M, et al. Ethnic variations in UK asthma frequency, morbidity, and health-service use: a systematic review and meta-analysis. Lancet. 2005;365:312–7.
Hjern A, Haglund B, Bremberg S, Ringbäck-Weitoft G. Social adversity, migration and hospital admissions for childhood asthma in Sweden. Acta Paediatr. 1999;88:1107–12.
Li X, Sundquist J, Calling S, Zöller B, Sundquist K. Mothers, places and risk of hospitalization for childhood asthma: a nationwide study from Sweden. Clin Exp Allergy. 2013;43:652–8.
Ikram UZ, Mackenbach JP, Harding S, et al. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. 2016;31:655–65.
MINISTERO DELL’INTERNO, Diritti, doveri, identità, partecipazione. Come diventare cittadini italiani [Internet]. Minist. Dell‘Interno. Available at: http://www.interno.gov.it/it/temi/cittadinanza-e-altri-diritti-civili/cittadinanza. Accessed 19 Nov 2019.
Giannoni M, Franzini L, Masiero G. Migrant integration policies and health inequalities in Europe. BMC Public Health. 2016;16:463.
Malmusi D. Immigrants’ health and health inequality by type of integration policies in European countries. Eur J Pub Health. 2015;25:293–9.
Author information
Authors and Affiliations
Contributions
AB and CC designed the study and wrote the manuscript; LS and LZ participated in coordination of the study; CC performed the statistical analysis; TDZ, SF, LZ and RIC critically revised the manuscript and contributed to the discussion. All authors contributed to results interpretation, read and approved the final manuscript. Prof. Cristina Canova will act as guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bardin, A., Dalla Zuanna, T., Favarato, S. et al. The Role of Maternal Citizenship on Pediatric Avoidable Hospitalization: A Birth Cohort Study in North-East Italy. Indian J Pediatr 86 (Suppl 1), 3–9 (2019). https://doi.org/10.1007/s12098-018-2826-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-018-2826-6