Abstract
Epilepsy surgery has become an accepted treatment for drug resistant epilepsy in infants and children. It has gained ground in India over the last decade. Certain epilepsy surgically remediable syndromes have been delineated and should be offered surgery earlier rather than later, especially if cognitive/behavioral development is being compromised. Advances in imaging, particularly in MRI has helped identify surgical candidates. Pre-surgical evaluation includes clinical assessment, structural and functional imaging, inter-ictal EEG, simultaneous video -EEG, with analysis of seizure semiology and ictal EEG and other optional investigations like neuropsychology and other newer imaging techniques. If data are concordant resective surgery is offered, keeping in mind preservation of eloquent cortical areas subserving motor, language and visual functions. In case of discordant data or non-lesional MRI, invasive EEG maybe useful using a two-stage approach. With multi-focal / generalized disease, palliative surgery like corpus callosotomy and vagal nerve stimulation maybe useful. A good outcome is seen in about 2/3rd of patients undergoing resective surgery with a low morbidity and mortality. This review outlines important learning aspects of pediatric epilepsy surgery for the general pediatrician.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is one of the major clinical problems in pediatric practice and drug-resistant epilepsy (DRE) often results in major disability and a poor quality of life.
Antiepileptic drugs are the mainstay of management in newly diagnosed epilepsy but about a third of patients will have unsatisfactory control [1]. In patients with DRE, recurrent seizure activity and even drug therapy itself can be harmful to the developing brain. These patients must be evaluated for surgical treatment. Surgical treatment of epilepsy has become increasingly feasible due to major advances in structural and functional neuroimaging, video-EEG monitoring and surgical techniques. About 10–50 % of the patients with DRE are amenable to surgical treatment [2]. The purpose of surgical resection is essentially seizure freedom, rather than seizure reduction as quality of life is linked to this outcome [3]. There are often additional benefits on neurodevelopment which can be considered a bonus and not a primary indication for surgery.
Drug Resistant Epilepsy
Before labeling patients as drug resistant epilepsy we should rule out pseudo-resistance. The main reasons for pseudo-resistance are wrong diagnosis (non-epileptic epilepsy mimics), inappropriate antiepileptic drugs (AEDs) (like carbamazepine for absence seizures), inadequate dose and non- compliance to AEDs.
DRE is defined in many ways but three important things need to be considered - number of drug failures, seizure frequency and duration and impact on the patient’s development.
What is now apparent is that despite the availability of several new AEDs, the percentage of patients achieving long-lasting seizure freedom does not increase beyond a point. In the landmark Glasgow study [1] on long term follow up of newly diagnosed epilepsy, 47 % become seizure free with the first AED, 13 % on the 2nd AED and only 4 % on the 3rd or a combination of two drugs. These observations suggest that when two appropriately chosen AEDs given at an adequate dosage, fail the chances of success with further agents rapidly diminish. This view has been contested lately though [4].
There is no consensus on what frequency of seizures defines intractability and rightly so. The situation is different depending on the disease and age e.g., several minor seizures in an infant with cerebral palsy maybe less handicapping than monthly seizures in an independent college -going adolescent
How long should a patient wait before considering surgery is a critical issue? The “rule of two” is often used in adult epilepsy i.e., consider surgery if at least two AEDs are ineffective over two years. However two years maybe too long to wait in infantile catastrophic epilepsy with it’s devastating effects on development. On the other hand, even DRE has a remission rate of 4 % a year [Udani unpublished data]. All these factors need to be considered before evaluating a patient for epilepsy surgery.
Epileptogenic and Other Cortical Zones
Before a detailed discussion on epilepsy surgery, an understanding of the concept of the epileptogenic zone and other cortical zones is in order.
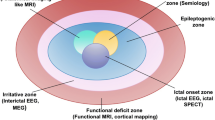
The epileptogenic zone (EZ) is a theoretical concept describing the region of cortex responsible for generating seizures (Fig. 1). Thus, resection or disconnection of the EZ will result in seizure freedom. The precision with which the EZ can be identified is limited with existing technology. Preserving eloquent cortical areas often limits the extent of a resection. Whether this is sufficient to provide seizure freedom depends upon the location of the other cortical zones, on whether the known ictal generator has been resected, and whether there exist other potential generators of ictal activity within the remaining EZ.
The EZ could be involving discrete, regional, hemispheric or bilateral epilepsy networks. The first three are often amenable to curative surgery while the last maybe helped by palliative surgery (as discussed below).
Clinically, we may define several cortical zones, which serve as markers for the EZ. When these zones overlap to describe the same cortical area, they localize the EZ with increased confidence. The five generally accepted conceptual regions include ictal onset zone, irritative zone, symptomatogenic zone, anatomic lesion/lesions and functional deficit zone (Fig. 1).
The ictal onset zone defines the cortical region generating ictal EEG onset. This does not include additional regions of the EZ necessary for seizure propagation and spread, nor other potential ictal generators within the EZ. Surface EEG gives an approximate localization, with more precise definition possible via intracranial EEG recording. Though limited by the lag between seizure onset and tracer transport to the ictal focus, a prompt ictal single photon emission computed tomography (SPECT) also aims to define the ictal onset zone. The ictal onset zone is often believed to be smaller than the EZ and must be removed for long-term seizure freedom.
The irritative zone refers to the cortical region generating inter-ictal epileptiform discharges and often may exceed the boundary of the EZ suggesting that it does not always have to be removed completely for seizure freedom. This zone may be defined by surface EEG, or more precisely by intracranial EEG. Magnetoencephalography (MEG) may also define this zone of interictal activity in deeper cortical or subcortical regions.
The symptomatogenic zone refers to the region of cortex that generates the clinical semiology of habitual clinical seizures when activated. This area may frequently be different from the EZ as ictal onset may occur in functionally “silent” regions of cortex. A seizure becomes clinically apparent only after spread has occurred to the symptomatogenic zone. Reviewing seizure semiology, by history or video-EEG capture, may localize the symptomatogenic zone.
An anatomic lesion identified by MRI is the single most important predictor for surgical success [5]. However, sometimes a lesion may not necessarily be epileptogenic. Furthermore, the EZ may include only part of a lesion, or extend to cortex beyond the anatomic boundaries of a given lesion. Also, one may have multiple lesions [for example in tuberous sclerosis (TS)], where only one might be epileptogenic, and surface video-EEG recording and other techniques would be necessary to confirm the epileptogenicity of a particular lesion.
The functional deficit zone is defined as the brain area that shows abnormal functioning in the interictal period. This abnormal functioning can be due to the effects of a structural lesion and/or due to the functional consequences of the persisting epileptic condition. The location and extent of the functional deficit zone can be assessed directly with the neurological examination and neuropsychological assessment (including the Wada test) and indirectly using surrogate markers of abnormal functioning including functional neuroimaging tools like single-photon-emission-tomography (SPECT), positron-emission-tomography (PET), magnetic resonance spectroscopy (MRS) and functional magnetic resonance imaging (fMRI). Assessment of this zone helps surgical decision making, e.g., Hemispherotomy is a much easier decision in a hemispheric epilepsy if a hemiplegia already exists pre-operatively.
Recently the ILAE sub-commission on pediatric epilepsy surgery has published a consensus statement on criteria for referral and evaluation of pediatric epilepsy surgery patients [6] and also use of diagnostic tests in the evaluation of epilepsy surgery [7]. Similar Indian guidelines have been published for both adult and pediatric surgery [8].
Surgically Remediable Epilepsy Syndromes (SRES)
Certain epilepsy syndromes are recognized in infants and children, which often tend to be drug-resistant and amenable to surgery. These are:
-
1)
Hemispheric syndromes: a) Hemispheric gliotic scars like what one gets with old arterial infarcts causing congenital hemiplegia b) Rasmussen’s encephalitis c) Sturge –Weber syndrome d) Hemimegelencephaly / Hemispheric cortical dysplasia. Catastrophic epilepsy is often encountered, especially in Rasmussen’s encephalitis and hemimegelencephaly. As these lesions often have an associated unilateral motor / visual field deficit, the decision to operate becomes easier.
-
2)
Lesions: Tumors, especially developmental in origin like: Dysembryoplastic neuroepithelial tumours (DNET) and gangliogliomas are important causes of DRE and are usually easily resected. The usually discrete, Focal Cortical Dysplasia (FCD) type 2 is the other lesion commonly helped by surgery. However FCDs need a lot more evaluation than tumors. Discrete or lobar / multi-lobar gliotic scars and vascular malformations are other important SRES.
-
3)
Mesial Temporal Lobe Epilepsy (MTLE): This is the commonest syndrome operated on in adults and often in adolescents. The substrate is usually hippocampal sclerosis (HS). However in younger children, isolated HS is only occasionally associated with MTLE. If present, it is often part of a dual pathology, most often a FCD. Other pathologies with childhood MTLE are tumors and gliotic scars.
-
4)
Neurocutaneous syndromes: Tuberous Sclerosis (TS) has recently been added to the SRES in childhood. Often in TS a single tuber is often responsible for contemporary epilepsy. The challenge is to identify the EZ associated with that tuber and multiple strategies can be used. Sturge –Weber syndrome (SWS) often presents in infants with catastrophic drug-resistant partial epilepsy and hemispheric surgeries can often reverse the developmental regression, which invariably follows. The recent, early use of aspirin may help reduce the need for surgery though [9].
-
5)
West syndrome and other epileptic encephalopathies can sometimes be drug-resistant and can play havoc with the infant’s development. Often, these can be due to a discrete lesion like FCD or a developmental tumor and surgery should be pursued early in these cases. In the early 1990s, 18 F-fluorodeoxyglucose (FDG) PET identified unifocal areas of hypometabolism in MRI-negative cases, which when operated on were found to be FCDs on pathology [10]. Since then many of these cases have been brought into the surgical domain with significant post-operative improvements in behavior and development [11].
Pre-surgical Evaluation [12]
Mandatory Investigations
Clinical Interviews / Examination
A detailed interview with the patient (especially a verbal cooperative older child / teenager)/ parents / friends is mandatory to recapitulate the past medical history, seizure semiology – both past and present, video-clippings of seizures and details of any stereotypic aura which might help lateralize / localize the patient’s habitual seizures. A history of lateralized prolonged febrile seizures in infancy might suggest hippocampal sclerosis and MTLE while a history of neonatal hypoglycemia or a past history of meningo-encephalitis might suggest multifocal pathology.
Examination should focus on hand / leg dominance and to exclude motor / visual and language deficits.
MRI
This is the single most important investigation in epilepsy surgery in infants and children. Identification of a lesion hugely improves the chances of a successful surgical outcome. Further investigations usually focus on the relationship between the MRI lesion and the seizures, on whether the EZ extends beyond the lesion, whether eloquent areas are likely to be in proximity to the lesion, deciding safety of surgical resection. The problem is that lesions like FCDs, HS and subtle gliotic scars need dedicated epilepsy protocols as routine MRIs may miss the lesion completely. Sequences for FCDs include T1 SPGR and 3-D fliuid attenuated inversion recovery (FLAIR) to identify subtle fuzziness at the grey-white matter interface or high intensity signals in the white matter especially if traced to the ventricle. For HS,3-D acquired T1, T2 and FLAIR thin 1 mm coronal slices of the temporal lobe perpendicular to the long axis of the hippocampus are needed. Gliotic scars, especially with neonatal hypoglycemic injury may be sometimes subtle and be seen only on FLAIR sequences. Gradient echo (GRE) / susceptibility weighted imaging (SWI) are essential to pick up cavernomas or other lesions with blood products or calcification.
In other words imaging in epilepsy surgery demands a high tesla strength (above 1.5 T – preferably 3 T) with experienced neuroradiologists. It is essential for the neuroradiologist to be guided by electro-clinical findings along with results of functional neuroimaging so that customized sequences for lesion detection are undertaken for an optimal result.
Simultaneous Video-EEG (sVEEG) [13]
The primary aim of sVEEG is to try and lateralise the seizure to one hemisphere and further localize it to a lobe or a region.
sVEEG can usually be recorded for several days to weeks to try and capture a few habitual seizures for semiological analysis. The simultaneous recording of the ictal EEG is helpful in confirming the ictal onset region.
Seizure Semiology The manner in which a seizure starts and evolves (seizure semiology) offers important clues to location of seizure onset and subsequent spread. Auras are very helpful in localizing seizure onset to a particular region. The later parts of the semiology are more important for spread patterns. In an older child, seizure semiology often has features resembling localization-related seizures in adults.
Frontal lobe seizures are typically of short duration, unassociated with postictal confusion, and frequently nocturnal. Tonic or postural features and hypermotor features like thrashing, pedaling, and kicking the lower extremities are common. Supplementary motor seizures arising from the mesial surface have bilateral asymmetric tonic postures but full preservation of consciousness.
Temporal lobe seizures often have auras such as epigastric ‘pain’ or rising sensation, fear or other psychic sensations. Distal hand automatisms like fumbling, and oral lip smacking / chewing are characteristic. Younger children have simpler while older children have more complex automatisms. Early tonic-clonic movements are unusual. Postictal confusion / aphasia are prominent especially with seizures from the dominant temporal lobe.
Occipital / parietal and posterior temporal areas give rise to posterior cortical seizures. Simple visual auras (sparks, flashes, scotomata, blindness) is typical of occipital lobe onset while more formed complex images are noted with temporal-occipital onset. Contralateral eye deviation, blinking, a sensation of eye movement, and nystagmoid eye movements are also seen. Prominent sensory auras like paresthesiae suggest contralateral parietal lobe. Posterior cortex onset seizures often spread to evolve into temporal lobe –like seizures or have contralateral head and eye deviation suggesting spread to frontal motor areas.
In infants and young children less than 3 y of age the normal rules of semiology do not apply [14, 15]. These are hypomotor seizures where only behavior arrest is seen or are focal / generalized, tonic / clonic motor seizures and epileptic spasms. Often “generalized” seizures occur from discrete lesions and hence should not be used as a point against surgery as a therapeutic option.
Ictal EEG Analysis Inter-ictal and ictal EEG analysis helps confirm region of onset well in temporal lobe seizures and is often unhelpful in frontal lobe seizures where bilateral changes or muscle artifacts predominate. It has been shown that in early lesions, either developmental or acquired, generalized or contralateral interictal or ictal epileptic discharges did not detract from a successful surgical outcome (Fig. 2) [16]. This suggests that in infants and young children, an MRI lesion is probably the single most important determinant of whether surgery should be pursued.
Findings in a 2-y-old with refractory infantile spasms; (a: EEG showing generalised epileptic discharges – inter-ictal and ictal (b: MRI brain showing right temporal FCD (blurring grey-white junction; thickened cortex); (c: PET scan showing right temporal hypometabolism (d: MRI brain showing right temporal lobectomy; Post-operative seizure freedom for 1 y
Optional Investigations
Neuropsychology
This is essential in adult / adolescent epilepsy surgery involving the hippocampal structures. It helps in lateralizing the epilepsy as verbal memory functions are sub-served by the left hippocampus and visual memory by the right. It also helps decide whether post-operative memory function would remain adequate after unilateral hippocampal resection. This is extremely important when considering dominant hippocampal resection in high functioning individuals as even mild declines in memory functions may impair daily activities. In younger children and infants, neuropsychology is usually not mandatory but establishes a baseline against which post-operative scores are compared.
Functional Neuroimaging
Positron Emission Tomography (PET) The most commonly used tracer is the 18 F-fluorodeoxyglucose (FDG) and it is used based on the principle that the EZ is usually hypo-metabolic in the inter-ictal state. It is offered routinely in patients with MRI-negative DRE. It is more useful in temporal lobe epilepsy (TLE) than in extra-temporal lobe epilepsy (ETLE). There is also a good experience in infantile spasms where a single hypometabolic area might suggest an underlying FCD. Other tracers like 11C alpha-methyl-tryptophan (AMT) are often useful in detecting the epileptic tuber amongst the many tubers in tuberous sclerosis [17].
ICTAL Single Photon Emission Computed Tomography (SPECT) SPECT is a marker for cerebral blood flow (CBF). During a seizure, CBF increases markedly in the EZ and in areas of seizure propagation – more so in the former. It is performed with an injection of a tracer [either hexamethylpropyleneamine oxime (HMPAO) or ethyl cysteinate diethylester (ECD)] during a sVEEG confirmed seizure and the earlier the injection (best before 30 s) the more accurate the localization of the EZ. Later injections may be falsely localizing as there maybe an ictal switch in the EZ from hyperperfusion to hypoperfusion. Also ictal spread patterns rather than ictal onset maybe highlighted. Subtraction ictal SPECT co-registered with MRI (SISCOM) subtracts inter-ictal from ictal images and helps further optimization of the image in relation to the anatomic area on MRI. It is of maximum use when the MRI is normal or only subtly abnormal like in FCD. It also helps planning the placement of intracranial EEG electrodes.
Advanced MRI Techniques
Mapping out eloquent areas including the sensorimotor cortex, language and visual areas are now possible with Blood Oxygen Level Dependent (BOLD) functional MRI (fMRI), where test paradigms are now well established in the co-operative older child. Functional MRI is based on subtle variations of blood flow, which occur when a particular activity is performed repeatedly. For example, movement of the hand will result in increases in the blood flow in the contralateral sensorimotor cortex with resultant increased extraction of oxygen relative to the resting state (Fig. 3a). This difference in the blood oxygen level between the active and resting states is imaged with a resultant map. Another technique called Diffusion Tensor Imaging (DTI) maps out the eloquent white matter tracts – e.g., corticospinal tract which emanates from the sensori-motor cortex (Fig. 3b). Hence both the eloquent cortices (fMRI) and their white matter connections (DTI) provide the surgeon with a functional map of eloquent areas to be avoided during surgery. The intra-carotid amytal test (WADA test), which was used, earlier for lateralizing language and memory functions is used less so nowadays after the advent of fMRI.
Magnetoencephalography (MEG)
This technique is based on detection of magnetic fields generated by brain neuronal activity. In contrast to the scalp EEG which identifies electrical activity from the surface, MEG identifies magnetic signals from the deeper cortex including that cortex adjacent to the sulci. Unlike the EEG signal, MEG signals do not get attenuated or distorted by the skull and intervening tissues. MEG can also be used to localize eloquent cortices. The cost-benefit of this extremely expensive equipment along with the expertise required is still debated. It has recently been installed in two central government medical institutes in India.
A multi-disciplinary epilepsy surgery management conference to collate and discuss the information from different non-invasive evaluations is the next step. Here, decisions on whether the patient is a surgical candidate are taken based on risk-benefit analysis. Resective surgeries are most likely to be successful when data from all these different modalities are congruent with localization hypothesis. If data are non-congruent of if eloquent cortex is adjudged to be at risk, a decision on whether intracranial EEG / functional cortical mapping is needed or not would be taken.
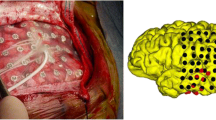
Intracranial EEG
If confident localization of the EZ has not been achieved after non-invasive evaluation, intracranial EEG recording maybe considered if there is a reasonable hypothesis. These often include patients with normal MRI or even lesional cases with discordant data or proximity to eloquent cortex. Subdural (Fig. 4) or depth electrodes are surgically implanted and sVEEG performed to capture inter-ictal / ictal recording from the cortex to exactly delineate the EZ as well as accurately map eloquent areas. Then a second stage resection is carried out.
Surgical Procedures
Surgery can be of two major categories, either resective (curative) or palliative. Resective surgeries aim at removal or disconnection of the EZ and have the potential to be curative, while palliative surgeries are aimed at reduction in intensity and frequency of seizures.
Resective (Potentially Curative) Surgery
Lobectomy / Multi-lobar Resections
Temporal lobectomy is the most commonly performed type of surgery in adults. A randomized controlled trial comparing surgical and medical treatment in early mesial temporal lobe epilepsy caused by hippocampal sclerosis confirmed the superiority of early surgical treatment [18]. In children, FCDs and developmental tumors with or without HS are the substrate. Long-term outcome in childhood temporal lobe surgery approaches 75 % after a minimum of 2 y follow-up [19, 20] declining to about 67 % after a 10 y follow up [21]. Extra-temporal lobectomies and multi-lobar resections have lower rates of seizure freedom.
Lesionectomy
In most lesions, epileptogenicity comes from surrounding dysfunctional cortex e.g., cortex surrounding a tumor or cavernoma. A notable exception is an intrinsically epileptogenic lesion like FCD 1. Once pre-surgical evaluation establishes the causal relationship between a lesion and epilepsy, lesionectomy with excision of surrounding cortex is usually successful in achieving seizure freedom in about 80 % at the end of one year follow up [22]. Longer follow up suggest an advantage of using intra-operative electrocorticography (ECoG) to guide resection [22].
Hemispheric Surgery
Current hemispheric surgery focuses less on resection and more on disconnection of epileptic tissue essentially de-efferenting it and so rendering it non-functional. This procedure is called hemispherotomy and is slowly replacing the more resective functional hemispherectomy. Outcomes are probably similar in both with 66-80 % achieving seizure freedom [23, 24]. Mortality is low though there is a steep learning curve for the surgeon. Post-opertive hydrocephalus complicates a quarter of hemispherectomy cases [24, 25] and can occur upto 2 y after [25]. About a third of hemispherectomy patients need blood transfusions [26]. Severe unilateral pathologies like Rasmussen encephalitis, Hemiconvulsion-Hemiplegia-Epilepsy syndrome (HHE), hemimegelencephaly / hemispheric dysplasia, Sturge-Weber syndrome and large gliotic lesions like old infarcts, make up most of the cases in large series [23, 24]. The worst outcome is seen in patients with hemimegelencephaly vis-à-vis acquired pathologies [23, 24].
Palliative Surgery
Corpus Callosotomy
Corpus callosotomy is a procedure disconnecting the two hemispheres by division of the corpus callosum and can be partial or total. It is most useful in epilepsies where drop attacks are prominent like the Lennox-Gastaut syndrome. Long-term outcome studies show a good outcome in ~ 75 % of drop attacks with the anterior 2/3rd corpus callosotomy [27] while total callosotomy has about 90 % improvement [28]. It is more effective than vagal nerve stimulation (VNS) in the outcome of drop attacks [29]. Adverse effects are few and transient even with total callosotomy, which is fast becoming the procedure of choice in low-functioning individuals [28].
Vagus Nerve Stimulation
VNS is an invasive palliative non-pharmacological treatment in patients with DRE where curative surgery is not feasible. The vagus nerve stimulator consists of a pulse generator that delivers a continuous biphasic current through a lead that is attached to the left vagus nerve in the cervical region. In general, at least 50 % of patients experience at least 50 % reduction in seizure frequency [30] with improvements over time. The adverse effects are generally minor like hoarseness, throat pain, cough and others. In India, the high cost and the non-availability of after – sales service is a major dampener to its use.
Outcomes and Complications
In young children, the rate of seizure free outcome after all types of respective epilepsy surgery varies from 59 to 69 % [31–33]. The authors’ own data from the Hinduja hospital in Mumbai (Table 1) as well as data from Delhi [34] and Hyderabad [5] mirrors this experience. The completeness of resection appears to play a major role in the outcome of surgery, regardless of location (temporal or extra temporal) [32]. Certain etiologies do worse than others e.g., development-associated epilepsy [33]. Seizure freedom or improvement in seizure frequency is the main outcome measure in most studies. Developmental outcome studies stress the “catch-up” which occurs post-operatively [35, 36].
Epilepsy surgery generally has a low morbidity and mortality [37]. Micro-neurosurgery, neuro-navigation and improved pediatric anesthesia have contributed hugely to all neurosurgeries becoming safer over the years. Higher risk situations include hemispherectomy in infants where small blood volumes coupled with significant scalp blood loss becomes an issue. Motor and visual field deficits are expected in certain surgeries like hemispherectomy / hemispherotomy while they may sometimes unexpectedly complicate others e.g., quadrantic field defects in anterior temporal lobectomies. One clear advantage that children have is the innate plasticity of the brain allowing fairly good recovery of function e.g., resection of the language areas within the first 5–6 y leads to transient aphasias which almost always disappear as language functions switch to the opposite hemisphere.
Key Messages
-
1)
Epilepsy surgery is a safe and effective treatment for many infants and children with drug – resistant epilepsy.
-
2)
It needs a team approach with the help of several professionals including at least an epileptologist, neurosurgeon, neuroradiologist and neuropsychologist.
-
3)
Technology advances especially in digital video-EEG, imaging and neurosurgery have made surgery possible for many and also enhanced safety.
-
4)
Seizure-free outcomes approach 70 % and often are accompanied by improvements and stabilization of developmental and cognitive outcomes.
References
Kwan P, Brodie M Early identification of refractory epilepsy. N Engl J Med. 2000;342:314–9.
Engel J Jr. Why is there still doubt to cut it out. Epilepsy Curr. 2013;13:198–204.
Elliott I, Kadis DS, Lach L, Olds J, McCleary L. Quality of life in young adults who underwent resective surgery for epilepsy in childhood. Epilepsia. 2012;53:1577–86.
Luciano AL, Shorvon SD. Results of treatment changes in patients with apparently drug-resistant chronic epilepsy. Ann Neurol. 2007; 62:375–81.
Jayalakshmi S, Panigrahi M, Kulkarni DK, Uppin M, Somayajula S, Challa S. Outcome of epilepsy surgery in children after evaluation with non-invasive protocol. Neurol India. 2011;59:30–6.
Cross JH, Jayakar P, Nordli D, Delalande O, Duchowny M, Wieser HG, et al; International League Against Epilepsy, Subcommission for Paediatric Epilepsy Surgery; Commissions of Neurosurgery and Paediatrics. Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the Sub-commission for. Pediatric Epilepsy Surgery. Epilepsia. 2006;47:952–9.
Jayakar P, Gaillard WD, Tripathi M, Libenson MH, Mathern GW, Cross JH; Task Force for Paediatric Epilepsy Surgery, Commission for Paediatrics, and the Diagnostic Commission of the International League Against Epilepsy. Diagnostic test utilization in evaluation for respective epilepsy surgery in children. Epilepsia. 2014. doi: 10.1111/epi.12544.
Chandra PS, Tripathi M. Epilepsy surgery: recommendations for India. Ann Indian Acad Neurol. 2010;13:87–93.
Udani V, Pujar S, Munot P, Maheshwari S, Mehta N. Natural history and magnetic resonance imaging follow-up in 9 Sturge-Weber syndrome patients and clinical correlation. J Child Neurol. 2007;22:479–83.
Chugani HT, Shields WD, Shewmon DA, Olson DM. Infantile spasms: I. PET identifies focal cortical dysgenesis in cryptogenic cases for surgical treatment. Ann Neurol. 1990;27:406–13.
Jonas R, Asarnow RF, LoPresti C,Yudovin S, Koh S, Wu JY, et al. Surgery for symptomatic infant-onset epileptic encephalopathy with and without infantile spasms. Neurology. 2005;64:746–50.
Rosenow F, Luders H Presurgical evaluation of epilepsy. Brain. 2001;124:1683–1700.
Udani V. Surface and intracranial electroencephalographic in evaluation for epilepsy surgery. J Pediatr Neurosci. 2008;3:65–73.
Acharya JN, Wyllie E, Lüders HO, Kotagal P, Lancman M, Coelho M. Seizure symptomatology in infants with localization-related epilepsy. Neurology. 1997;48:189–96.
Nordli DR Jr, Bazil CW, Scheuer ML, Pedley TA. Recognition and classification of seizures in infants. Epilepsia. 1997;38:553–60.
Wyllie E, Lachhwani DK, Gupta A, Chirla A, Cosmo G, Worley S, et al. Successful surgery for epilepsy due to early brain lesions despite generalized EEG findings. Neurology. 2007;69:389–97.
Kagawa K, Chugani DC, Asano E, Juhász C, Muzik O, Shah A, et al. Epilepsy surgery outcome in children with tuberous sclerosis complex evaluated with alpha-[11C]methyl-L-tryptophan positron emission tomography (PET). J Child Neurol. 2005;20:429–38.
Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001;345:311–8.
Benifla M, Otsubo H, Ochi A, Weiss SK, Donner EJ, Shroff M, et al. Temporal lobe surgery for intractable epilepsy in children: an analysis of outcomes in 126 children. Neurosurgery. 2006;59:1203–13.
Englot DJ, Rolston JD, Wang DD, Sun PP. Seizure outcomes after temporal lobectomy in pediatric patients. J Neurosurg Pediatr. 2013;12:134–41.
Benifla M, Rutka JT, Otsubo H, Lamberti-Pasculli M, Elliott I, Sell E, et al. Long-term seizure and social outcomes following temporal lobe surgery for intractable epilepsy during childhood. Epilepsy Res. 2008;82:133–8.
Gelinas JN, Battison AW, Smith S, Connolly MB, Steinbok P. Electrocorticography and seizure outcomes in children with lesional epilepsy. Childs Nerv Syst. 2011;27:381–90.
Moosa AN, Gupta A, Jehi L, Marashly A, Cosmo G, Lachhwani D, et al. Longitudinal seizure outcome and prognostic predictors after hemispherectomy in 170 children. Neurology. 2013;80:253–60.
Schramm J, Kuczaty S, Sassen R, Elger CE, von Lehe M. Pediatric functional hemispherectomy: outcome in 92 patients. Acta Neurochir (Wien). 2012;154:2017–28.
Lew SM, Matthews AE, Hartman AL, Haranhalli N; Post-Hemispherectomy Hydrocephalus Workgroup. Posthemispherectomy hydrocephalus: results of a comprehensive, multiinstitutional review. Epilepsia. 2013;54:383–9.
Koubeissi MZ, Syed TU, Syed I, Jordan J, Alshekhlee A, Kossoff EH. Hemispherectomy-associated complications from the Kids' Inpatient Database. Epilepsy Res. 2009;87:47–53.
Tanriverdi T, Olivier A, Poulin N, Andermann F, Dubeau F. Long-term seizure outcome after corpuscallosotomy: a retrospective analysis of 95 patients. J Neurosurg. 2009;110:332–42.
Jalilian L, Limbrick DD, Steger-May K, Johnston J, Powers AK, Smyth MD. Complete versus anterior two-thirds corpus callosotomy in children: analysis of outcome. J Neurosurg Pediatr. 2010;6:257–66.
Lancman G, Virk M, Shao H, Mazumdar M, Greenfield JP, Weinstein S, et al. Vagus nerve stimulation vs. corpus callosotomy in the treatment of Lennox-Gastaut syndrome: a meta-analysis. Seizure. 2013;22:3–8.
Elliott RE, Morsi A, Tanweer O, Grobelny B, Geller E, Carlson C, et al. Efficacy of vagus nerve stimulation over time: review of 65 consecutive patients with treatment-resistant epilepsy treated with VNS > 10 years. Epilepsy Behav. 2011;20:478–83.
Wyllie E, Comair YG, Kotagal P, Bulacio J, Bingaman W, Ruggieri P. Seizure outcome after epilepsy surgery in children and adolescents. Ann Neurol. 1998;44:740–8.
Paolicchi JM, Jayakar P, Dean P, Yaylali I, Morrison G, Prats A, et al. Predictors of outcome in pediatric epilepsy surgery. Neurology. 2000;54:642–7.
Kim SK, Wang KC, Hwang YS, Kim KJ, Chae JH, Kim IO, et al. Epilepsy surgery in children: outcomes and complications. J Neurosurg Pediatr. 2008;1:277–83.
Dagar A, Chandra PS, Chaudhary K, Avnish C, Bal CS, Gaikwad S, et al. Epilepsy surgery in a pediatric population: a retrospective study of 129 children from a tertiary care hospital in a developing country along with assessment of quality of life. Pediatr Neurosurg. 2011;47:186–93.
Asarnow RF, LoPresti C, Guthrie D, Elliott T, Cynn V, Shields WD, et al. Developmental outcomes in children receiving resection surgery for medically intractable infantile spasms. Dev Med Child Neurol. 1997;39:430–40.
Freitag H, Tuxhorn I. Cognitive function in preschool children after epilepsy surgery: rationale for early intervention. Epilepsia. 2005;46:561–7.
Hader WJ, Tellez-Zenteno J, Metcalfe A, Hernandez-Ronquillo L, Wiebe S, Kwon CS, et al. Complications of epilepsy surgery: a systematic review of focal surgical resections and invasive EEG monitoring. Epilepsia. 2013;54:840–7.
Contributions
RS: Prepared the initial draft and helped in adding references to the manuscript; AB: Compiled data from Hinduja Hospital Epilepsy Surgery Programme; VU: Finalized and approved the manuscript, helped with further referencing. VU will act as guarantor for this paper.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, R., Botre, A. & Udani, V. Trends in Pediatric Epilepsy Surgery. Indian J Pediatr 82, 277–285 (2015). https://doi.org/10.1007/s12098-014-1660-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1660-8