Abstract
Background
Novel and highly effective drugs for non-melanoma skin cancer (NMSC) improve patient outcomes, but their high cost strains healthcare systems. Spain’s decentralized public health system, managed by 17 autonomous communities (AaCc), raises concerns about equitable access.
Methods
A cross-sectional survey (July–September 2023) was sent to Spanish Multidisciplinary Melanoma Group (GEM Group) members to assess access to new drugs.
Findings
Fifty physicians from 15 Spanish AaCc responded to the survey. Access for drug with approved public reimbursement, Hedgehog inhibitors in basal-cell carcinoma and anti PD-L1 antibody in Merkel carcinoma, was observed in 84% and 86% of centers, respectively. For other EMA-approved treatments, but without reimbursement in Spain access decreased to 78% of centers. Heterogeneity in access was mainly observed intra regions.
Conclusion
Unequal financial support for drugs for NMSC with creates a patchwork of access across Spanish hospitals, with variations even within the same AaCc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-melanoma skin cancer (NMSC) is the most common type of cancer in humans. Rates of NMSC in Spain have been on a continuous rise in recent years. In fact, Spain sees a staggering 10.85 new NMSC cases per 100,000 inhabitants every year, significantly higher than other European countries. Most of the cases are curable with surgery or local therapies, so the mortality is low, and advanced stages are uncommon. There are no official specific data on the number of advanced NMSC cases in Spain. The 5-year survival rate for advanced NMSC is around 50%, while the 5-year survival rate for early stage NMSC is over 95%. Mortality rates associated with NMSC in Spain were reported as 1.27 per 100,000 inhabitants in 2018 (95% CI 1.16–1.39) for the overall population [1].
Recent advancements in systemic therapies for NMSC include immunotherapy and targeted therapies [2, 3]. However, their high cost creates challenges for patients seeking access to these active medications. Recently, the European Federation of Pharmaceutical Industries Associations (EFPIA) survey indicates that only 28% of cancer drugs approved by European Medicines Agency (EMA) between 2018 and 2021 are fully available in Spain [4].
Spain’s public healthcare system is universal and operates through 17 regional health ministries, one for each Autonomous Community (AC). The national Spanish Agency of Medicines and Medical Devices (AEMPS) regulates drug approval, while the Inter-Ministerial Commission for Medicines Pricing (CIPM) sets pricing and reimbursement. Ultimately, each AC government decides on and finances drug costs. This decentralized system, can lead to significant disparities in patient access to treatment depending on their residence. The Spanish Society of Oncology (SEOM) [5], patient group societies [6], and scientific societies [7] have all raised concerns about equity and sustainability within this healthcare system.
While the high cost of new drugs is a concern, limited research has investigated how Spain’s decentralized healthcare system impacts access to these therapies for patients with NMSC. This study aims to described which is the situation of access to new drug for NMSC in Spain and if there are disparities in drug access across the country.
Methods
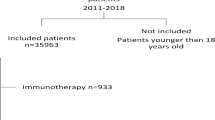
Study population and survey design
A cross-sectional survey was conducted between July and September 2023. The survey was electronically distributed to all members of the Spanish Melanoma Group (GEM) at hospitals across all Spanish AaCs. Only physicians with prescribing privileges for systemic cancer therapies were eligible to complete the anonymous questionnaire. The survey collected data on demographics, clinical practice settings, hospital characteristics, and physician access to NMSC treatments. The survey included items regarding access outside of clinical trials for these therapies in advanced-stage cutaneous squamous-cell carcinoma (CSC), basal-cell carcinoma (BCC), and immunotherapy for Merkel cell carcinoma (MCC).
Statistical analysis
All survey responses were subjected to descriptive analysis, categorized by AaC to identify potential regional variations. Additionally, subgroup analyses were performed to assess potential influences from prescribing physician characteristics (sex, age, and specialty) and hospital characteristics (public/private, tertiary/community, and city population size). Statistical analysis software SAS version 9.4 was used for this purpose.
Results
Among the 56 GEM physicians who responded to the survey, 50 prescribed systemic drugs for NMSC and were eligible for the final analysis. The final cohort included 50 hospitals from 15 Autonomous Communities (AaCc). Most participants were from public centers (n = 46, 92%), with only four private centers (8%) participating (two each in Catalonia and Madrid). The median participant age was 43 years (range 32–65), and 54% (n = 30) were women. The median number of participating centers per AaC was two (range 1–12). Nine AaCc had two or more participating centers (Table 1). No significant differences in drug access were observed based on prescriber age, sex, hospital type, or city population size.
Treatments options for cutaneous squamous-cell carcinoma (CSC) patients
Treatment options for CSC patients with advanced or metastatic disease, or lesions not amenable to surgery or radiotherapy, include the targeted therapy cetuximab [8] and immunotherapy with anti-PD-1 antibodies (primarily cemiplimab [9], pembrolizumab [10], and nivolumab [11]). Cemiplimab, Libtayo®, received EMA approval in 2019 for treating advanced CSC. However, there is currently no national reimbursement agreement for these treatments in Spain. Despite this, some Autonomous Communities (AaCc) and even individual hospitals within these regions have authorized the use of anti-PD-1 antibodies for these patients with advanced CSC.
Our survey revealed that 39 out of 50 hospitals (78%) reported having access to anti-PD1 antibody treatment for CSC. Notably, some centers within regions like Extremadura, Asturias, Catalonia, Valencia, Andalusia, and Aragon lacked access, despite other centers in those same regions having it. This suggests that access disparities may not be solely driven by regional policies (Fig. 1a).
Access to therapies for advanced cutaneous squamous-cell carcinoma (CSC). a Access to anti PD-1 antibodies. b Access to cetuximab. Percentage of centers in every AACC were marked in red when there was no access (public centers), gray when there was full access (public centers), blue when there was full access (private centers), pink no access (private centers), and brown if the specialist answered they did not known. pu public hospital, pr private hospital
Access to cetuximab was lower, with only 34 out of 50 hospitals (68%) reporting availability. Like anti-PD1 antibodies, access disparities were observed within some regions (Extremadura, Andalusia, Valencia, Madrid, and Catalonia). One hospital was unsure about access to anti-PD1 antibodies, and seven were unsure about access to cetuximab (Fig. 1b).
Treatments options for patients with basal-cell carcinoma (BCC)
Currently, the treatment options for patients with advanced locorregional or metastatic BCC include Hedgehog inhibitors (HHIs) that block a key pathway [12] and that are EMA-approved -vismodegib (Erivedge®, 2013) and sonidegib (Odomzo®, 2015) [13]—and Anti-PD-1 antibodies with two EMA-approved options that are cemiplimab (Libtayo®, 2018) and pembrolizumab (Keytruda®, 2014) for patients after failure to HHIs or intolerant to HHIs [14, 15].
In Spain, HHIs are reimbursed for first-line advanced or metastatic BCC, but there is no reimbursement agreement for anti PD-1 antibodies in BCC.
According to our study, there was access to Hedgehog inhibitors (HHIs) in 42 out of 50 hospitals (84%). Centers that answered that had no access were in Extremadura, Catalonia, and Madrid. However, within these regions, there were also hospitals that reported having access, suggesting potential discrepancies in access or reporting. One hospital was unsure about access to HHIs (Fig. 2a).
Access to therapies for advanced basal-cell carcinoma (BCC). a Access to HHIs. b Access to anti PD-1 antibodies. Percentage of centers in every AACC were marked in red when there was no access (public centers), gray when there was full access (public centers), blue when there was full access (private centers), pink no access (private centers), and brown if the specialist answered they did not known. pu public hospital, pr private hospital
Relating to anti-PD-1 antibodies, there was access in 39 out of 50 hospitals (78%) for advanced BCC. Centers without access were located in Extremadura, Asturias, Catalonia, Valencia, Andalusia, and Aragon. Like HHIs, there were instances of conflicting access reports within the same regions. Eleven hospitals were unsure about access to anti-PD-1 antibodies (Fig. 2b).
Treatments options for patients with Merkel cell carcinoma (MCC)
Patients with advanced MCC have one main treatment option consisting in immunotherapy with anti-PD-1 antibodies [16]. The EMA-approved anti-PD-L1 antibody for MCC is avelumab (Bavencio®), approved in 2017. In Spain, avelumab is reimbursed for this indication.
According to our survey, 43 out of 50 hospitals (86%) reported having access to immunotherapy. There were two hospitals where specialists were unsure about access to immunotherapy (the only hospital representing Asturias in the survey and one of the 11 hospitals in the Community of Madrid). All centers without access were in Andalusia, despite other hospitals in the same region reporting access (Fig. 3).
Access to anti PD-L1 antibody treatment for advanced Merkel cell carcinoma (MCC). Percentage of centers in every AACC were marked in red when there was no access in public hospitals, gray when there was full access, and yellow when there was access only for exceptional cases. pu public hospital, pr private hospital
Discussion
Our findings revealed a heterogeneous landscape of access, with reimbursement status playing a significant role. For public reimbursed therapies, higher availability across treatment centers was observed.
Interestingly, access to non-reimbursed therapies for NMSC appeared to be higher compared to similar situations observed in other tumor types, such as melanoma [17]. This disparity could be attributed to the relatively low prevalence of advanced NMSC and the limited availability of alternative treatment options. Consequently, some treatment centers appear to demonstrate greater flexibility regarding access to non-reimbursed drugs, with a significant portion, nearly 78%, reporting access to anti-PD-1 antibodies for BCC and SCC. However, the lack of reimbursement for certain NMSC therapies introduces challenges. When therapies lack established reimbursement, access becomes more dependent on subjective criteria and individual center policies. This can potentially lead to inequities in patient care, with access to potentially active treatments varying based on location and institutional policies.
While access patterns varied across regions, there was no clear indication that regional policies were the sole determinant of access disparities. Some regions now have a central committee to make decisions on drugs with pending financial decisions. Although we think that this is a first step in the right direction, there are still major differences among regions. Quick decisions about financing would be the best way to guarantee equal access throughout the country.
A small yet concerning proportion of physicians (2–4% for specific NMSC subtypes) exhibited uncertainty regarding reimbursement details. This highlights the potential need for improved communication and education initiatives targeting healthcare professionals to ensure accurate knowledge of reimbursement policies for novel NMSC treatments.
Additionally, educational initiatives targeting healthcare professionals could also play a crucial role. These efforts can help ensure that all patients receive optimal treatment options, regardless of location of patients.
Although this study is subject to limitations inherent to survey-based research, including potential response bias and the accuracy of self-reported dada, it highlights the complex landscape of access to novel NMSC therapies within the Spanish healthcare system. While public reimbursed therapies are generally available, disparities in access exist for non-reimbursed options. Addressing these disparities through further research, policy changes, and educational initiatives is crucial to ensure equitable access to these potentially active treatments for all patients with advanced NMSC.
References
Sendín-Martin M, Durán-Romero AJ, Martin-Carrasco P, Conejo-Mir J, Pereyra-Rodriguez JJ. Mortality associated with non-melanoma skin cancer in Spain from 1979 to 2018: trends and age-adjusted rates. Eur J Dermatol. 2021. https://doi.org/10.1684/ejd.2021.4110.
Silk AW, Barker CA, Bhatia S, Bollin KB, Chandra S, Eroglu Z, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of nonmelanoma skin cancer. J Immunother Cancer. 2022. https://doi.org/10.1136/jitc-2021-004434.
Shalhout SZ, Kaufman HL, Emerick KS, Miller DM. Immunotherapy for nonmelanoma skin cancer: facts and hopes. Clin Cancer Res. 2022;28(11):2211–20. https://doi.org/10.1158/1078-0432.CCR-21-2971.
EFPIA. European Federation of Pharmaceutical Industries and Associations (EFPIA). EFPIA Patients W.A.I.T. Indicator 2022 Survey. 2022.
Rodríguez-Lescure A, de la Peña FA, Aranda E, Calvo A, Felip E, Garrido P, et al. Study of the Spanish Society of Medical Oncology (SEOM) on the access to oncology drugs and predictive biomarkers in Spain. Clin Transl Oncol. 2020;22(12):2253–63. https://doi.org/10.1007/s12094-020-02366-y.
GEPAC. Cancer, cuestión de estado. https://www.gepac.es/cuestionestado/pdf/PROTOCOLO_CA%CC%81NCER_CUESTIO%CC%81N_DE_ESTADO_GEPAC_2023_.pdf (2023).
Calvo V, Camps C, Carcereny E, Cobo M, Dómine M, Campelo MRG, et al. Difficulties on the access to innovative targeted therapies for lung cancer in Spain. Clin Transl Oncol. 2023. https://doi.org/10.1007/s12094-023-03303-5.
Jarkowski A, Hare R, Loud P, Skitzki JJ, Kane JM, May KS, et al. Systemic therapy in advanced cutaneous squamous cell carcinoma (CSCC): the Roswell park experience and a review of the literature. Am J Clin Oncol. 2016;39(6):545–8. https://doi.org/10.1097/COC.0000000000000088.
Migden MR, Rischin D, Schmults CD, Guminski A, Hauschild A, Lewis KD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018;379(4):341–51. https://doi.org/10.1056/NEJMoa1805131.
Hughes BGM, Munoz-Couselo E, Mortier L, Bratland Å, Gutzmer R, Roshdy O, et al. Pembrolizumab for locally advanced and recurrent/metastatic cutaneous squamous cell carcinoma (KEYNOTE-629 study): an open-label, nonrandomized, multicenter, phase II trial. Ann Oncol. 2021;32(10):1276–85. https://doi.org/10.1016/j.annonc.2021.07.008.
Munhoz RR, Nader-Marta G, de Camargo VP, Queiroz MM, Cury-Martins J, Ricci H, et al. A phase 2 study of first-line nivolumab in patients with locally advanced or metastatic cutaneous squamous-cell carcinoma. Cancer. 2022;128(24):4223–31. https://doi.org/10.1002/cncr.34463.
Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366(23):2171–9. https://doi.org/10.1056/NEJMoa1113713.
Migden MR, Guminski A, Gutzmer R, Dirix L, Lewis KD, Combemale P, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16(6):716–28. https://doi.org/10.1016/S1470-2045(15)70100-2.
Stratigos AJ, Sekulic A, Peris K, Bechter O, Prey S, Kaatz M, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):848–57. https://doi.org/10.1016/S1470-2045(21)00126-1.
Chang ALS, Tran DC, Cannon JGD, Li S, Jeng M, Patel R, et al. Pembrolizumab for advanced basal cell carcinoma: an investigator-initiated, proof-of-concept study. J Am Acad Dermatol. 2019;80(2):564–6. https://doi.org/10.1016/j.jaad.2018.08.017.
D’Angelo SP, Hunger M, Brohl AS, Nghiem P, Bhatia S, Hamid O, et al. Early objective response to avelumab treatment is associated with improved overall survival in patients with metastatic Merkel cell carcinoma. Cancer Immunol Immunother. 2019;68(4):609–18. https://doi.org/10.1007/s00262-018-02295-4.
Gonzalez-Cao M, Puertolas T, Manzano JL, Maldonado C, Yelamos O, Berciano-Guerrero MÁ, et al. Access to melanoma drugs in Spain: a cross-sectional survey. Clin Transl Oncol. 2024. https://doi.org/10.1007/s12094-024-03501-9.
Acknowledgements
The authors acknowledge Stephanie Davis for her assistance in language revision.
Funding
There were no funding sources.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
None.
Research involving human participants and/or animals
This article does not conatiin any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cerezuela-Fuentes, P., Gonzalez-Cao, M., Puertolas, T. et al. Access to systemic treatment of non-melanoma skin cancer in Spain: a survey analysis. Clin Transl Oncol (2024). https://doi.org/10.1007/s12094-024-03583-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12094-024-03583-5