Abstract
Purpose
We investigated the effect of boost radiation therapy (RT) in addition to whole pelvis RT (WPRT) on treatment outcome and safety of cervical cancer patients following hysterectomy with close/positive resection margins (RM).
Methods
We retrospectively analyzed 51 patients with cervical cancer who received WPRT with or without boost-RT as adjuvant treatment between July 2006 and June 2022. Twenty patients (39.2%) were treated with WPRT-alone, and 31 (60.8%) received boost-RT after WPRT using brachytherapy or intensity-modulated RT.
Results
The median follow-up period was 41 months. According to RT modality, the 4-year local control (LC) and locoregional control (LRC) rates of patients treated with WPRT-alone were 61% and 61%, respectively, whereas those in LC and LRC rates in patients who underwent WPRT with boost-RT were 93.2% and 75.3%, with p-values equal to 0.005 and 0.090, respectively. Seven patients (35.0%) had local recurrence in the WPRT-treated group compared to only two out of the 31 patients (6.5%) in the WPRT with boost-RT-treated counterparts (p = 0.025). Boost-RT was a significantly good prognostic factor for LC (p = 0.013) and LRC (p = 0.013). Boost-RT did not result in statistically-significant improvements in progression-free survival or overall survival. The acute and late toxicity rates were not significantly different between groups.
Conclusion
Boost RT following WPRT is a safe and effective treatment strategy to improve LC without increasing toxicity in patients with cervical cancer with close/positive RM after hysterectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When cervical cancer is treated by surgery alone, the risk of recurrence is up to 10% in the early stage and up to 40% in the locally advanced stage [1,2,3]. Identifying which patient subgroups have high recurrence risks and providing adjuvant treatments (ATs) accordingly is therefore necessary. Pathologic features such as lymph node (LN) metastasis, positive resection margin (RM), and parametrial involvement are major risk factors for cancer recurrence following primary surgical treatment [4]. In particular, positive RM is an important risk factor for local recurrence [5]. The influence of RM status and adjuvant radiation therapy (RT) on recurrence in cervical cancer was reported by Viswanathan et al. [6]. Progression-free survival (PFS) rates were 11%, 20%, and 38% for cervical cancer with negative, close, and positive RM, respectively. Adjuvant RT decreased the local recurrence rate from 10 to 0%, 17% to 0%, and 50% to 25% for negative, close, and positive RMs, respectively. Close/positive RMs of both the parametrial and vaginal sides remain major risk factors for local recurrence even when patients are treated with adjuvant RT [6, 7]. Therefore, additional treatments to improve local control (LC) should be considered in patients with close/positive RM following whole pelvis RT (WPRT), but the optimal AT strategy remains unclear. The American Brachytherapy Society guidelines state that “there is no clear agreement to indications” but recommends the consideration of boost-RT using brachytherapy for patients with close/positive RM [8]. The National Comprehensive Cancer Network (NCCN) guidelines recommend individualized decisions regarding brachytherapy in close/positive vaginal RM; however, there are no comments concerning close/positive parametrial RM [9].
To determine the optimal treatment strategy for cervical cancer patients with close/positive RM, we evaluated the treatment outcome and toxicity of employing adjuvant WPRT with/without boost-RT.
Materials and methods
Patients
Cervical cancer patients who received adjuvant RT at our institution between July 2006 and June 2022 were evaluated. The inclusion criteria were as follows: (1) hysterectomy and histologically proven primary cervical cancer; (2) confirmation of either close (safety margin < 5 mm) or positive RM of parametrial and/or vaginal sides on pathology; and (3) received WPRT with or without boost-RT as AT. Fifty-nine patients with cervical cancer with close/positive RM underwent adjuvant WPRT. The exclusion criteria were: (1) achieved negative RM with re-excision, (2) macroscopic residual tumor after hysterectomy (R2 resection), and (3) no follow-up after irradiation treatment. Eight patients were excluded from the study. This study was approved by the institutional review board of the Catholic Medical Center ethics committee (reference number: OC22RASI0154). All data were retrieved from medical reports and our institutional records.
Treatment
Radical hysterectomy was performed on 46 patients (90.2%); the remaining five patients (9.8%) underwent simple hysterectomy. Forty-one patients (80.4%) underwent pelvic LN dissection. Para-aortic LNs were sampled in 21 patients (41.2%).
Adjuvant WPRT was initiated 4–6 weeks after the hysterectomy. The vaginal stump, paravaginal soft tissue, and regional pelvic lymphatics, including the internal, external, common iliac, and presacral lymphatics, were defined as planning target volume. Para-aortic lymphatic was also included in the RT field with the identification of metastasis. The median total dose of WPRT was 5040 cGy (range: 4500–5580 cGy) in 28 fractions (range: 25–31 fractions). WPRT was delivered using three-dimensional conformal RT or intensity-modulated RT (IMRT). Thirty-eight patients (74.5%) received concurrent chemotherapy (CT). The most prevalent regimen for CT was weekly cisplatin (40 mg/m2).
Twenty patients (39.2%) underwent WPRT exclusive, and 31 (60.8%) received WPRT with boost-RT using brachytherapy or IMRT. Whether/how to use boost-RT was decided by the attending physicians. Brachytherapy boost was primarily used for close/positive RM of the vagina or both vagina and parametrium, and IMRT boost was mainly used for close/positive RM of the parametrium. Brachytherapy using Ir-192 was delivered in 27 patients, with a median dose of 2500 cGy (range: 1200–3500 cGy) in 5 fractions (range: 2–6 fractions). Most patients were treated with 2000–3000 cGy in 5–6 fractions. The radiation dose was prescribed at 0.5 cm depth from the surface of the cylinder, and the treatment length was the upper 2–3 cm of the vagina. It was administered 2–3 times weekly with at least 48 h between fractions. IMRT boost was performed in four patients with a median of 1500 cGy (range: 900–3500 cGy) in 7.5 fractions (range: 5–10 fractions). The vaginal stump and paravaginal soft tissue were the targets of IMRT boost.
Statistical analyses
The Kaplan–Meier method was used to estimate LC, locoregional control (LRC), PFS, and overall survival (OS). LC was defined as the absence of vaginal stump recurrence. LRC was defined as the absence of any recurrence within the radiation field. PFS was defined as the duration from the date of hysterectomy to the date of first recurrence of disease or last follow-up visit. OS was defined as the time from the date of hysterectomy to any-cause death or last follow-up visit. Univariate analyses were performed using the Cox regression model to assess prognostic factors related to disease control/survival. Potential prognostic factors (p < 0.1) in the univariate analyses were included in the multivariate analyses. The latter analyses were performed using the Cox proportional hazards model. All test results were two-sided. Statistical significance was set at p < 0.05. All statistical analyses were performed using R software version 4.2.1.
Treatment-related toxicities were recorded and analyzed according to the Common Terminology Criteria for Adverse Events version 5.0 [10]. Toxicities occurring within 90/after 90 days of RT completion were considered acute/late toxicities, respectively.
Results
Patient and tumor characteristics
Baseline patient, disease, and treatment characteristics are summarized in Table 1. Tumor staging was performed according to the 2018 International Federation of Obstetrics and Gynecology (FIGO) staging system [11]. FIGO Stage IIIC disease with pelvic and/or para-aortic LN involvement was most common (n = 22, 43.1%). The main histological type was squamous cell carcinoma (SCC) (n = 39, 76.5%), and the remaining were adenocarcinomas or adenosquamous carcinomas (n = 12, 23.5%). Nineteen patients (37.3%) had close/positive parametrial RM, and 42 (82.4%) had close/positive vaginal RM. Ten patients (19.6%) had close/positive parametrial and vaginal RM.
Only the status of vaginal RM showed a significant difference between the two treatment modality groups. The patients with close/positive vaginal RM received boost-RT more frequently than those with negative vaginal RM (p = 0.003).
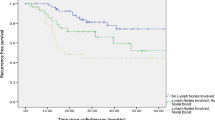
Treatment outcomes and pattern of failure
The median follow-up period was 41 months (range: 6–166 months). The 4-year LC, LRC, PFS, and OS rates were 81.2%, 69.5%, 64.5%, and 75.2%, respectively. According to RT modality, the 4-year LC, LRC, PFS, and OS rates of patients treated by WPRT-alone were 61%, 61%, 61%, and 71.5%, respectively, whereas these rates in patients who underwent WPRT with boost RT treatment were 93.2%, 75.3%, 67.5%, and 77.3%, respectively (p = 0.005, p = 0.090, p = 0.400, and p = 0.500, respectively) (Fig. 1).
During the follow-up period, 17 patients (33.3%) experienced disease recurrence. The patterns of failure at the time of the first recurrence are shown in Table 2. Cancer spread to multiple sites simultaneously in some patients. The median interval of recurrence was 13 months (range: 5–114 months). Seven patients (35.0%) had local recurrence in the WPRT-alone group, whereas only 2/31 patients (6.5%) had local relapse in the WPRT with boost-RT group (p = 0.025). However, distant recurrence at the time of the first counterpart was only found in the WPRT with boost-RT group (29.0%) compared to the WPRT-alone group (0.0%; p = 0.023).
Prognostic factors
Prognostic factors associated with disease recurrence and survival were analyzed. Detailed analysis results of the prognostic factors for LC and LRC are shown in Table 3. Boost-RT after WPRT remained a strong predictor of better LC (hazard ratio [HR]: 0.09, 95% confidence interval [CI] 0.01–0.60; p = 0.013) and LRC (HR: 0.04, 95% CI 0.00–0.52; p = 0.013) by multivariate analysis. The presence of LN metastasis was also an important prognostic factor for worse LC (HR: 12.42, 95% CI 1.12–138.13; p = 0.040 for para-aortic LN) and LRC (HR: 15.12, 95% CI 1.17–194.80; p = 0.037 for pelvic LN, HR: 784.70, 95% CI 7.34–83,860.00; p = 0.005 for para-aortic LN). Furthermore, large primary tumors (HR: 27.27, 95% CI 2.23–333.00; p = 0.010) and deep stromal invasion (DSI; HR: 5.49, 95% CI 1.30–23.12; p = 0.020) were also associated with worse LRC.
Analysis of the prognostic factors of PFS and OS are summarized in Table 4. Poorly differentiated (PD) carcinoma and DSI were independent poor prognostic factors influencing PFS (HR: 9.62, 95% CI 2.27–40.78; p = 0.002 for PD, HR: 4.61; 95% CI 1.51–14.09; p = 0.007 for DSI) and OS (HR: 4.72, 95% CI 1.56–14.33; p = 0.006 for PD, HR: 2.82; 95% CI 1.01–7.92; p = 0.048 for DSI). SCC histology was a good prognostic factor for PFS (HR: 0.15, 95% CI 0.04–0.58; p = 0.006).
Toxicity
The treatment was tolerated in all patients who received either WPRT with/without boost-RT. As shown in Table 5, 15 patients (29.4%) experienced Grade 2 acute toxicity. No acute toxicity ≥ Grade 3 was observed. Three patients experienced both gastrointestinal and genitourinary toxicities. The former was observed in nine (17.6%) patients, including proctitis (seven) and nausea (two). Genitourinary toxicity was observed in nine (17.6%) patients, including cystitis (six) and urinary frequency (three). Although the incidence of acute toxicity in patients treated by WPRT with boost-RT (35.5%) was higher than that of WPRT-alone (20.0%), the difference was not statistically-significant (p = 0.384).
Eight (15.7%) patients developed Grade 2 late toxicities, half of which were associated with acute toxicity, and the rest being newly-developed. Late toxicity included proctitis in two (3.9%), urinary incontinence in two (3.9%), and cystitis in four (7.9%). There was no late toxicity of ≥ Grade 3, such as fistula formation or urinary tract stricture. The incidence of late toxicity was higher in the WPRT with boost-RT group (19.3%) compared to the WPRT-alone group (10.0%), but the difference was not statistically-significant (p = 0.615).
Discussion
The optimal AT strategy for cervical cancer patients with close/positive RM following surgery remains unclear. Current treatment guidelines recommend boost-RT using brachytherapy as a treatment option [8, 9]. To establish the effect of boost-RT, we compared the treatment outcomes and toxicities of WPRT with/without boost-RT in patients with close/positive RM. Boost-RT was associated with improvements in LC and LRC, and all toxicities observed were at clinically-acceptable levels. The incidence of acute and late toxicities was not significantly different between the two groups.
Our results regarding the effect of boost-RT in the AT setting after hysterectomy are consistent with prior studies [12, 13]. Lee et al. investigated differences in treatment outcomes using adjuvant WPRT with/without brachytherapy in patients with close/positive vaginal RM [13]. The 5-year LC rate was significantly higher in the WPRT with brachytherapy group than in the WPRT-alone counterpart (100% vs. 81.3%, p = 0.022). The acute and late toxicity rates were not significantly different. Ager et al. evaluated the impact of brachytherapy boost and dose-escalated external-beam-RT (EBRT) on OS in patients with positive RM following hysterectomy, using the National Cancer Database [14]. The addition of brachytherapy to WPRT significantly improved OS compared to WPRT-alone. Three-year OS was 73% and 81% for patients who received WPRT-alone and WPRT with brachytherapy, respectively (p = 0.017). However, dose-escalated EBRT was not associated with OS improvement (p = 0.450). Since dose-escalated EBRT was simply defined as 5040 cGy or more, it is believed that a considerable number of patients in the dose-escalation group could not receive a sufficient dose to improve OS.
The 4-year PFS rates of the patients who received WPRT-alone and WPRT with boost-RT were 61% and 67.5%, respectively, and their OS rates were 71.5% and 77.3%, respectively. Although a sufficient dose of boost-RT improved LC and LRC, it did not result in statistically-significant improvements in PFS or OS. There are two potential reasons for this. First, the sample size may have been too small. Second, the addition of boost-RT may have changed the pattern of failure. The main failure pattern in patients receiving WPRT-alone was a local recurrence, whereas in patients receiving WPRT with boost-RT, it was a distant recurrence. The incidence of distant recurrence was higher in the boost-RT group. These results are consistent with those of previous studies. The predominant failure pattern after WPRT-alone is locoregional failure [15]. Although locoregional failure is reduced, distant failure accounts for most treatment failures among patients receiving WPRT with boost-RT [12, 16]. Lee et al. also reported more distant recurrence after treatment with WPRT with boost-RT (13.4%) than with WPRT-alone (6.7%), although the difference was not statistically-significant (p = 0.671) [13].
Based on these findings, additional CT may play an important role in controlling distant metastasis in patients with improved LC and LRC by boost-RT. This would lead to improvements in OS by lowering distant metastasis, especially in patients at high risk of recurrence. To test this hypothesis directly, the GOG 724 trial, which evaluates high-risk patients after surgery, randomly allocated to receive either concurrent chemoradiation therapy (CCRT) -alone or CCRT followed by additional CT, has been ongoing since 2009 [17].
Furthermore, we identified other prognostic factors associated with disease control/survival, besides RT modality. LN status is also a significant prognostic factor for LC and LRC. Many studies have clearly identified LN metastasis as a major risk factor [18,19,20]. Koh et al. documented that ~ 40% of patients with LN metastasis experienced pelvic recurrence [21]. Although LN status was not associated with PFS or OS in this study, it was confirmed that OS of cervical cancer patients decreased with increasing numbers of positive LNs [22]. Primary tumor size and depth of invasion (DOI) were also prognostic factors for LRC. Histological type, DOI, and differentiation grade were independent prognostic factors for PFS and/or OS. Adenocarcinoma and adenosquamous carcinoma have been associated with poorer prognoses than SCC in cervical cancer [23]. A large primary tumor and DSI are known to be intermediate prognostic factors that increase recurrence risk when combined with lymphovascular space invasion (LVSI), confirmed to be a significant prognostic factor only in the univariate analysis in this study, rather than increasing the recurrence rate by itself [24, 25]. Ryu et al. showed that adenocarcinoma, large primary tumor size, DSI, and LVSI were associated with disease recurrence and designed recurrence-predicting modeling using these four factors. The presence of any two may be useful for predicting disease recurrence [26]. Other researchers have also confirmed that PD carcinoma is associated with poor treatment outcomes [27, 28].
In addition to its retrospective nature, this study has some limitations. A selection bias may have been introduced by physicians when selecting the AT modality. CCRT is currently the standard treatment for patients with close/positive RM; however, 25% of the patients were treated with RT alone without concurrent CT. This may have affected the treatment outcomes. This study included a relatively small number of patients, which may have affected the result generalizability. Despite these, this study suggests the feasibility of boost-RT following WPRT in patients with close/positive RM following hysterectomy.
Conclusion
WPRT with boost-RT improved LC and LRC without increasing toxicity in cervical cancer patients with close/positive RM after hysterectomy. Our findings support the current treatment guidelines for adding boost-RT after WPRT as an AT for patients with close/positive RM margins. However, the main pattern of failure changed from local recurrence to distant recurrence after boost-RT, which did not improve the PFS or OS to the expected extent. Our results further confirmed that the already-known high and intermediate risk factors for recurrence and survival, such as histologic type, grade of differentiation, primary tumor size, DOI, and LN metastasis were valid in patients with close/positive RM. Based on these findings, additional CT may play an important role in controlling distant metastasis in patients with improved LC and LRC after boost-RT. This could lead to improvements in OS, particularly in patients with poor prognostic factors.
Data availability
Data are available upon reasonable request.
References
Zhao H, He Y, Yang SL, Zhao Q, Wu YM. Neoadjuvant chemotherapy with radical surgery vs radical surgery alone for cervical cancer: a systematic review and meta-analysis. Onco Targets Ther. 2019;12:1881–91.
Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–904.
Uppal S, Gehrig PA, Peng K, Bixel KL, Matsuo K, Vetter MH, et al. Recurrence rates in patients with cervical cancer treated with abdominal versus minimally invasive radical hysterectomy: a multi-institutional retrospective review study. J Clin Oncol. 2020;38:1030–40.
Samlal RA, van der Velden J, Schilthuis MS, González González D, Ten Kate FJ, Hart AA, et al. Identification of high-risk groups among node-positive patients with stage IB and IIA cervical carcinoma. Gynecol Oncol. 1997;64:463–7.
Orosco RK, Tapia VJ, Califano JA, Clary B, Cohen EEW, Kane C, et al. Positive surgical margins in the 10 most common solid cancers. Sci Rep. 2018;8:5686.
Viswanathan AN, Lee H, Hanson E, Berkowitz RS, Crum CP. Influence of margin status and radiation on recurrence after radical hysterectomy in Stage IB cervical cancer. Int J Radiat Oncol Biol Phys. 2006;65:1501–7.
Kim YJ, Lee KJ, Park KR, Kim J, Jung W, Lee R, et al. Prognostic analysis of uterine cervical cancer treated with postoperative radiotherapy: importance of positive or close parametrial resection margin. Radiat Oncol J. 2015;33:109–16.
Small W Jr, Beriwal S, Demanes DJ, Dusenbery KE, Eifel P, Erickson B, et al. American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. Brachytherapy. 2012;11:58–67.
National Comprehensive Cancer Network. Cervical cancer (Version 1.2023). 2023. https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 15 Jan 2023.
National Cancer Institute. Common Terminology Criteria for Adverse Events v5.0. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf. Accessed 15 Jan 2023.
Lee SI, Atri M. 2018 FIGO staging system for uterine cervical cancer: enter cross-sectional imaging. Radiology. 2019;292:15–24.
Kim D, Ki Y, Kim W, Park D, Lee J, Lee J, et al. Adjuvant external beam radiation and brachytherapy for vaginal resection margin positive cervical cancer. Radiat Oncol J. 2018;36:147–52.
Lee YH, Kim YS, Choi KH, Sung S, Jeong BK, Ha IB, et al. Comparison of treatment outcomes of pelvis external radiotherapy with and without vaginal brachytherapy for cervical cancer patients with positive or close vaginal resected margins. Int J Clin Oncol. 2022;27:202–12.
Ager BJ, Torgeson A, Francis SR, Burt LM, Gaffney DK, Cannon DM. Impact of brachytherapy boost and dose-escalated external beam radiotherapy in margin positive cervical cancer treated with chemotherapy and radiation. Am J Clin Oncol. 2020;43:35–42.
Stock RG, Chen AS, Flickinger JC, Kalnicki S, Seski J. Node-positive cervical cancer: impact of pelvic irradiation and patterns of failure. Int J Radiat Oncol Biol Phys. 1995;31:31–6.
Contreras J, Srivastava A, Chundury A, Schwarz JK, Markovina S, Thaker PH, et al. Long-term outcomes of intensity-modulated radiation therapy (IMRT) and high dose rate brachytherapy as adjuvant therapy after radical hysterectomy for cervical cancer. Int J Gynecol Cancer. 2020;30:1157–61.
Gynecologic Oncology Group. Chemotherapy and pelvic radiation therapy with or without additional chemotherapy in treating patients with high-risk early-stage cervical cancer after radical hysterectomy. NLM identifier: NCT00980954. https://clinicaltrials.gov/ct2/show/NCT00980954 Accessed 10 Jan 2023.
Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, et al. Multivariate analysis of histopathologic prognostic factors for invasive cervical cancer treated with radical hysterectomy and systematic retroperitoneal lymphadenectomy. Acta Obstet Gynecol Scand. 2002;81:1144–51.
Kamura T, Tsukamoto N, Tsuruchi N, Saito T, Matsuyama T, Akazawa K, et al. Multivariate analysis of the histopathologic prognostic factors of cervical cancer in patients undergoing radical hysterectomy. Cancer. 1992;69:181–6.
Du R, Li L, Ma S, Tan X, Zhong S, Wu M. Lymph nodes metastasis in cervical cancer: incidences, risk factors, consequences and imaging evaluations. Asia Pac J Clin Oncol. 2018;14:e380–5.
Koh WJ, Panwala K, Greer B. Adjuvant therapy for high-risk, early stage cervical cancer. Semin Radiat Oncol. 2000;10:51–60.
Guo Q, Zhu J, Wu Y, Wen H, Xia L, Ju X, et al. Validation of the prognostic value of various lymph node staging systems for cervical squamous cell carcinoma following radical surgery: a single-center analysis of 3732 patients. Ann Transl Med. 2020;8:485.
Lai CH, Hsueh S, Hong JH, Chang TC, Tseng CJ, Chou HH, et al. Are adenocarcinomas and adenosquamous carcinomas different from squamous carcinomas in stage IB and II cervical cancer patients undergoing primary radical surgery? Int J Gynecol Cancer. 1999;9:28–36.
Van de Putte G, Lie AK, Vach W, Baekelandt M, Kristensen GB. Risk grouping in stage IB squamous cell cervical carcinoma. Gynecol Oncol. 2005;99:106–12.
Takekuma M, Kasamatsu Y, Kado N, Kuji S, Tanaka A, Takahashi N, et al. The issues regarding postoperative adjuvant therapy and prognostic risk factors for patients with stage I-II cervical cancer: a review. J Obstet Gynaecol Res. 2017;43:617–26.
Ryu SY, Kim MH, Nam BH, Lee TS, Song ES, Park CY, et al. Intermediate-risk grouping of cervical cancer patients treated with radical hysterectomy: a Korean gynecologic oncology group study. Br J Cancer. 2014;110:278–85.
Landoni F, Maneo A, Cormio G, Perego P, Milani R, Caruso O, et al. Class II versus class III radical hysterectomy in stage IB-IIA cervical cancer: a prospective randomized study. Gynecol Oncol. 2001;80:3–12.
Matsuo K, Mandelbaum RS, Machida H, Purushotham S, Grubbs BH, Roman LD, et al. Association of tumor differentiation grade and survival of women with squamous cell carcinoma of the uterine cervix. J Gynecol Oncol. 2018. https://doi.org/10.3802/jgo.2018.29.e91.
Author information
Authors and Affiliations
Contributions
HJK contributed to the study conception and design. Material preparation, data collection and analysis were performed by HJK, MK, Y-KK, and SJL. The first draft of the manuscript was written by SJL. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was approved by the institutional review board of the Catholic Medical Center ethics committee (IRB No.: OC22RASI0154).
Informed consent
No informed consent was required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, S.J., Kim, M., Kwak, YK. et al. The impact of boost radiation therapy after hysterectomy on cervical cancer patients with close or positive resection margins. Clin Transl Oncol 26, 689–697 (2024). https://doi.org/10.1007/s12094-023-03283-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03283-6