Abstract
Background
Irinotecan and temozolomide (IT) is a widely used regimen for relapsed Ewing sarcoma (ES), although studies are largely limited to paediatric populations.
Methods
We retrospectively reviewed paediatric (< 18 years) and adult patients (≥ 18 years) treated with salvage IT at two institutions. Haematologic toxicities were graded according to common terminology criteria of adverse events. Survival was estimated by the Kaplan–Meier method and compared by the Log Rank test.
Results
Fifty-three patients were treated with IT from Jan, 2010 to Dec, 2018 (n = 16 paediatric; n = 37 adult). IT was given as second-line (n = 34; 64%) or ≥ third-line (n = 19; 36%). There was no difference in ≥ grade 3/4 haematologic toxicity between paediatrics and adults (31% vs. 35% respectively; p = 0.76). The frequency of diarrhoea of any grade was similar (38% in each group). Of 43 patients assessable for response, 12 (28%) had objective response (1 CR, 11 PR), 12 (28%) stable disease and 19 (44%) disease progression. Objective response rate did not differ between the two groups (36% in paediatrics vs. 25% in adults; p = 0.47). Median PFS was superior in paediatrics vs. adults (7.4 vs. 2.2 months, p = 0.039).
Conclusion
Irinotecan and temozolomide (IT) chemotherapy has activity for relapsed ES, with favourable toxicity and equally observed objective responses in the paediatric and adult populations. The observed superior PFS for the paediatric cohort requires further confirmation in future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ewing sarcoma (ES) is a highly malignant neoplasm that accounts for 10–15% of primary bone tumours and is the second most common bone malignancy in childhood [1, 2]. Standard therapy for primary localized ES involves a multimodal approach that include multiagent chemotherapy and surgery (and/ or radiation). Five-year event-free survival (EFS) rates with this approach approximate 70–75% [2]. Historically, chemotherapy for ES has consisted of anthracyclines and alkylating agents. The outcomes of primary localized ES have improved with modification of this chemotherapy backbone by adding ifosfamide and etoposide (IE) into the three-drug combination of vincristine, doxorubicin and cyclophosphamide (VDC), given as alternating cycles of IE and VDC every 3 weeks [3]. Compression of the interval between treatment courses from 3 to 2 weeks with use of granulocyte colony-stimulating factor (G-CSF) support has resulted in additional improvement in EFS rates [4]. In Europe, the initial chemotherapy regimen consists of vincristine, ifosfamide, doxorubicin and etoposide (VIDE regimen) [5]. However, interim results of the Euro Ewing 2012 (EE2012) randomized trial have demonstrated improved outcomes using VDC-IE as the chemotherapy backbone [6].
Relapse following primary therapy is associated with a poor prognosis, with an estimated 5-year overall survival (OS) and EFS of 10–20% and 5–10%, respectively [7,8,9]. Tumor volume > 200 ml, location in the pelvis, and age > 14 years are among the established adverse prognostic factors for primary localized disease [1]. Metastatic disease at presentation is also associated with poor prognosis for the majority of patients, especially after progression on standard VDC-IE chemotherapy [1, 7].
Early studies with irinotecan have shown promising single agent activity in patients with relapsed ES [10, 11]. Studies have demonstrated enhanced activity and acceptable toxicity profile by addition of temozolomide to irinotecan in paediatric patients who relapse following VDC-IE [8, 12, 13]. However, there is significant variability in the schedule and dosing of irinotecan, with doses ranging from 10 to 50 mg/m2 administered on day 1–5 only or 10–20 mg/m2 administered on day 1–5 and day 8–12. The overall response rate (ORR) with the irinotecan and temozolomide (IT) regimen in ES has been reported in the range of 29–63% [8, 12, 13]. Preclinical data have suggested a synergistic rather than an additive effect for the combination [14, 15]. However, majority of studies that assessed the IT regimen have been conducted in paediatric populations with small sample sizes [8, 12, 13].
Given the limited data on IT regimen in adult patients, we aimed to compare the tolerability and efficacy of IT between paediatric and adult populations across two institutions.
Materials and methods
Patients
Eligible patients had a diagnosis of ES treated and followed up at two institutions: The King Hussein Cancer Centre, Amman, Jordan, and the Peter MacCallum Cancer Centre, Melbourne, Australia. Patients were required to have relapsed or progressive disease after VDC-IE chemotherapy for localized or metastatic disease and to have initiated IT chemotherapy (≥ second-line) between January, 2010 and December, 2018. Patients were identified at each of the two institutions through electronic chemotherapy prescription records. Chemotherapy prescription records after local Human Research Ethics Committee approval (18 KHCC 06; PMCC 18/145). Consent waiver was granted given the retrospective nature of the study.
All cases were diagnosed after careful histologic examination of the hematoxylin and eosin-stained slides along with supportive immunohistochemical stains (IHC) at both institutions, as per standard of care. Essentially, a panel of IHC stains were performed to confirm the diagnosis (e.g. diffuse and strong membranous staining for CD99) and exclude other tumors that may have similar histomorphology. In cases where there was any uncertainty regarding the diagnosis, molecular confirmation for the presence of EWSR1 gene translocation by Flourescent Insitu Hybridization (FISH) study was performed.
The following data were collected from the electronic medical records: age, sex, primary tumour sites, stage at initial diagnosis, sites of disease relapse, the interval from prior chemotherapy (defined as the time from last chemotherapy cycle of the prior chemotherapy to the date of initiation of first cycle of the IT regimen), irinotecan dose and schedule, temozolomide dose, number of cycles, and best response to IT chemotherapy. In addition, blood counts prior to each cycle were reviewed, and haematologic toxicities were graded according to common terminology criteria of adverse events (CTCAE v. 4.03). The occurrences of non-haematologic toxicities were also documented based on case file review. Furthermore, data on any dose reductions, delays, or hospitalizations secondary to chemotherapy were obtained. Dates of first progression following initiation of IT chemotherapy and dates of last follow-up and death were also documented. Data collection commenced following acquisition of institutional review board approval at each of the two institutions.
Outcomes and definitions
Progression-free survival (PFS) was defined as the time from initiation of the first cycle of IT chemotherapy to the first documentation of disease progression, last follow-up or death. In the event of a patient being lost to follow-up, this was regarded as a censoring event and not an event of interest. Overall response rate (ORR) was defined as the percentage of patients assessable for response who achieve partial response (PR) or complete response (CR) following IT chemotherapy. Paediatric age group was defined as patients aged < 18 years at time of initiation of IT chemotherapy. Responses were assessed according to Response Evaluation Criteria in Solid Tumours (RECIST) version 1.1 Patients were required to have at least one measurable target lesion to be assessable for response according to RECIST. Measurable lesions that were irradiated were not selected as target lesions unless they had progressed following radiotherapy. Patients without measurable target lesion(s) at baseline were not assessable for response; however, they were included in PFS analysis. The outcomes of interest included ORR and PFS following IT chemotherapy in the overall eligible population and for comparison between the paediatric and adult patients. Comparisons were made in the frequency of hematologic toxicities and diarrhoea by age group, irinotecan dose and schedule.
Imaging studies
Response to IT chemotherapy was assessed with computed tomography (CT) scan or magnetic resonance imaging (MRI) following each two cycles of IT. CT was the imaging modality used to assess response in the lungs, whereas MRI was performed to assess response of tumours located in the extremities, spine, and pelvis. Following completion of chemotherapy, imaging studies were performed every 3 months or at the time of any report of symptoms that might suggest disease progression (DP).
Statistical analysis
Data are presented descriptively as proportions, means or medians as appropriate. PFS and OS were estimated by the Kaplan–Meier method and survival comparisons was carried out by the log rank test. All p values < 0.05 were considered statistically significant. Rates of toxicity were compared between adults and paediatric patients by the χ2 test.
Results
Patients
Between January, 2010 and December, 2018, we identified 53 patients (n = 16 paediatric; n = 37 adult) receiving combination IT regimen for relapsed ES following VDC-IE chemotherapy (34 patients were treated at King Hussein Cancer Center and 19 at Peter MacCallum Cancer Center). The diagnosis of 34 patients (64%); (20 at King Hussein Cancer Center and 14 at Peter MaccCallum Cancer Center) was molecularly confirmed by demonstration of EWSR1 translocation by FISH. All other patients had typical pathologic and IHC features that were sufficient for diagnosis. IT was given as second-line for 34 patients (64%) and as third-line or beyond in 19 (36%). The median age of patients was 20 (range 5–45 years).
A total of 236 cycles of IT chemotherapy were delivered (median = 4, range 1–7). At the time of initiation of IT, 11 patients had local recurrence of ES and 42 had distant metastasis (5 of them had both local and metastatic disease). Of the patients who initiated IT for systemic progression, lung was the most common site of progression (26 patients; 62%). Nine patients (21%) had bone metastasis and 7 (17%) had progression in multiple sites.
Chemotherapy
Patients received IT chemotherapy according to one of the following protocols: Protocol 1: TMZ 100 mg/m2 D1–D5, irinotecan 40 mg/m2 D1–D5. Repeat every 21 days (n = 33); Protocol 2: TMZ 100 mg/m2 D1–D5, irinotecan 50 mg/m2 D1–D5. Repeat every 21 days (n = 13); Protocol 3: TMZ 100 mg/m2 D1–D5, irinotecan 20 mg/m2 D1–D5, D8–D12. Repeat every 21 days (n = 7).
All patients received temozolomide at a dose of 100 mg/m2/ day D1–D5. Irinotecan was initiated at a dose of 40 mg/m2 D1–D5 in 21-day cycles in 24 patients, 50 mg/m2 D1–D5 in 21-day cycles in 23 patients, and 20 mg/m2 D1–D5 and D8–D12 in 6 patients. In total, 29 patients received < 250 mg/m2/cycle of irinotecan and 24 patients received ≥ 250 mg/m2/cycle. Of note, 26 (49%) adult patients received the lower irinotecan dosing compared to only three paediatric patients. Fifteen (28%) patients received cefixime prophylaxis, 34 (64%) did not receive antibiotic prophylaxis, and data were missing for four (8%). None of the patients received primary granulocyte-colony stimulating factor (GCSF) prophylaxis at initiation of IT chemotherapy. However, one patient required secondary GCSF prophylaxis in subsequent cycles for history of febrile neutropenia after the third cycle.
Efficacy
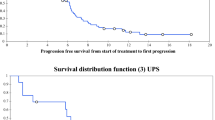
Fifty-two patients were assessable for PFS. One patient was excluded from PFS analysis due to incomplete follow-up data. The median PFS was 3.8 months, 6-month PFS was 39% (Fig. 1). Median PFS was superior in paediatrics vs. adults (7.4 vs. 2.2 months, p = 0.039) (Fig. 2). We further assessed PFS by line of therapy. In the second-line setting, PFS was 7.2 months for paediatric patients and 3.1 months for adults, p = 0.22, and in ≥ third-line PFS was 7.1 and 1.2 months, respectively, p = 0.087. Of note, we did not find any statistically significant difference in the median PFS based on time from prior chemotherapy (< 1 year vs. ≥ 1 year); 2.6 vs. 4.3 months, p = 0.98. The median OS was 14.1 months from the time of initiation of IT chemotherapy.
Ten patients (19%) were not assessable for response for absence of measurable target lesions that can be reliably followed and assessed by RECIST (six with bone metastasis, three with lung with pleural metastasis and one with bone and lung metastasis). Of the remaining 43 patients assessable for response, 12 (28%) had objective response (1 CR, 11 PR), 19 (44%) had disease progression and 12 (28%) had stable disease. There was no statistically significant difference in ORR between the two age groups (36% in paediatrics vs. 25% in adults; p = 0.47). Of the 27 patients who received IT in a second-line setting and are assessable for response, 8 (30%) had objective response, whereas 4 (24%) of 17 assessable patients who received IT in ≥ 3rd-line setting had objective response.
Among responders, median time from initiation of IT chemotherapy to response was 1.72 months ± 0.69 (range 1.0–2.9 months). Median number of cycles to achieve response was 2.5 ± 0.82 (range 2.0–4.0 cycles).
Following IT chemotherapy, five patients (10%) were candidates for consolidation therapy (surgery ± whole lung radiotherapy): one refused surgery given its morbidity and whole lung radiotherapy (WLRT), one underwent pulmonary metastasectomy and WLRT, two received WLRT, and the 5th underwent excision of local disease followed by adjuvant radiotherapy and WLRT. The patient who underwent metastasectomy + WLRT is alive without disease at 58 months and 55 months of initiation of IT and surgery, respectively, inspite of progressing during 2nd line ifosfamide and etoposide retreatment and receiving IT in a third-line setting. One patient who underwent consolidation WLRT remained free of progression for 18 months after initiation of IT, then subsequently underwent a hemipelvectomy for progression of local recurrence and is currently alive with disease at 22 months. The other two who received consolidation therapy had disease progression at 4 and 10 months. None of the patients were consolidated with high-dose chemotherapy and autologous stem cell transplant.
Toxicity
The IT regimen was well tolerated and toxicities requiring dose delay or leading to hospitalizations were rarely observed. Furthermore, less than 10% of patients had discontinued treatment due to toxicity (Table 1). At the time of analysis, three patients (6%) have ongoing treatment with IT chemotherapy. Twenty-five (47%) discontinued treatment for DP, 19 (36%) discontinued treatment because they have completed the planned number of cycles, 4 (8%) discontinued IT for toxicity, and 2 stopped chemotherapy given patient preference.
Haematologic toxicities of any grade occurred in 32 patients (60%). Haematological toxicities of grades ≥ 3 were observed in 18 patients (34%), with no statistically significant difference by age groups (Table 2).
Diarrhoea of any grade occurred in 20 patients (38%), 14 adults and 6 paediatrics (38% of patients in each group). We did not observe a statistically significant difference in the frequency of diarrhoea or severe haematologic toxicities by irinotecan dose (250 mg/m2/cycle vs. lower dose), (Table 3), or schedule (Table 4). However, there was a non-significant trend towards higher frequency of diarrhoea in the D1–D5 every 21-day schedule (Table 4). Cefixime prophylaxis against diarrhoea was given for 15 (28%) patients, whereas 34 (64%) did not receive cefixime, and data were missing for 4 (8%).
Discussion
Chemotherapy utilizing the VDC-IE has been a standard regimen in North America for primary localized ES [3]. VIDE regimen is considered another standard regimen in Europe [5]. However, there is no consensus on a standard regimen for ES patients who progress after VDC and IE chemotherapy or VIDE, mainly due to lack of data from randomized trials in that setting. In keeping with previous publication, the major findings of this study is that IT has activity as a salvage regimen in both paediatric and adult populations and associated with favourable toxicity profile. Nevertheless, outcomes following salvage regimens at relapse are discouraging with 5-year OS of ≤ 10% [16] and a median OS of 14 months within our study population.
A number of regimens have traditionally been used in the relapse setting with camptothecin-containing regimens being associated with modest efficacy [8, 12, 16,17,18,19]. An increase in response rates has been observed when camptothecins are combined with synergistic agents. Combination of topotecan and cyclophosphamide is an active regimen for relapsed ES, with reported ORR of 30–35%, which is consistent with the response rates observed for the IT regimen [19]. Other non-camptothecin based regimens have also demonstrated significant activity in relapsed ES. The activity of the ICE regimen was demonstrated in a Children’s Cancer Group trial of variety of sarcoma histologies including ES. In that trial, an objective response was observed in 48% of the 21 patients with relapsed ES [20].
Multiple phase I trials and case series have reported varying response rates associated with IT regimen in patients with relapsed ES. The Memorial Sloan-Kettering Cancer Centre has reported the highest ORR of 63% in a series of 19 patients [8]. However, consistent with our data, other studies have reported almost half of the response rate reported by the MSKCC group [12, 17, 21].
Data on efficacy and tolerability of IT chemotherapy in adult patients is limited. Blanchette et al. assessed the tolerability and efficacy of IT chemotherapy in 24 adult patients with variety of sarcomas including ES (n = 11; 46%) [22]. Consistent with data from our study, the frequencies of grade ≥ 3 anemia, neutropenia and thrombocytopenia were low (21%, 12%, and 4%, respectively). However, diarrhoea of any grade occurred in 50% of patients compared to 38% of our adult patients. The authors concluded that IT is active and tolerable in adults with ES and desmoplastic small round cell tumors. Palmerini et al. recently reported data for 51 patients treated with salvage IT, 34 (66%) of the patient population were adults [17]. Our study represents the second published study that has included both paediatric and adult patients (37 adult patients, 70%). Notably, 25% of patients in the data reported by Palmerini et al. received IT as the first salvage regimen after VDC-IE, whereas 64% of our patient population received IT as the first salvage regimen. Furthermore, 27% of the series reported by Palmerini received prior myeloablative therapy with busulfan and melphalan, which suggests a more heavily treated patient population compared to our reported patient population. Of note, grade 3–4 haematologic toxicities occurred at a lower proportion of patients in that case series compared to our study (e.g. grade 3–4 neutropenia 12% vs. 34% in our study). Nevertheless, chemotherapy was reasonably tolerated by both adults and paediatric in both studies and had rarely resulted in treatment discontinuation, hospitalizations or febrile neutropenia. However, contradicting with their data, our study showed superior PFS in the paediatric population, which requires confirmation from other studies.
Although data on the tolerability of the IT regimen in adult patients with ES are limited, there are other data that have assessed its tolerability in other cancer settings [23, 24]. However, tolerability of a particular regimen may vary among patients with different conditions and thus should be interpreted with caution.
A triplet regimen with vincristine added to irinotecan and temozolomide in paediatric patients with variety of tumours that included Ewing sarcoma (n = 15), rhabdomyosarcoma (n = 8), neuroblastoma (n = 8), osteosarcoma (n = 2) and Wilms’ tumor (n = 1), has also shown efficacy in ES patients, with an ORR of 40% [25].
There remains an unmet need to identify a standard regimen for relapsed ES, mainly due to absence of data from randomized trials. The rEECur trial (ISRCTN36453794) is a highly novel multi-arm multi-stage (MAMS) phase II/III “drop-a-loser” randomized trial in the relapsed ES that is currently comparing four regimens: topotecan and cyclophosphamide (TC), IT, gemcitabine and docetaxel and high-dose ifosfamide. The first analysis has shown inferior outcomes with gemcitabine and docetaxel, which has subsequently been dropped [26]. In the second interim analysis, IT was found to be less effective compared to TC and high-dose ifosfamide [27]. However, the trial is conducted in European countries where first-line VIDE chemotherapy is widely practiced and as such, whether IT is inferior to the other regimens after progression following VDC-IE chemotherapy remains unclear.
We acknowledge that the retrospective design might have biased the documentation of non-haematologic toxicity assessment. However, haematologic toxicity values in our study were accurate because these values are well documented in laboratory records prior to each cycle. Interestingly, the frequency of grades ≥ 3 haematologic toxicities was low in both paediatrics and adults in this heavily pre-treated population. Of note, the risk of febrile neutropenia was extremely low (two patients; 4%), although none of the patients received primary growth factor support prophylaxis. Diarrhoea was a common toxicity with IT regimen that was observed in 38% of patients, although other studies reported a higher frequency of diarrhoea of up to 50–60% of patients [21, 22]. Of note, we could not accurately grade the severity of diarrhoea given the retrospective design of the study. However, diarrhoea that was severe enough to require hospitalization was observed in only three patients (6%). Apart of the limitations of the retrospective design that affects reporting of non-haematologic toxicities, other limitations that we acknowledge are the small sample size and the heterogeneity of the different IT regimens used. These limitations can be overcome by international collaborative phase 2/3 trials.
The reason for the observed superior PFS in the paediatric population is unclear. This difference was observed regardless of line of therapy; however, IT was delivered as a later line of therapy in a higher proportion of adult patients and adult patients were more likely to receive a lower dose of irinotecan per cycle. Of note, there was no observed difference in PFS between adults and paediatrics in the data reported by Palmerini et al. [17].
In conclusion, our review of patients receiving IT has demonstrated that it is a well-tolerated and effective chemotherapy regimen for relapsed ES, with similarly observed favourable toxicity profile in adults and paediatric patients. Given our retrospective design, we eagerly await confirmation of the prospective rEEcur study that will test its effectiveness and tolerability versus other chemotherapy combinations. The sequencing of IT therapy and the optimal dose and schedule of irinotecan are other important areas that require future investigation.
References
Burchill SA. Ewing's sarcoma: diagnostic, prognostic, and therapeutic implications of molecular abnormalities. J Clin Pathol. 2003;56(2):96–102.
Potratz J, Dirksen U, Jürgens H, Craft A. Ewing sarcoma: clinical state-of-the-art. Pediatr Hematol Oncol. 2012;29(1):1–11.
Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med. 2003;348(8):694–701.
Womer RB, West DC, Krailo MD, et al. Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: a report from the Childrenʼs Oncology Group. J Clin Oncol. 2012;30(33):4148–54. https://doi.org/10.1200/JCO.2011.41.5703.
Juergens C, Weston C, Lewis I, et al. Safety assessment of intensive induction with vincristine, ifosfamide, doxorubicin, and etoposide (VIDE) in the treatment of Ewing tumors in the EURO-EWING 99 clinical trial. Pediatr Blood Cancer. 2006;47(1):22–9. https://doi.org/10.1002/pbc.20820.
Brennan B, Kirton L, Marec-Berard P, et al. Comparison of two chemotherapy regimens in Ewing sarcoma (ES): Overall and subgroup results of the Euro Ewing 2012 randomized trial (EE2012). J Clin Oncol. 2020;38(15_suppl):11500. https://doi.org/10.1200/JCO.2020.38.15_suppl.11500.
Ferrari S, Luksch R, Hall KS, et al. Post-relapse survival in patients with Ewing sarcoma. Pediatr Blood Cancer. 2015;62(6):994–9.
Casey DA, Wexler LH, Merchant MS, et al. Irinotecan and temozolomide for Ewing sarcoma: the Memorial Sloan-Kettering experience. Pediatr Blood Cancer. 2009;53(6):1029–34.
Leavey PJ, Mascarenhas L, Marina N, et al. Prognostic factors for patients with Ewing sarcoma (EWS) at first recurrence following multi-modality therapy: a report from the Children's Oncology Group. Pediatr Blood Cancer. 2008;51(3):334–8.
Cosetti M, Wexler LH, Calleja E, et al. Irinotecan for pediatric solid tumors: the Memorial Sloan-Kettering experience. J Pediatr Hematol Oncol. 2002;24(2):101–5.
Bisogno G, Riccardi R, Ruggiero A, et al. Phase II study of a protracted irinotecan schedule in children with refractory or recurrent soft tissue sarcoma. Cancer. 2006;106(3):703–7.
Wagner LM, McAllister N, Goldsby RE, et al. Temozolomide and intravenous irinotecan for treatment of advanced Ewing sarcoma. Pediatr Blood Cancer. 2007;48(2):132–9.
Kurucu N, Sari N, Ilhan IE. Irinotecan and temozolamide treatment for relapsed Ewing sarcoma: a single-center experience and review of the literature. Pediatr Hematol Oncol. 2015;32(1):50–9.
Houghton PJ, Stewart CF, Cheshire PJ, et al. Antitumor activity of temozolomide combined with irinotecan is partly independent of O6-methylguanine-DNA methyltransferase and mismatch repair phenotypes in xenograft models. Clin Cancer Res. 2000;6(10):4110–8.
Patel VJ, Elion GB, Houghton PJ, et al. Schedule-dependent activity of temozolomide plus CPT-11 against a human central nervous system tumor-derived xenograft. Clin Cancer Res. 2000;6(10):4154–7.
Huang M, Lucas K. Current therapeutic approaches in metastatic and recurrent Ewing sarcoma. Sarcoma. 2011;2011:863210.
Palmerini E, Jones RL, Setola E, et al. Irinotecan and temozolomide in recurrent Ewing sarcoma: an analysis in 51 adult and pediatric patients. Acta Oncol. 2018;57(7):958–64.
Farhat R, Raad R, Khoury NJ, et al. Cyclophosphamide and topotecan as first-line salvage therapy in patients with relapsed ewing sarcoma at a single institution. J Pediatr Hematol Oncol. 2013;35(5):356–60.
Hunold A, Weddeling N, Paulussen M, Ranft A, Liebscher C, Jürgens H. Topotecan and cyclophosphamide in patients with refractory or relapsed Ewing tumors. Pediatr Blood Cancer. 2006;47(6):795–800.
Van Winkle P, Angiolillo A, Krailo M, et al. Ifosfamide, carboplatin, and etoposide (ICE) reinduction chemotherapy in a large cohort of children and adolescents with recurrent/refractory sarcoma: the Children's Cancer Group (CCG) experience. Pediatr Blood Cancer. 2005;44(4):338–47.
Hernández-Marqués C, Lassaletta-Atienza A, Ruiz Hernández A, et al. Irinotecan plus temozolomide in refractory or relapsed pediatric solid tumors. An Pediatr (Barc). 2013;79(2):68–74.
Blanchette PS, Lo A, Ng P, et al. Irinotecan and temozolomide in adults with recurrent sarcoma. J Solid Tumors. 2015;5(2):105–11.
Gruber ML, Buster WP. Temozolomide in combination with irinotecan for treatment of recurrent malignant glioma. Am J Clin Oncol. 2004;27(1):33–8.
Vredenburgh JJ, Desjardins A, Reardon DA, Friedman HS. Experience with irinotecan for the treatment of malignant glioma. Neuro Oncol. 2009;11(1):80–91. https://doi.org/10.1215/15228517-2008-075.
Büyükkapu Bay S, Kebudi R, Görgün O, Zülfikar B, Darendeliler E, Çakır FB. Vincristine, irinotecan, and temozolomide treatment for refractory/relapsed pediatric solid tumors: a single center experience. J Oncol Pharm Pract. 2019;25(6):1343–8. https://doi.org/10.1177/1078155218790798.
Mccabe MG, Moroz V, Khan M, et al. Results of the first interim assessment of rEECur, an international randomized controlled trial of chemotherapy for the treatment of recurrent and primary refractory Ewing sarcoma. J Clin Oncol. 2019;37(15 suppl):11007. https://doi.org/10.1200/JCO.2019.37.15_suppl.11007.
McCabe MG, Kirton L, Khan M, et al. Results of the second interim assessment of rEECur, an international randomized controlled trial of chemotherapy for the treatment of recurrent and primary refractory Ewing sarcoma (RR-ES). J Clin Oncol. 2020;38(15 suppl):11502. https://doi.org/10.1200/jco.2020.38.15_suppl.11502.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of retrospective study, formal consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salah, S., To, Y.H., Khozouz, O. et al. Irinotecan and temozolomide chemotherapy in paediatric and adult populations with relapsed Ewing Sarcoma. Clin Transl Oncol 23, 757–763 (2021). https://doi.org/10.1007/s12094-020-02466-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02466-9