Abstract
Background
T cell therapy for cancer involves genetic introduction of a target-binding feature into autologous T cells, ex vivo expansion and single large bolus administration back to the patient. These reprogrammed T cells can be highly effective in killing cells, but tumor heterogeneity results in regrowth of cells that do not sufficiently express the single antigen being targeted. We describe a cell-based therapy that simultaneously targets multiple tumor-specific antigens.
Methods
High-affinity polyclonal rabbit antibodies were generated against nine different surface-related tumor-specific mutations on B16F10 cells. Unsorted splenic effector cells from syngeneic mice were incubated with a cocktail of the nine anti-B16F10 antibodies. These ‘armed’ effector cells were used to treat mice previously inoculated with B16F10 melanoma cells.
Results
The cocktail of nine antibodies resulted in dense homogeneous binding to histological sections of B16F10 cells. Five treatments with the armed effector cells and PD1 inhibition inhibited tumor growth and improved survival. Shortening the interval of the five treatments from every three days to every day increased survival. Arming effector cells with the four antibodies showing best binding to B16F10 cells even further increased survival.
Conclusions
This study demonstrates that ex vivo arming a mixed population of immune effector cells with antibodies targeting multiple tumor-specific mutated proteins in conjunction with PD1 inhibition delayed tumor growth and prolonged survival in mice inoculated with an aggressive melanoma. A remarkably low total antibody dose of less than 5 µg was sufficient to accomplish tumor inhibition. Scaling up to clinical level may be feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
T cell therapy was enabled when protocols to expand them ex vivo were developed [1]. This led to adoptive cell therapy using tumor-infiltrating lymphocytes (TILs) [2]. Dramatic responses in a some patients demonstrated the powerful capacity of T cells to inhibit tumors [3]. However, TIL products are not readily controlled. TILs delivered to the patient are a mix of T cell clones binding to unspecified targets. In many patients, TILs are not even recoverable [4]. Chimeric antigen receptor T cell therapy (CAR-T) is designed to gain greater control over the final product delivered to the patient. A binding element is introduced to T cells to direct therapy to a specific target.
Unlike TIL therapy, CAR-T cell therapy is largely limited to a single target [5]. This is a critical limitation that does not address the universal problem of tumor heterogeneity. In addition, targeting tumor-specific antigens by CAR-T cell therapy appears to not yet be possible and in most trials, the target is limited to tissue-specific targets such as CD19 [6]. Targeting CD19 or any other tissue-specific target will mediate cell death of normal cells along with tumor cells.
We present a new method of cell therapy that redirects multiple types of immune effector cells to multiple tumor-specific targets. Prior to delivery, effector cells are coated ex vivo with multiple antibodies targeting tumor-specific mutations. There are several potential advantages to this strategy. Simultaneously targeting multiple tumor-specific antigens may overcome the fundamental problem of tumor heterogeneity. Incubating effector cells ex vivo vastly reduces the amount of antibody required to cause tumor inhibition. Expansion of effector cells ex vivo is not required. We present the first preliminary data demonstrating tumor inhibition and increased survival in a mouse model with immune effector cells coated with antibodies targeting up to nine different tumor-specific antigens.
Methods
Reagents and cell line
B16F10 melanoma tumor cells were procured from the American Type Culture Collection (ATCC, Manassas, VA). Normal rabbit IgG was supplied by Sino Biological, Inc. (Wayne, PA). Alexa Fluor 568-conjugated goat anti-rabbit antibody was procured from Life Technologies (Carlsbad, CA). Anti-mouse PD1 inhibitor antibody (PD1i) was supplied by Bio X cell (West Lebanon, NH). Dulbecco’s Modified Eagle’s Medium (DMEM) and Trypsin–EDTA solution were purchased from ATCC. All other reagents used in this study were of molecular or high-purity grade.
Selection of tumor-specific mutated proteins and antibody production
We utilized confirmed sequence data of B16F10 mouse melanoma tumor cell line [7] and selected multiple cell surface-related mutated proteins with a single amino acid substitution. The 11-mer peptides representing the mutated region of the mutated proteins were designed, keeping the mutated amino acid residue in or near the center (Table 1). Peptide synthesis and production of affinity-enriched rabbit antibodies were purchased from GenScript (Piscataway, NJ).
Affinity estimations (EC50) of individual purified polyclonal antibodies for their respective mutated peptides were done by titering the samples using ELISA [8]. Individual mutated peptides were immobilized in flat-bottom clear MaxiSorp 96-well plates (Nunc, Rochester, NY) and after blocking the wells with 1% BSA in PBS, the plates were washed thrice with PBS. Serially diluted purified antibodies were incubated with the immobilized mutated peptides. HRP-conjugated anti-rabbit IgG antibodies and HRP substrate 3,3′,5,5′-tetramethylbenzidine (TMB) reagent (GenScript) were used for determining antibody binding to the mutated peptides. Following the color development, wells were read for their absorbance at 450 nm using a Synergy HT plate reader (BioTek Instruments, Inc. Winooski, VT).
Binding analysis of rabbit polyclonal antibodies by immunofluorescence microscopy
Frozen sections of mouse B16F10 tumor tissue mounted on glass slides were fixed in 3% paraformaldehyde (Electron Microscopy Sciences, Hatfield, PA) in PBS. Slides were rinsed twice, 3 min each, in PBS and blocked with Image-iT™ FX Signal Enhancer (Thermo Fisher Scientific, Waltham, MA) for 30 min at room temperature in a humidified chamber. Tissue sections were rinsed again thrice in PBS and incubated with single or pooled rabbit polyclonal antibodies and normal rabbit IgG for 1 h at room temperature. Slides were rinsed thrice in PBS and incubated with Alexa Fluor 568-conjugated goat anti-rabbit IgG (H + L) antibody for 1 h at room temperature. Slides were rinsed in PBS, cover-slipped with Dako Fluorescent Mounting Medium (Agilent, Santa Clara, CA), and were analyzed at excitation 579 nm and emission 603 nm using Nikon TE2000-U inverted fluorescence microscope (Nikon Corp., Kanagawa, Japan).
Mouse spleen leukocyte preparation
Mice were euthanized by carbon dioxide inhalation in accordance with University of Vermont Institutional Animal Care and Use Committee protocol (IACUC). Spleens were collected under sterilized condition, trimmed to remove fat, and cut into small pieces under the hood. The pieces were disaggregated in Dulbecco's phosphate-buffered saline (DPBS) by gently pressing them with the plunger end of a syringe between 150 μm sterilized nylon meshes. The liberated cells were passed through a 70 μm cell strainer and rinsed twice in DPBS. Red blood cells were removed by incubating the cells with ACK lysing buffer (Life Technologies Corp., Grand Island, NY) at 37 °C for 3 min. Viability was determined using trypan blue. Leukocytes from multiple mice were pooled for the study.
Arming of spleen effectors cells with antibodies
Spleen leukocyte samples were mixed with the antibody cocktail of rabbit anti-mutated peptide antibodies (1 × 108 cells + 100 μg antibodies/mL PBS) and incubated for 30 min in ice. The samples were centrifuged and the leukocyte pellet was suspended in cold PBS (1 × 108 cells/mL). The cells were kept in ice and used immediately.
Flow cytometric analysis of spleen leukocyte-binding to anti-mutated peptide antibodies
Flow cytometry was used to analyze binding of rabbit antibodies to spleen leukocytes [9]. The cells in PBS containing 1% BSA were blocked with 10% (v/v) donkey serum (Southern Biotech, Birmingham, AL) before or after incubation with rabbit polyclonal anti-mutated peptide antibodies (1 × 107 cells/1.1 μg each Ab/100μL). Cell-bound rabbit Ig was detected with phycoerythrin-conjugated donkey anti-rabbit Ig (H + L) antibody (BioLegend, San Diego, CA). All the incubation steps were for 30 min in ice followed by three-time (3 min each) washings with PBS containing 1% BSA. The stained cells were fixed in 2% paraformaldehyde and following PBS washes, the samples were run on BD LSRII (BD Biosciences, San Jose, CA) flow cytometer equipped with BD FACSDiva™ version 8 software for data acquisition. The data were analyzed using FlowJo™ v10.1 software (FlowJo, LLC, Ashland, OR) following the required gating with the help of proper controls.
Animal tumor model
A transplantable syngeneic tumor model representing a spontaneous C57BL/6-derived B16F10 melanoma tumor was used for this study. An attractive feature is the reliability and rapidity of tumor growth allowing short duration experiments. Due to the short interval from tumor inoculation to death of the mouse, a range of treatment times relatively close to the time of tumor inoculation have been reported for immunological experiments. Examples of treatment start times include the day before tumor inoculation and post inoculation days 1, 3, 5, 7, and 12 [10,11,12,13,14,15]. Consistent with these previous reports, we chose to begin treatments at day 3 post tumor inoculation. The Jackson Laboratory (Bar Harbor, ME) supplied 6–7 weeks old female mice of C57BL/6 J strain. Mice were kept in the animal facility with 12-h light/dark cycles and provided with food pellets and water ad libitum. Following one week of acclimatization, mice were ear-punched for numbering and had their right flank region shaved. B16F10 melanoma tumor cells were cultured to ~ 70% confluence in DMEM containing 10% (v/v) fetal bovine serum. Cells were tested for mycoplasma infection using detection kit (Bulldog Bio, Inc., Portsmouth, NH) to confirm negative prior to implantation. Washed cells were suspended in PBS and subcutaneously injected at the shaved right flank of the mice. All animal procedures used in the present study were approved by the UVM IACUC (Protocol # 18-002).
Experiment 1
This experiment was conducted to determine the effect of combined treatment of mouse spleen effector cells (EC) armed with a cocktail of nine rabbit polyclonal antibodies against the nine tumor-specific mutated proteins (referred below to Ab cocktail) and anti-mouse PD1 inhibitor antibody (PD1i) on tumor growth and survival. All the mice in this experiment received subcutaneous implantation of 3 × 105 B16F10 melanoma tumor cells. The mice were treated as follows:
Gr 1. PBS control: B16F10 cells implanted in PBS, no further treatment.
Gr 2. PBS+PD1i only: B16F10 cells implanted in PBS, treatment intraperitoneal 0.2 mg PD1i on 3, 6, 8, 10, and 13 days post-implantation (DPI).
Gr 3. EC+PD1i: B16F10 cells implanted in PBS, treatment subcutaneous injection of 1 × 107 spleen leukocytes (effector cells, EC) at the tumor base + intraperitoneal 0.2 mg PD1i, both on 3, 6, 8, 10, and 13 DPI.
Gr 4. EC armed with Ab cocktail+PD1i: B16F10 cells implanted in PBS, treatment subcutaneous injection of 1 × 107 spleen leukocytes armed with nine Ab cocktail at the tumor base + intraperitoneal 0.2 mg PD1i, both on 3, 6, 8, 10, and 13 DPI.
Experiment 2
This experiment was conducted to determine the effectiveness of (1) combined treatment with spleen leukocytes armed with four high tumor-binding anti-mutated antibodies and PD1i and (2) shorter time interval of injection of effector cells from every 2–3 days to every 1 day on the B16F10 melanoma tumor growth and survival. The animals received subcutaneous implantation of 3 × 105 B16F10 melanoma tumor cells. The mice were treated as follows:
Gr 1. PBS control: B16F10 cells implanted in PBS, no further treatment.
Gr 2. PBS+PD1i only: B16F10 cells implanted in PBS, treatment intraperitoneal 0.2 mg PD1i on 3, 5, 7, 10 and 12 DPI.
Gr 3. EC armed with nine-Ab cocktail+PD1i: B16F10 cells implanted in PBS, treatment subcutaneous injection of 1x107 spleen leukocytes armed with nine-Ab cocktail at the tumor base on 3, 4, 5, 6, and 7 DPI + intraperitoneal 0.2 mg PD1i on 3, 5, 7, 10, and 12 DPI.
Gr 4. EC armed with 4HB-Ab cocktail + PD1i: B16F10 cells implanted in PBS, treatment subcutaneous injection of 1 × 107 spleen leukocytes armed with the cocktail of four high-binding (HB) antibodies at the tumor base on 3, 4, 5, 6, and 7 DPI + intraperitoneal 0.2 mg PD1i on 3, 5, 7, 10, and 12 DPI.
Tumor growth and survival
Growth of B16F10 tumors was followed by measuring tumor volume (V = w2 × l/2) everyday starting from 7 DPI using an electronic caliper. Survival time was calculated based on the animal death or euthanasia following tumor volume reaching to ≥ 2000 mm3 according to the approved IACUC protocol. Body weights were recorded twice a week for monitoring general health of the mice.
Statistical analyses
Two-way ANOVA followed by Tukey’s multiple comparison test was applied for evaluating tumor growth differences. Survival data were presented as a Kaplan–Meier plot. The significance of differences among survival curves of treatment groups was analyzed using log-rank (Mantel-Cox) test. The confidence intervals (CI) for means of median survival and hazard (Mantel–Haenszel) ratios at 95% confidence level were also estimated. GraphPad (San Diego, CA) Prism software was used for some of the analyses.
Mutation analysis in cancer patients
Breast cancer and melanoma whole exome sequence data and mutation identification were downloaded from publications by Wang et al. and Snyder et al. [16, 17]. Whole exome sequencing of five neuroblastoma patients was obtained from patients treated at Helen Devos Children’s Hospital enrolled on the signature study: molecular analysis of pediatric tumors with establishment of tumor models in an exploratory biology study: NMTRC 00B. Sequencing was performed at the Translational Genomics Research Institute. DNA extraction by Qiagen AllPrep and libraries generated with KAPA Hyper (Illumina) and captured with a supplemented IDT xGen exome kit. Libraries were clustered on a flow cell and sequenced using the Novaseq 6000 (Illumina). Somatic point mutations and indels were detected by VarScan2.3.9 (VarScan2.3.9 somatic –min-coverage 20 –somatic-p value 0.001 –min-var-freq 0.05 –min-avg-qual 30) and later annotated with SnpEff software [18, 19]. Variant Effect Predictor (VEP) was used to convert the genetic variants on genes or transcripts to protein mutants on the protein level [20]. Only missense variants were considered for further analysis. The identification of the subcellular and extracellular locations for all the mutated proteins was completed with UniProt database [21]. Cell membrane protein mutants or secreted protein mutants were selected. For cell membrane protein mutants, the only mutated sites included in the analysis are those within extracellular regions of the protein.
Results
ELISA titration of antibody samples against mutated vaccine peptides revealed high titer (≥ 1:500,000) values. Calculations of EC50 value of each antibody sample provided an affinity estimate against their targets in the picomolar range (Table 1).
Fluorescence microscopic analysis of individual polyclonal antibodies to mouse B16F10 tumor sections demonstrated positive and variable binding by all the samples (Fig. 1). However, tumor binding with a cocktail of all nine antibodies produced uniformly high-intensity stained tumor sections. Antibodies generated against the mutated peptides Lama1, Ptgfrn, CD99l2, and Serpinc1 clearly displayed higher tumor tissue binding intensities in comparison to other antibodies. These antibodies were designated as four high-binding antibodies for animal studies.
Binding analysis of affinity-enriched rabbit polyclonal antibodies raised against selected mutated peptides to mouse B16F10 tumor sections by immunofluorescence microscopy. The staining by a cocktail of nine antibodies presented in the far-left panel shows strong uniform binding to the tumor tissue. Considerable variations in the staining by nine individual antibodies are seen in other panels labeled by the names of target mutated proteins. The lower right corner panel represents negative control showing no tumor binding by normal rabbit IgG and fluorescent secondary antibody
Figure 2 presents binding of the nine-antibody cocktail armed to spleen leukocytes evaluated by flow cytometry. The results show that ~ 98% of leukocytes bind to the rabbit antibodies in the cocktail (lower right). It was also observed that the donkey secondary antibody binding to mouse spleen leukocytes was negligible (lower middle). Furthermore, there was no difference in the mouse leukocyte binding to rabbit antibody, whether the samples were blocked by donkey serum samples before or after rabbit antibody incubation step (data not presented). These controls ruled out any interference with the blocker and secondary antibody.
Representative density plots and histograms from flow cytometric analyses of binding by a cocktail of nine rabbit antibodies to spleen leukocytes. Leukocyte samples were gated to include most of the live cells based on side (SSA) and forward (FSA) scatter characteristics. The histograms showing the gated fluorescently stained and unstained cell populations, representing the cells bound (Ig + ) to and not bound (Ig −) to rabbit antibodies
Animal experiment 1
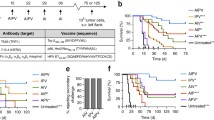
The results of combined treatment of effector cells armed with the nine-Ab cocktail and PD1i on tumor growth are presented in Fig. 3. The two-way ANOVA of the data showed significant tumor growth differences by the treatment (P = 0.0252) and time (P < 0.001) factors. The treatment with PD1i alone or PD1i in combination with unarmed effector cells did not affect the tumor growth significantly in comparison to PBS control group. However, a combined treatment of effector cells armed with the cocktail of 9 antibodies and PD1i (EC armed with Ab cocktail + PD1i) significantly retarded the tumor growth in comparison to PBS control groups. Tumor growth in this group of mice was reduced by − 39% (7 DPI), − 34% (8 DPI), − 42% (9 DPI), − 47% (10 DPI), and − 49% (13 DPI) in comparison to PBS control. Tukey’s multiple comparison test following two-way ANOVA determined significant tumor growth retardations in this group of mice treated with EC armed with Ab cocktail + PD1i in comparison to both PBS control and PD1i alone groups at 13 DPI.
The effect of different treatments on B16F10 tumor growth in mice. Significant tumor growth retardations (34–49%) were observed in the mice treated with effector cells armed with the nine-antibody cocktail and PD1i, as compared to PBS control group. Two-way ANOVA analysis of the data shows significantly different curves by treatment and time. *Significantly different (P ≤ 0.05) in comparison to PBS and PD1i alone groups as determined by Tukey’s multiple comparisons test. The values represent the mean ± SEM of six mice in each group. EC effector cells, EC armed with Ab Cocktail Effector cells armed with a cocktail of all the nine rabbit antibodies against selected mutated peptides, TCT tumor cell transplantation, T1–T5 EC treatment days, DPI days post-implantation
Kaplan–Meier plot in Fig. 4 presents mice survival data. Log-rank trend test of the data revealed a significant (P = 0.033) trend in the survival curves. Combined treatment of effector cells armed with the cocktail of antibodies against nine selected mutated proteins and PD1i significantly increased the survival of mice in comparison to the mice of control groups. The median survival was 16.5 days for PBS, 18.5 days for PD1i alone, 20 days for effector cells + PD1i, and 25 days for effector cells armed with nine-antibody cocktail groups. The survival ratio of effector cells armed with antibodies and PBS control was 1.212 with a 95% confidence of interval (CI) of the ratio ranging from 0.370 to 3.972. The hazard ratio (log-rank) of these two groups was 0.559 (95% CI 0.168–1.866).
The effect of different treatments on survival of mice implanted with B16F10 melanoma cells. The combined treatment with effector cells armed with nine-antibody cocktail and PD1i increased the survival of mice. EC effector cells, EC armed with Ab Cocktail effector cells armed with a cocktail of all the nine antibodies against selected mutated peptides, TCT tumor cell transplantation, T1–T5 EC treatment days, DPI days post-implantation
Animal experiment 2
Combined treatment of effector cells armed with four- or nine-antibody cocktail and PD1 inhibitor on tumor growth are presented in Fig. 5. Mice received daily treatment of effector cells armed with a cocktail of four high-binding antibodies or all nine antibodies for 5 days starting from 3 DPI. The results show significant retardation in the tumor growth in both the groups treated with effector cells armed with antibodies and PD1i.
The effect of combined treatment of PD1i and effector cells armed with either a cocktail of nine antibodies or four high-binding antibodies on tumor growth in mice implanted with B16F10 melanoma cells. Significant tumor growth retardations (44–68%) were observed in the mice treated with effector cells armed with nine-antibody cocktail and PD1i, as compared to PBS control group. More robust growth retardation (64–87%) was observed in the group that received combined treatment of effector cells armed with the cocktail of four high-binding antibodies and PD1i. Two-way ANOVA analysis of the data shows significantly different curves by treatment and time. *Significantly different (P ≤ 0.05) in comparison to PBS and PD1i alone groups as determined by Tukey’s multiple comparisons test. The values represent the mean ± SEM of six mice in each group. EC armed with nine-Ab Cocktail effector cells armed with a cocktail of all the nine rabbit anti-antibodies against selected mutated peptides, EC-4HB-Ab Cocktail effector cells armed with a cocktail of four high tumor-binding rabbit antibodies, TCT tumor cell transplantation; T1–T5 EC treatment days, DPI days post-implantation
The two-way ANOVA of the data showed significant tumor growth differences by the treatment (P < 0.0001) and time (P = 0.0013) factors. Treatment with PD1i alone did not produce significant effects in comparison to PBS control. However, a combined treatment of effector cells armed with nine antibodies and PD1i (EC armed with nine-Ab Cocktail + PD1i) daily for 5 days retarded the tumor growth by − 44%, − 63%, − 67%, − 68%, and − 60% at 7, 10, 11, 12, and 13 DPI, respectively, in comparison to PBS control group. Further high degrees of tumor growth retardations were observed in mice co-treated with effector cells armed with the cocktail of four high-binding antibodies (EC armed with 4HB-Ab Cocktail) and PD1i (− 64% at 7 DPI, − 84% at 10 DPI, − 87% at 11 and 12 DPI, − 85% at 13 DPI) in comparison to PBS control. Tukey’s multiple comparison test following two-way ANOVA determined highly significant tumor growth retardations in the mice of 4HB-Ab cocktail group in comparison to both PBS control (11 DPI, P = 0.0222; 12 DPI, P = 0.0025; 13 DPI, P = 0.0127) and PD1i alone (11 DPI, P = 0.0089; 12 DPI, P = 0.0006; 13 DPI, P = 0.0069) groups.
Kaplan–Meier plot in Fig. 6 presents the mice survival data following combined treatment with effector cells armed with a cocktail of four high-binding or all nine antibodies and PD1i. Log-rank (Mantel-Cox) test of the data revealed a highly significant (P < 0.0007) differences in survival curves of the four groups of animals. Survival curves of mice co-treated with effector cells armed with four- or nine-antibody cocktail plus PD1i were significantly different (P = 0.0024) from PBS control groups. Combined treatment with the cocktail of four high tumor-binding antibodies against selected mutated proteins and PD1i was most effective and produced maximum survival for 31 days. All the animals in the PBS control group died by 19 days. Median survivals were 17 days for PBS, 19.5 days for PD1i alone, 22.5 days for effector cells armed with all nine antibodies + PD1i, and 31 days for effector cells armed with four high binding antibody cocktail groups. The median survival ratio of effector cells armed with nine antibodies group and PBS control was 1.324 with 95% CI ranging from 0.404 to 4.337. The Log-rank hazard ratio of these two groups was 0.249 (95% CI 0.061–1.014).
The effect of treatment with a cocktail of four high tumor-binding antibodies on survival of mice implanted with B16F10 melanoma cells. The combined treatment with effector cells armed with four high tumor-binding antibody cocktail and PD1i increased the survival of mice longer (31 days) than those treated with the effector cells armed with a cocktail of all the nine antibodies and PD1i (22.5 days). EC effector cells, EC armed with nine-Ab cocktail effector cells armed with a cocktail of all the nine rabbit antibodies against selected mutated peptides, EC-4HB-Ab cocktail Effector cells armed with a cocktail of four high tumor-binding rabbit antibodies, TCT Tumor cell transplantation, TCT tumor cell transplantation, T1–T5 EC treatment days, DPI days post-implantation
To assess possible translation of our approach to humans, we determined the frequency of mutated targets in multiple cancers. We focused on the same selection criteria used for the B16F10 cells, which were non-synonymous mutations expressed on the extracellular surface of membrane-associated or secreted proteins (Table 2). The total number of gene mutations in the breast cancer patients ranged from 15 to 252 and in the neuroblastoma patients, ranged from 17 to 128. Using Uniprot protein database, breast cancers had an average of ten non-synonymous mutations (range 3–24) that are on the extracellular region of cell membrane proteins and on average nine non-synonymous mutations (range 1–26) expressed on secreted proteins. In the neuroblastoma tumors, there was an average of eight mutations (range 1–18) per patient on the extracellular region of cell membrane proteins and on average five mutations (range 2–9) that are expressed on secreted proteins. In malignant melanomas, we identified an average of 83 mutations (range 16–179) per tumor on the extracellular region of cell membrane proteins and on average 66 mutations (range 11–131) per tumor expressed on secreted proteins (see Supplemental Table for details).
Discussion
We previously determined that when multiple antibodies targeting nine different tumor-specific mutations were combined and delivered as a cocktail not bound to effector cells, there was remarkable inhibition of tumor (manuscript submitted). However, clinical application of this strategy is restricted by the difficulty of scaling up of antibody production from the amount needed in a mouse model to the large amount of antibody required to treat a patient. Generating multiple unique tumor-specific antibodies for each patient in sufficient quantities would be extremely challenging. In this report, we demonstrate that the amount of antibody can be dramatically reduced, when the antibodies are used to redirect immune effector cells.
Similar to our previous experiments with free antibodies, a cocktail of nine antibodies loaded on effector cells combined with PD1 inhibitor caused tumor inhibition and increased survival of mice. However, these outcomes were achieved at a dramatically lower dose of antibodies. It is remarkable that a total dose of antibodies less than 5 µg (from five injections) was capable of inhibiting tumor and prolonging survival. The dramatic reduction in antibody may make scaling up for human studies with this approach more feasible. For example, based on the types of effector cells in human peripheral blood and the molar mass of antibodies the estimated amount of antibodies needed to arm 1 × 109 effector cells is about 8–75 micrograms [22, 23]. There are a variety of strategies to obtain such small quantities of antibodies, including affinity enrichment following vaccination of a small animal as was done here. We also observed that arming effector cells with a set of higher binding antibodies increased the effectiveness of inhibiting tumor cells. These results begin to provide a selection strategy for which antibodies to use to arm effector cells.
The duration of antibodies binding to effector cells via Fc receptors is transient and likely less than 12 h [24, 25]. With a short time interval for armed cells to be bioactive, treatment for every three days might have allowed time for this highly aggressive melanoma to grow between treatments. Indeed, when armed effector cells were given daily instead of every 2–3 days, there was improved tumor control and increased survival. The short duration of antibodies binding to effector cells may be advantageous by providing a built-in safety feature, if applied to human cancer patients. Stopping treatments should rapidly cease ongoing bioactivity of the effector cells. This approach may avoid the risk for a variety of adverse events such as cytokine release syndrome [26] as occurs when CAR-T cells are given as a single large bolus.
Arming effector cells with a multiplicity of tumor-specific antibodies offers a strategy to overcome the fundamental challenge of heterogeneity. Individually, each of the nine antibodies had variable binding to B16F10 cells representing heterogeneous expression on the B16F10 cells. When combined, there was strong homogeneous binding. Targeting tumor-specific mutations may also mitigate non-tumor tissue destruction that occurs for example with CD19-targeted T cell therapy. We targeted neutral tumor-specific proteins that were not known to be driver mutations. These were random mutations that are highly tumor specific. These types of mutations appear to be common in multiple types of human cancers. Analysis of sequence data from human specimens of breast cancer, neuroblastoma, and melanoma showed that non-synonymous cell surface mutations were present and in many cases abundant. The possibility of targeting non-public patient-specific mutated proteins with antibodies has been hardly considered, because of the overwhelming challenges associated with producing large quantities of unique antibodies for each patient. Arming effector cells is accomplished with such small quantities of antibodies that treating patient-specific cancer mutations with antibodies may be possible.
In this study, unsorted splenic cells were used as effector cells. Previous studies have demonstrated that multiple types of effector cells derived from spleen, peripheral blood, marrow, and peritoneum can mediate cytotoxicity when armed with immune sera [27, 28]. Using only one immune effector cell type as is done with T cell therapy, does not take full advantage of multiple mechanisms of tumor cell destruction offered by different immune effector cells [29]. The ability to grow T cells has factored heavily in the choice of cell type for most trials. Our strategy avoids the complexity and major expense related to growing T cells ex vivo. Multiple types of effector cells are readily available from peripheral blood and do not require ex vivo growth expansion. Genetic modification to introduce a binding element as done with CAR-T cells is not necessary since effector cells are already endowed with a good handle for antibodies.
Conclusions
This study demonstrates that ex vivo arming a mixed population of immune effector cells with antibodies targeting multiple tumor-specific mutated proteins in conjunction with PD1 inhibition delayed tumor growth and prolonged survival in mice inoculated with an aggressive melanoma. A total arming dose of antibody less than 5 µg was sufficient to accomplish tumor inhibition.
The types of tumor-specific mutations targeted in this mouse study appear to be common in multiple types of human cancers. This approach requires such a small amount of antibody that clinical trials of arming effector cells with antibodies against patient-specific and tumor-specific mutations should be feasible.
References
Topalian SL, Muul LM, Solomon D, Rosenberg SA. Expansion of human tumor infiltrating lymphocytes for use in immunotherapy trials. J Immunol Methods. 1987;102:127–41.
Rosenberg SA, Packard BS, Aebersold PM, et al. Use of tumor-infiltrating lymphocytes and interleukin-2 in the immunotherapy of patients with metastatic melanoma. A preliminary report. N Engl J Med 1988;319:1676–80
Rosenberg SA, Dudley ME. Cancer regression in patients with metastatic melanoma after the transfer of autologous antitumor lymphocytes. Proc Natl Acad Sci USA. 2004;101(Suppl 2):14639–45.
Yannelli JR, Hyatt C, McConnell S, et al. Growth of tumor-infiltrating lymphocytes from human solid cancers: summary of a 5-year experience. Int J Cancer. 1996;65:413–21.
Minutolo NG, Hollander EE, Powell DJ Jr. The Emergence of universal immune receptor T cell therapy for cancer. Front Oncol. 2019;9:176.
Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725–33.
Castle JC, Kreiter S, Diekmann J, et al. Exploiting the mutanome for tumor vaccination. Cancer Res. 2012;72:1081–91.
Shukla GS, Sun YJ, Pero SC, Sholler GS, Krag DN. Immunization with tumor neoantigens displayed on T7 phage nanoparticles elicits plasma antibody and vaccine-draining lymph node B cell responses. J Immunol Methods. 2018;460:51–62.
Shukla GS, Olson WC, Pero SC, et al. Vaccine-draining lymph nodes of cancer patients for generating anti-cancer antibodies. J Transl Med. 2017;15:180.
McGray AJ, Hallett R, Bernard D, et al. Immunotherapy-induced CD8+ T cells instigate immune suppression in the tumor. Mol Ther. 2014;22:206–18.
Dominguez-Soto A, de las Casas-Engel M, Bragado R, et al. Intravenous immunoglobulin promotes antitumor responses by modulating macrophage polarization. J Immunol 2014;193:5181–9.
Hassannia H, Amiri MM, Jadidi-Niaragh F, et al. Inhibition of tumor growth by mouse ROR1 specific antibody in a syngeneic mouse tumor model. Immunol Lett. 2018;193:35–41.
Cho HI, Barrios K, Lee YR, Linowski AK, Celis E. BiVax: a peptide/poly-IC subunit vaccine that mimics an acute infection elicits vast and effective anti-tumor CD8 T-cell responses. Cancer Immunol Immunother. 2013;62:787–99.
Buhtoiarov IN, Sondel PM, Eickhoff JC, Rakhmilevich AL. Macrophages are essential for antitumour effects against weakly immunogenic murine tumours induced by class B CpG-oligodeoxynucleotides. Immunology. 2007;120:412–23.
Nagato T, Lee YR, Harabuchi Y, Celis E. Combinatorial immunotherapy of polyinosinic-polycytidylic acid and blockade of programmed death-ligand 1 induce effective CD8 T-cell responses against established tumors. Clin Cancer Res. 2014;20:1223–344.
Snyder A, Makarov V, Merghoub T, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014;371:2189–99.
Wang L, Lawrence MS, Wan Y, et al. SF3B1 and other novel cancer genes in chronic lymphocytic leukemia. N Engl J Med. 2011;365:2497–506.
Koboldt DC, Larson DE, Wilson RK. Using VarScan 2 for Germline Variant Calling and Somatic Mutation Detection. Curr Protoc Bioinform 2013;44:15 4 1–7
Cingolani P, Platts A, le Wang L, et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin). 2012;6:80–92.
McLaren W, Gil L, Hunt SE, et al. The Ensembl Variant Effect Predictor. Genome Biol. 2016;17:122.
The UC. UniProt: the universal protein knowledgebase. Nucleic Acids Res. 2017;45:D158–D69.
Fleit HB, Wright SD, Unkeless JC. Human neutrophil Fc gamma receptor distribution and structure. Proc Natl Acad Sci USA. 1982;79:3275–9.
Patel KR, Roberts JT, Barb AW. Multiple variables at the leukocyte cell surface impact Fc γ receptor-dependent mechanisms. Front Immunol. 2019;10:223.
Penfold PL, Walker LC, Roitt IM. Complex arming in antibody-dependent cell-mediated cytotoxicity: ultrastructural studies of the interaction between human effector cells armed with aggregated anti-DNP antibody and DNP-coated erythrocytes. Clin Exp Immunol. 1978;31:197–204.
Saksela E, Imir T, Makela O. Specifically cytotoxic human and mouse lymphoid cells induced with antibody or antigen-antibody complexes. J Immunol. 1975;115:1488–92.
Park JH, Riviere I, Gonen M, et al. Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N Engl J Med. 2018;378:449–59.
Parrillo JE, Fauci AS. Apparent direct cellular cytotoxicity mediated via cytophilic antibody. Multiple Fc receptor bearing effector cell populations mediating cytophilic antibody induced cytotoxicity. Immunology 1977;33:839–50.
Perlmann P, Perlmann H. Contactual lysis of antibody-coated chicken erythrocytes by purified lymphocytes. Cell Immunol. 1970;1:300–15.
Matlung HL, Babes L, Zhao XW, et al. Neutrophils kill antibody-opsonized cancer cells by trogoptosis. Cell Rep. 2018;23(3946–59):e6.
Acknowledgements
This work was supported by the SD Ireland Cancer Research Fund, Cast Off Chemo! Foundation, the Department of Surgery at the University of Vermont Larner College of Medicine internal grant, and the Beat Neuroblastoma Foundation. This work was also supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under Grant Number P20GM103449. Flow cytometry data was obtained at the Harry Hood Bassett Flow Cytometry and Cell Sorting Facility at the University of Vermont Larner College of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and ethical standards
All animal procedures used in the present study were approved by the UVM IACUC (Protocol # 18-002).
Animal source
Mice were obtained from the Jackson Laboratory (Bar Harbor, ME) in the present study.
Cell line authentication
We utilized confirmed sequence data of B16F10 mouse melanoma tumor cell line7 and selected multiple cell surface-related mutated proteins with a single amino acid substitution.
Informed consent
Informed consent is not applicable to this manuscript. We only report on mice and did refer to having the protocol correctly approved. The human sequence information comes from public databases.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shukla, G.S., Pero, S.C., Sun, Y.J. et al. Multiple antibodies targeting tumor-specific mutations redirect immune cells to inhibit tumor growth and increase survival in experimental animal models. Clin Transl Oncol 22, 1094–1104 (2020). https://doi.org/10.1007/s12094-019-02235-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02235-3