Abstract
Introduction
In patients with peritoneal carcinomatosis (PC), the incidence of respiratory complications following cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) is not well established. We aimed to describe the center-specific incidence and patient characteristics associated with respiratory complications following CRS and HIPEC in patients receiving treatment for PC.
Materials and methods
We used the University Hospital of Arrixaca study database to identify patients who underwent CRS and HIPEC for PC. Patients who experienced a post-operative respiratory complication were categorized according to the National Cancer Institute-Common Terminology Criteria for Adverse Events. Multivariable regression methods were used to identify independent risk factors for developing a respiratory complication following CRS and HIPEC.
Results
Between 2008 and 2017, we identified 247 patients who underwent CRS and HIPEC for PC. A total of eight patients (3.2%) were categorized as having a post-operative respiratory complication. A diaphragmatic peritonectomy and a PC index of > 14 were identified as independent risk factors for developing a respiratory complication. Radiographic evidence of a pleural effusion was identified in 72 patients who had CRS of the diaphragmatic peritoneum; however, only 6 (8.3%) of these patients required pleural drainage.
Conclusions
Only 3.2% of patients developed a symptomatic respiratory complication following CRS and HIPEC. A pleural effusion was identified in almost all patients requiring a diaphragmatic peritonectomy as part of their CRS; however, less than one in ten of these patients required pleural drainage. Prophylactic insertion of a pleural drainage tube is, therefore, not indicated following CRS and HIPEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peritoneal carcinomatosis (PC) is an advanced form of cancer found in the peritoneal cavity [1]. It is most often caused by malignant spread from a primary tumor in the appendix, bowel, rectum or ovaries and has been associated with median survival rates of 6 months or less [1]. However, over the last 2 decades, cytoreductive surgery (CRS) followed by hyperthermic intraperitoneal chemotherapy (HIPEC) has been developed as a curative treatment for patients with PC [2].
The aim of CRS is to remove the maximum amount of macroscopic tumor cells through both the surgical excision of the peritoneum (peritonectomy), and the resection of involved but non-essential abdominal organs [3, 4]. Following CRS, but still at the time of surgery, the abdominal cavity is flushed with a heated chemotherapeutic agent [2]. This method permits the local absorption of a highly concentrated cytotoxic agent into superficial cell layers, helping to maximize its therapeutic effect and minimize its systemic side effects—a procedure known as HIPEC [2, 4].
Combined, CRS and HIPEC have proven to provide a survival benefit in patients who have developed PC following a primary colorectal or ovarian cancer [4]. In general, the 30-day mortality is reported between zero and five percent and the procedure is well-tolerated in carefully selected patients [5]. Major post-operative complications following CRS and HIPEC are reported to occur in 15–40% of patients [5].
The most commonly identified post-operative complication is paralytic ileus [6]. Rarer complications are less well described. For example, the incidence, predisposing factors and management of respiratory complications following CRS and HIPEC are poorly described. In particular, there is widespread debate as to how often patients experience symptomatic post-operative pleural effusion and how often they need subsequent pleural drainage [7].
In this study, we aim to address this gap in the literature by partitioning our analysis into two sections. In the first part of the analysis, we use the University Hospital of Arrixaca study database from 2008 to 2017 to identify the incidence of respiratory complications in patients with PC who have undergone CRS and HIPEC. We then categorize the respiratory complications according to version 4.0 of the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) [8] and, in a separate step, identify all patients who experience a post-operative pleural effusion. In the second part of the analysis, we build univariate and multivariable logistic regression models and identify the patient factors associated with developing respiratory complications following CRS and HIPEC.
Materials and methods
Study population
A retrospective analysis was performed of all patients who underwent CRS and HIPEC at the University Hospital of Arrixaca between 1st January 2007 and 1st January 2017.
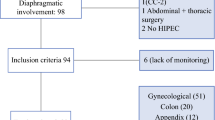
Included in this study were patients between ages 18 and 80, who underwent surgery for PC. All patients had to have a histologically confirmed PC secondary to the following primary malignancies: ovarian carcinoma or platinum-sensitive recurrences (recurrence of active oncological disease in patients who have achieved a documented response to initial platinum-based treatment), colorectal cancer and gastric cancer. Patients with PC secondary to other less frequent primary malignancies were also considered and these included non-ovarian gynecological tumors, peritoneal sarcomatosis, peritoneal pseudomyxoma or malignant peritoneal mesothelioma. To be considered for the procedure, patients also had to have an adequate baseline functional status [Eastern Cooperative Oncology score (ECOG) 0–1] [9] and an absence of serious comorbidities, including cardiopathy or severe valvulopathy, coagulopathy and renal or hepatic dysfunction.
Patients were excluded from the study in the presence of (a) extraperitoneal disease at the time of evaluation, (b) a platelet count that could not be improved (with figures < 80,000 platelets/m3), (c) the presence of heart, kidney or respiratory failure, and (d) an International Normalized Ratio (INR) of 1.5 of above.
University Hospital of Arrixaca CRS and HIPEC study database
Data from paper and electronic medical records for all patients included in our study were retrospectively entered into a study-specific database. Variables included information on demographic, clinical and operative characteristics. Specific operative variables in the database included information on the requirement of diaphragmatic peritonectomy, supramesocolic surgery or splenectomy, the total operative time and the peritoneal carcinomatosis index (PCI, a score that is used to assess the extent of peritoneal cancer in the peritoneal cavity) [10, 11].
Data referring to post-operative morbidity and mortality were collected prospectively. The end-point of follow-up was 1st January 2017. We categorized patients as having a post-operative respiratory complication; if according to version 4.0 of NCI-CTCAE, they qualified as having a grade II-V adverse event [8].
Grading of respiratory complications using the NCI-CTCAE
The NCI-CTCAE are a set of criteria developed by the US National Cancer Institute that standardize the classification of adverse effects following the administration of drugs used in cancer therapy [8]. The NCI-CTCAE use a five-point scale (grade I–V) to grade the severity of post-procedural adverse events [8]. As an assessment tool, it can be adapted to specific conditions and symptoms and has been widely validated in the available literature [4, 7, 12].
In our study, and in accordance with the NCI-CTCAE, respiratory complications in which the required treatment was clinical observation only (grade I) were considered minor and not included in the final analysis. Symptomatic respiratory complications requiring only minimal medical intervention (grade II) were graded as moderate. Complications requiring ultrasound or computed tomography-guided percutaneous drainage, either through the placement of a pleural drainage tube or therapeutic endoscopy, were considered severe (grade III). Life-threatening respiratory complications requiring repeat surgical intervention or the admission to the intensive care unit (ICU) were graded IV. Deaths related to respiratory complications were graded V [8] (see Online Appendix Table S1).
Pleural effusion
Post-operative pleural effusion in patients undergoing CRS and HIPEC was diagnosed using chest radiographs. According to the NCI-CTCAE, a pleural effusion was only categorized as a respiratory complication if medical intervention (grade II) or the placement of a pleural drainage tube (grade III) was considered clinically indicated (voluminous pleural effusion and accompanying respiratory symptoms) or if the patient required intubation and intensive care monitoring (grade IV) or died as a direct result of the pleural effusion (grade V) [8].
Statistical analysis
In the first part of the analysis, demographic, clinical and operative characteristics were described for all patients, and stratified according to the presence of respiratory complication (NCI-CTCAE grades II–V). In a separate step, all patients with radiographic evidence of a pleural effusion were identified and categorized according to the NCI-CTCAE. Continuous data were presented as means with standard deviations (SD) and compared using the Student’s t test. Categorical variables were described as frequencies and percentages and compared using the Chi-square test.
In the second part of the analysis, a univariate model was built to compare the patient’s characteristics between those who categorized as having a grade II–V post-operative respiratory complication and those who were not. In this model, the magnitude of the association between the categorical variables and the development of a respiratory complication was established by calculating the relative risk, and between continuous variables using the Pearson correlation coefficient. To determine the independent patient characteristics associated with post-operative respiratory complications, a multivariable logistic regression was used to estimate odds ratios (OR) adjusted for the potential correlation between all risk factors found to be statistically significant in the univariate analysis.
All analyses were conducted with the statistical program SPSS v. 22.0 (Chicago, Illinois, USA).
Results
Description of the study cohort
From January 1st, 2008, to January 1st, 2017, 282 patients with PC who underwent CRS and HIPEC procedures at the University Hospital of Arrixaca were identified. Of these, 35 patients had, at the time of laparotomy, unresectable disease and were excluded from the study (Fig. 1). A total of 247 patients were included in our final analysis.
The median age of the study cohort was 58 years (range 27–79 years). Primary surgery was performed on 47 patients (19.0%), surgery after preoperative chemotherapy (interval surgery) on 100 patients (40.5%), rescue surgery after initial suboptimal surgery on 32 patients (13.0%) and surgery due to recurrence after a disease-free period on the remaining 68 patients (27.5%). The median PCI was 10 (range 1–32). In 216 patients (87.4%), surgery was considered CC-0 (no macroscopic tumor residue at the end of surgery) and in the remaining 31 (12.6%) patients, CC-1 (tumor residue less than 2.5 mm). Of the 247 patients, 110 patients (44.5%) required surgery on the supramesocolic compartment. A diaphragmatic peritonectomy was performed on a total of 73 patients (29.6%).
On anesthetic assessment, 176 patients (71.3%) were graded as either ASA (American Society of Anesthesiologists physical grading system) I or II, and the remaining 71 patients (28.7%) classified as ASA III.
Respiratory complications
According to the NCI-CTCAE, a total of eight patients (3.2%) qualified as having a respiratory complication following CRS and HIPEC (Table 1). Of these, one patient had a grade II complication, six patients had grade III complications and one patient had a grade IV complication. No patient was found to have a grade V post-operative respiratory complication. All eight patients were female.
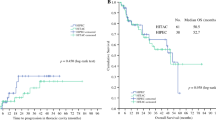
In the univariate analysis (Table 2), the factors associated with grade II–IV respiratory complications were diaphragmatic peritonectomy (p = 0.001), the need for intraoperative platelet transfusion (p < 0.001), PCI ≥ 14 (p = 0.03), surgery in the supramesocolic compartment (p = 0.01), surgery lasting over 300 min (p = 0.02) and omentectomy (p = 0.04). In the multivariate analysis, we found that diaphragmatic peritonectomy (O.R. 1.9; 95% CI 1.00–3.64, p = 0.049) and the PCI ≥ 14 (OR 3.4%; 95% CI 1.7–6.7; p < 0.001) were the only independent patient characteristics identified to be associated with developing a post-operative respiratory complication.
Pleural effusion
Radiographic evidence of a pleural effusion was found on 72 of the 73 patients on whom a diaphragmatic peritonectomy was performed as part of their CRS. Of these 72 patients, six (8.3%) had a voluminous symptomatic pleural effusion that required pleural drainage (Table 1). Five of these patients were categorized as having a grade III complication. The other patient who underwent pleural drainage developed respiratory distress in the immediate post-operative period that prevented extubation (and intensive care monitoring) until the 8th post-operative day and was categorized as having a grade IV complication.
Discussion
Main findings
According to the NCI-CTCAE criteria, the incidence in our institution of a grade II–V respiratory complication following CRS and HIPEC is 3.2% (8 patients). Following multivariable logistic regression, the only independent risk factors associated with the development of respiratory complications were a PCI ≥ 14 and the requirement of a diaphragmatic peritonectomy. Almost all patients who required a peritonectomy of the diaphragm developed radiographic evidence of a pleural effusion; however, only 8.3% (six patients) of these patients met the NCI-CTCAE criteria for having a graded respiratory complication. In each of these cases, pleural drainage was required to alleviate symptoms.
Methodological limitations
In identifying the incidence of respiratory complications, we have updated the existing literature on the post-operative morbidity following CRS and HIPEC for PC. Based on our large case series, we are confident that our results, according to the NCI-CTCAE, reflect the true incidence of post-operative respiratory complications; however, we must acknowledge that they remain specific to the population of PC patients which our surgical unit serves. To improve the generalizability of our findings we would need nationwide morbidity data on all patients undergoing CRS and HIPEC and unfortunately, no national database containing this information currently exists. Instead, our incidence figures can still be used to inform clinicians and counsel PC patients prior to CRS and HIPEC but when doing so the limitations of applying the results to different patient populations must be acknowledged.
We must also recognize the limitations in our statistical modeling. With only eight patients found to have a respiratory complication, there is limited statistical power to detect differences in potential risk factors between those who developed a respiratory complication and those who did not. It is, therefore, probable that other independent risk factors for developing a respiratory complication following CRS and HIPEC exist.
Explanation of results
Respiratory complications
Respiratory complications following major surgery are a recognized phenomenon and encapsulate a myriad of pathologies that are often related [13]. These include atelectasis, pneumonia, pulmonary embolism (PE) and symptomatic pleural effusion [14]. In broad terms, general anesthesia and major abdominal surgery have long been attributed as the main causes of post-operative respiratory complications [12,13,14,15,16]. More specifically, reduced lung capacity induced by prolonged anesthesia leads to atelectasis from which more severe pneumonic pathology can develop [17].
In our analysis, the two main risk factors associated with the development of a post-operative respiratory complications were the requirement of a diaphragmatic peritonectomy and a PCI ≥ 14. The peritoneum of the diaphragm is found adjacent to the pleura of the lungs; therefore, its anatomic location best explains why following extensive dissection—including the partial or complete removal of the diaphragmatic peritoneum (or in some cases an entire portion of the diaphragm)—a diaphragmatic peritonectomy is a risk factor for developing a post-operative respiratory complication [17, 18]. Similarly, a higher PCI equates to more extensive disease and thus the potential for more extensive surgical dissection, including dissection of the diaphragm.
All eight patients found to have a respiratory complication in our study were female. Five out of eight of these patients’ primary source of malignancy was ovarian and it is already known that PC most often metastasizes from ovarian cancer thus helping to explain female sex as a proxy risk factor [1]. The predisposition of all the other primary malignancies identified in our patients—cancers of the colon and appendix and mesothelioma—varies between male and female [5]; however, with only three patients in total it is likely the role of chance best explains why these remaining patients were all female.
Pleural effusion
The development of a post-operative pleural effusion is particularly common following diaphragmatic peritonectomy [18] and in almost all patients undergoing this surgical maneuver effusion an was noted on post-operative chest radiograph. However, according to the NCI-CTCAE, less than 10% of patients with pleural effusion qualified as having a respiratory complication.
The mobilization of the liver, required during diaphragmatic peritonectomy, can contribute to the development of pleural effusion whilst iatrogenic microscopic defects of the diaphragm, often not identified during surgery, can increase the passage of fluid to the thoracic cavity during the HIPEC treatment and lead to fluid collecting in the pleural cavity. Post-operative pleural effusion will almost be inevitable in a majority of patients requiring diaphragmatic peritonectomy as part of their CRS and especially so for patients with advanced ovarian cancer where the diaphragm is frequently affected by metastatic spread [7, 19].
How you treat the pleural effusion is, therefore, an important component in the post-operative management of patients undergoing diaphragmatic peritonectomy. Some clinicians advocate the prophylactic use of pleural drainage following cytoreduction of the diaphragm and argue that since the presence of pleural effusion is universal, the insertion of a chest tube leads to an improvement in post-operative respiratory parameters in all patients undergoing diaphragmatic peritonectomy [6, 7].
However, pleural tubes are not without their complications including infection, pain, intrapleural bleeding and hemothoraces, and on occasion damage to other viscera. Although our series did identify the almost universal occurrence of pleural effusion following diaphragmatic CRS, only eight patients were categorized as having a symptomatic respiratory complication and only six of these patients required pleural drainage. Based on our own results, we, therefore, do not advocate the routine use of pleural tubes in patients undergoing diaphragmatic peritonectomy as part of their CRS.
We did find the learning curve proved to be a strong ally in our management of post-CRS and HIPEC-induced pleural effusions. From 166 patients operated on between 2008 and 2012, 5 patients (3.0%) required pleural drainage following diaphragmatic peritonectomy as opposed to 1 patient from 81 cases (1.2%) between 2013 and 2017. In this second half of our surgical series, we adapted our surgical protocol by applying cold physiological saline during the diaphragmatic peritonectomy.
Conclusion
According to the NCI-CTCAE, less than 5% of all patients with PC who undergo CRS and HIPEC go onto develop symptomatic respiratory complications in the post-operative period. In our study, patients requiring diaphragmatic peritonectomy as part of their CRS almost universally develop post-operative pleural effusion; however, less than 10% of these require pleural drainage to alleviate their respiratory symptoms. We, therefore, do not advocate the routine and prophylactic use of pleural tubes in any patients undergoing CRS and HIPEC for PC.
Abbreviations
- ASA:
-
American Society Anaesthesiologists
- CRS:
-
Cytoreductive surgery
- ECOG:
-
Eastern Cooperative Oncology score
- HIPEC:
-
Hyperthermic intraperitoneal chemotherapy
- INR:
-
International normalized ratio
- ITU:
-
Intensive care unit
- NCI-CTCAE:
-
National Cancer Institute-Common Terminology Criteria for Adverse Events
- OR:
-
Odds ratio
- PC:
-
Peritoneal carcinomatosis
- PCI:
-
Peritoneal carcinomatosis index
- SD:
-
Standard deviation
References
Hoskins WJ. Epithelial ovarian carcinoma: principles of primary surgery. Gynecol Oncol. 1994;55:S91–6. https://doi.org/10.1006/gyno.1994.1346.
Muñoz-Casares FC, Rufián S, Rubio MJ, Díaz CJ, Díaz R, Casado A, et al. The role of hyperthermic intraoperative intraperitoneal chemotherapy (HIPEC) in the treatment of peritoneal carcinomatosis in recurrent ovarian cancer. Clin Transl Oncol. 2009;11:753–9.
Shih KK, Chi DS. Maximal cytoreductive effort in epithelial ovarian cancer surgery. J Gynecol Oncol. 2010;21:75–80. https://doi.org/10.3802/jgo.2010.21.2.75.
Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol. 2006;103:559–64. https://doi.org/10.1016/j.ygyno.2006.03.051.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. https://doi.org/10.3322/caac.21166.
Benedetti Panici P, Di Donato V, Fischetti M, Casorelli A, Perniola G, Musella A, et al. Predictors of postoperative morbidity after cytoreduction for advanced ovarian cancer: analysis and management of complications in upper abdominal surgery. Gynecol Oncol. 2015;137:406–11. https://doi.org/10.1016/j.ygyno.2015.03.043.
Eisenhauer EL, D’Angelica MI, Abu-Rustum NR, Sonoda Y, Jarnagin WR, Barakat RR, et al. Incidence and management of pleural effusions after diaphragm peritonectomy or resection for advanced mullerian cancer. Gynecol Oncol. 2006;103:871–7. https://doi.org/10.1016/j.ygyno.2006.05.023.
U.S. Department of Health and Human Services. National Institutes of Health. National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. Published: May 28, 2009 (v4.03: June 14, 2010). n.d.
Péus D, Newcomb N, Hofer S. Appraisal of the Karnofsky performance status and proposal of a simple algorithmic system for its evaluation. BMC Med Inform Decis Mak. 2013;13:72. https://doi.org/10.1186/1472-6947-13-72.
Gilly FN, Cotte E, Brigand C, Monneuse O, Beaujard AC, Freyer G, et al. Quantitative prognostic indices in peritoneal carcinomatosis. Eur J Surg Oncol. 2006;32:597–601. https://doi.org/10.1016/j.ejso.2006.03.002.
Sugarbaker PH. Management of peritoneal-surface malignancy: the surgeon’s role. Langenbeck’s Arch Surg. 1999;384:576–87.
Cliby W, Dowdy S, Feitoza SS, Gostout BS, Podratz KC. Diaphragm resection for ovarian cancer: technique and short-term complications. Gynecol Oncol. 2004;94:655–60. https://doi.org/10.1016/j.ygyno.2004.04.032.
Dowdy SC, Loewen RT, Aletti G, Feitoza SS, Cliby W. Assessment of outcomes and morbidity following diaphragmatic peritonectomy for women with ovarian carcinoma. Gynecol Oncol. 2008;109:303–7. https://doi.org/10.1016/j.ygyno.2008.02.012.
Chéreau E, Rouzier R, Gouy S, Ferron G, Narducci F, Bergzoll C, et al. Morbidity of diaphragmatic surgery for advanced ovarian cancer: retrospective study of 148 cases. Eur J Surg Oncol. 2011;37:175–80. https://doi.org/10.1016/j.ejso.2010.10.004.
Montz FJ, Schlaerth JB, Berek JS. Resection of diaphragmatic peritoneum and muscle: role in cytoreductive surgery for ovarian cancer. Gynecol Oncol. 1989;35:338–40. https://doi.org/10.1016/0090-8258(89)90074-7.
Chéreau E, Ballester M, Selle F, Cortez A, Pomel C, Darai E, et al. Pulmonary morbidity of diaphragmatic surgery for stage III/IV ovarian cancer. BJOG An Int J Obstet Gynaecol. 2009;116:1062–8. https://doi.org/10.1111/j.1471-0528.2009.02214.x.
Aletti GD, Dowdy SC, Gostout BS, Jones MB, Stanhope CR, Wilson TO, et al. Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol. 2006;107:77–85. https://doi.org/10.1097/01.AOG.0000192407.04428.bb.
Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol. 2002;20:1248–59. https://doi.org/10.1200/JCO.2002.20.5.1248.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of the research article entitled “Identifying the incidence of respiratory complications following diaphragmatic cytoreduction and hyperthermic intraoperative intraperitoneal chemotherapy” declare that there are no potential conflicts of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cascales Campos, P., Martinez Insfran, L.A., Wallace, D. et al. Identifying the incidence of respiratory complications following diaphragmatic cytoreduction and hyperthermic intraoperative intraperitoneal chemotherapy. Clin Transl Oncol 22, 852–859 (2020). https://doi.org/10.1007/s12094-019-02195-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02195-8