Abstract
Purpose/objectives
To evaluate the prognostic impact of maximum standardized uptake value (SUVmax) in patients with locally advanced head and neck squamous cell carcinoma (HNSCC) undergoing pretreatment [F-18] fluoro-d-glucose-positron emission tomography/computed tomography (FDG PET/CT) imaging.
Materials/methods
Fifty-eight patients undergoing FDG PET/CT before radical treatment with definitive radiotherapy (±concomitant chemotherapy) or surgery + postoperative (chemo)radiation were analyzed. The effects of clinicopathological factors (age, gender, tumor location, stage, Karnofsky Performance Status (KPS), and treatment strategy) including primary tumor SUVmax and nodal SUVmax on overall survival (OS), disease-free survival (DFS), locoregional control (LRC), and distant metastasis-free survival (DMFS) were evaluated. Kaplan–Meier survival curves were generated and compared with the log-rank test.
Results
Median follow-up for the whole population was 31 months (range 2.3–53.5). Two-year OS, LRC, DFS and DMFS, for the entire cohort were 62.1, 78.3, 55.2 and 67.2%, respectively. Median pretreatment SUVmax for the primary tumor and lymph nodes was 11.85 and 5.4, respectively. According to univariate analysis, patients with KPS < 80% (p < 0.001), AJCC stage IVa or IVb vs III (p = 0.037) and patients undergoing radiotherapy vs surgery (p = 0.042) were significantly associated with worse OS. Patients with KPS < 80% (p = 0.003) or age ≥65 years (p = 0.007) had worse LRC. The KPS < 80% was the only factor associated with decreased DFS (p = 0.001). SUVmax of the primary tumor or the lymph nodes were not associated with OS, DFS or LRC. The KPS < 80% (p = 0.002), tumor location (p = 0.047) and AJCC stage (p = 0.025) were associated with worse cancer-specific survival (CSS). According to Cox regression analysis, on multivariate analysis KPS < 80% was the only independent parameter determining worse OS, DFS, CSS. Regarding LRC only patients with IK < 80% (p = 0.01) and ≥65 years (p = 0.01) remained statistically significant. Nodal SUVmax was the only factor associated with decreased DMFS. Patients with a nodal SUVmax > 5.4 presented an increased risk for distant metastases (HR, 3.3; 95% CI 1.17–9.25; p = 0.023).
Conclusions
The pretreatment nodal SUVmax in patients with locally advanced HNSCC is prognostic for DMFS. However, according to our results primary tumor SUVmax and nodal SUVmax were not significantly related to OS, DFS or LRC. Patients presenting KPS < 80% had worse OS, DFS, CSS and LRC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Outcome indicators in patients with head and neck squamous cell carcinoma (HNSCC) cancer have traditionally been derived from clinical and pathological features [1].
Recognition of additional prognostic factors for locoregional control (LRC) and overall survival (OS), particularly biologic parameters, may allow the development of individualized strategies that lead to improved outcomes in terms of LRC and survival.
Tumor [F-18] fluoro-d-glucose (FDG) uptake has been associated with various cellular characteristics such as cell viability and proliferation activity [2, 3]. Hence, analyses of metabolic parameters, which are independent of morphologic changes, offer an attractive opportunity to predict individual tumor behavior. This would have implications not only for the clinical management of head and neck cancer patients but also for their prognostic stratification.
Clinical outcomes have particularly improved with the incorporation of concurrent, platinum-based chemotherapy and epidermal growth factor receptor targeted therapy [4,5,6]. Nevertheless, long-term OS in patients with locally advanced disease remains suboptimal [7].
Identification of pretreatment prognostic factors to supplement conventional TNM staging could help to detect high-risk subpopulations of patients who might benefit from treatment intensification.
Recently, the relationship between tumor FDG uptake and the outcomes of different treatment strategies in patients with locally advanced-stage HNSCC has received growing attention [8,9,10]. The prognostic value of maximum standard uptake value (SUVmax) is an unresolved issue with PET scanning. In theory, a greater SUVmax would correspond with a more aggressive tumor. However, controversy has SUVmax with multiple series [11] reporting both for and against a correlation with outcomes in HNSCC.
Thus, the aim of this study was to evaluate the prognostic value of a well-known metabolic parameter such as SUVmax (commonly available in clinical practice) in patients with locally advanced HNSCC undergoing pretreatment FDG-positron emission tomography (FDG PET/CT) imaging.
Materials and methods
Patient population
Patients enrolled in a prospective PET scanning study valuating the diagnostic performance of pretreatment PET/CT form the basis of this analysis.
The current study is a subgroup analysis of a population from a previous prospective study performed at our institution [12]. We recruited 84 patients in our department between September 2011 and February 2013 to determine the incremental staging information provided by pretreatment PET/CT and its impact on management plans in patients with untreated stage III–IV HNSCC. All patients were staged according to 7th edition American Joint Committee on Cancer criteria [13]. Patient characteristics as well as the results of diagnostic studies were recorded prospectively in a dedicated database.
Pretreatment systematic evaluations were performed along with a routine physical examination, laryngoscopy and tissue biopsy, serum chemistry, contrast-enhanced CT or MRI of the head and neck, and FDG PET/CT scan. Clinical staging and treatment choices were decided using the information derived from these examinations at the Head and Neck Cancer Board.
For the present study, we selected a group of patients from the original cohort as follows: Patients with locally advanced HNSCC who underwent PET/CT before a radical treatment either with definitive radiotherapy (±concomitant chemotherapy) or surgery + postoperative (chemo) radiation. Patients undergoing treatment with palliative intent or presenting with distant metastasis at diagnosis were not included. A total of 58 patients met the inclusion criteria and were assessed in this study. This study was approved by the local Ethics Committee (reference number: CEIC 11/46).
FDG PET technique and imaging assessment
FDG PET/CT (CT without contrast) was obtained in all patients prior to receiving treatment. After the patients had fasted for at least 6 h, and 60 min before the scan, they were given an intravenous injection of fluorodeoxyglucose (FDG) using a dosage of 3–4 MBq/kg (210–440 MBq). Images were acquired from the head to the mid-thighs. Axial images were acquired using a GE Discovery PET/CT 600 with BGO crystal and a 16-channel CT scan (with a tube voltage of 120 kV and current of 10 mA), and images were reconstructed in coronal and sagittal planes [12].
The maximum standardized uptake value (SUVmax) was quantitatively used to determine FDG PET/CT activity. Region-of-interest borders were set by manual adjustment in three planes to exclude adjacent physiologic FDG-avid structures. SUV is commonly defined as the concentration of FDG divided by the injected dose, corrected for the body weight of the patient and radioactive decay at scanning time (SUV = activity concentration/[injected dose/body weight]). We calculated the SUV value according to the Janmahasatian formulation. However, no SUV cut-off was established to read a region as positive. The PET/CT interpretation was qualitative, in which visual analysis of 18F-FDG uptake above background was used [12].
To calculate the SUV, pretreatment scans images were reviewed and the slice containing the macroscopic disease (primary tumor or nodes) was selected. In general, three bed positions were acquired. To minimize partial volume effects, the maximum SUV within the regions of interest (ROIs) was used for further calculations. Therefore, SUV values (a semiquantitative measurement of relative FDG uptake within ROIs) were calculated.
The measured variables were primary tumor and nodal volume (calculated directly from the number of pixels in the PET scan drawn regions), SUVmax, on pretreatment scans.
Treatment characteristics
Treatment decision was adopted in a multidisciplinary tumor board considering the best radical approach for each case according to current guidelines [14].
Twenty-one patients (36.2%) underwent radical surgery with neck dissection followed by postoperative radiotherapy to a total dose of 60 Gy or 66 Gy (a higher dose of radiation up to 66 Gy was administered in case of positive margins and/or when extracapsular extension was appreciated after surgery [15, 16]). In the surgery group, several surgical approaches (local excision or organ excision) were used according to the primary tumor location and extension. Regarding the neck management, a total of 21 patients underwent a neck dissection as follows: unilateral neck dissection was performed in three cases (5.2%) whereas bilateral neck dissection was performed in 18 patients (31%).
Thirty-seven (63.8%) patients received definitive radiotherapy: Forty-nine patients were treated with three-dimensional radiation therapy (3D-CRT) and nine patients received Intensity Modulated Radiation Therapy (IMRT). Briefly, when 3D-CRT was administered patients received a prescribed dose of 70 Gy to the planning target volume (PTV70) and 50 Gy to the lower risk volume (subclinical disease) at 2 Gy per fraction. Patients undergoing IMRT received a prescribed dose of 70 Gy to the planning target volume (PTV70), 59.4 Gy to the high-risk subclinical disease (PTV59.4), and 54 Gy to the lower risk subclinical disease (PTV54). The dose per fraction was 2.12 Gy to PTV70, 1.8 Gy to PTV59.4, and 1.64 Gy to PTV54 [17, 18].
Forty-five (77.6%) patients underwent concomitant chemotherapy (either with definitive or postoperative radiation) receiving high-dose cisplatin alone, consisting of 100 mg/m2 every 3 weeks for a planned three cycles. Chemotherapy was administered with concomitant radiotherapy either in patients treated with definitive radiotherapy or in patients undergoing previous surgery (in these cases concomitant postoperative chemoradiation was considered for resected poor-risk disease: when nodal extracapsular extension or surgical positive margins were found after surgery) [19,20,21].
Clinical endpoints and follow-up
Data were collected from prospective follow-up of patients after treatment to determine locoregional failure, distant failure, or death. All patients were seen in post-treatment follow-up visits jointly by radiation oncology, medical oncology, and head and neck surgeons (planned for 4, 8, and 12 weeks after completion of treatment, then every 3–4 months for 2 years, followed by every 6 months thereafter). The patients were evaluated with direct flexible fiber-optic endoscopic examinations along with post-treatment imaging studies (CT, PET–CT, and MRI).
Cancer-specific survival (CSS) refers to the actuarial rate of freedom from death with HN cancer. However, overall survival (OS) was defined as death due to any cause (all causes of death were considered). Locoregional failure was defined as recurrence in the head and neck region (local failure at the primary site or any nodal failure after treatment was considered as an event). Time to locoregional failure was calculated from the initial date of treatment to the date of an event or the last follow-up visit. Locoregional failures were included as first failure event or as event occurring concurrently with distant failure. A diagnosis of recurrent tumor or distant metastasis was based on either a positive biopsy or unequivocal clinical or radiographic evidence of progression.
Disease-free survival (DFS) was defined as those patients rendered disease free and alive at last follow-up. Events included in the analysis of DFS included any locoregional or distant failure, or death from any cause. Finally, distant metastasis-free survival (DMFS) was defined as the absence of any distant metastasis at the last follow-up.
Statistical analysis
Continuous variables are expressed as the median and range, or the mean ± standard deviation, whereas categorical variables are presented as frequencies and percentages. We sought to determine the prognostic significance of primary tumor and lymph node SUVmax along with other clinical parameters (age, gender, tumor location, tumor stage, Karnofsky Performance Status (KPS), and treatment strategy (radiotherapy group/surgery group), relative to OS, LRC, DFS and DMFS.
We analyzed the statistically significant SUV cut-off value for LRC and survival analysis using the log-rank test and receiver operating characteristic (ROC) curve analysis with the optimal threshold determined by Youden’s criterion. However, we did not found any significant cut-off point better than the median value. Therefore, the median value of the SUV (primary tumor SUVmax and nodal SUVmax) of the whole population was used to establish two subgroups above and below the median SUVmax value, although this value does not necessarily represent the best discriminative cut-off. This approach is in agreement with methodology previously reported by other authors [8, 9, 22, 23].
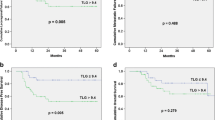
OS, LRC, DFS, and DMFS were calculated using the Kaplan–Meier method. Kaplan–Meier curves were generated for statistically significant clinical parameters, including SUVmax (dichotomizing the patient population above and below the median value of the pertinent SUV parameter) and comparisons were made with the log-rank test.
The Cox regression analysis was performed to identify significant prognostic factors for LRC and survival. Variables with a p < 0.100 in the univariate analysis were included in the multivariate stepwise non-automatic model. p values of <0.05 were considered statistically significant. Data were analyzed using Statistical Package for the Social Sciences (SPSS, version 23.0).
Results
Patient and treatment characteristics
A total of 58 patients were assessed in this study. The median age at diagnosis was 61.5 years, (range 39.4–84.8) and 52 patients (89.7%) were male. All patients presented with locally advanced disease (stage III/IVa-b). T3 and T4 disease comprised 67.2% of the study population, whereas 77.5% of patients had N2 or N3 disease. The most common subsites were larynx and hypopharynx, comprising 62% of the study population. The majority of patients (63.8%) received definitive radiation (with or without concurrent chemotherapy). Table 1 summarizes the study population.
Median follow-up for surviving patients was 42.7 months (range 23–53 months) and 31 months (range 2.3–53.5) months for the whole population. Two-year OS, LRC, DFS and DMFS, for the entire cohort were 62.1, 78.3, 55.2 and 67.2%, respectively (see Fig. 1). Median pretreatment SUVmax for the primary tumor and lymph nodes was 11.85 (range 3.1–25.8) and 5.4 (range 1.8–18), respectively.
Correlation between SUV and clinical parameters
We evaluated the relationship between clinical prognostic factors (T stage, N stage, treatment group) to assess the potential linkage. Hence, T1 and T2 tumors (T1 + T2) had a lower median SUVmax compared with T3-T4 tumors (8.5 vs 12, respectively; p = 0.027). Regarding nodal staging, N1 tumors had a lower median SUVmax compared with N2-N3 tumors (4.2 vs 7.3, respectively; p = 0.063). Stage III tumors presented a lower SUVmax compared with patients classified as stage IV (10.5 vs 12, respectively; p = 0.45). Finally, primary tumor SUVmax in patients undergoing surgery was slightly higher than in patients undergoing radiotherapy (12 vs 11.7; p = 0.48).
The distribution of SUVmax > 5.4 according to nodal stage was as follows: 20 patients (71.4%) had stage N1-N2 and 8 patients (28.6%) had N3 nodal staging whereas all patients [24] with nodal SUVmax ≤ 5.4 were included in the N1-N2 nodal staging (p = 0.005).
Prognostic factors analysis
Overall survival
Overall, 28 patients (48.3%) died. The mean OS for the whole population was 34.9 months (C.I 95%; 29.9–40.1).
Regarding clinical parameters influencing OS, only KPS, TNM stage and treatment modality were found statistically significant (see Supplementary Table S1).
In summary, patients with KPS < 80 vs ≥80% (p < 0.001), TNM stage IV (a-b) vs III (p = 0.037) and patients undergoing definitive radiotherapy vs surgery followed by radiotherapy (p = 0.042) were significantly associated with lower OS-rates. 2-year OS: was 0 vs 67.9%; 37.5 vs 87.5% and 48.6 vs 85.7%, respectively (see Supplementary Table S1). No other clinical parameters were significantly associated with OS. Moreover, SUVmax for the primary tumor or lymph nodes were not significantly related to OS (see Fig. 2 and Table S1). However, on multivariate analysis the KPS < 80% was the only independent prognostic factor (HR, 9.8; CI 3.2–29.4; p < 0.001).
On the other hand, data regarding CSS (death due only to HN cancer) are detailed in Table S2 (Supplementary Table 2). In brief, patients with KPS < 80 vs ≥80% (p = 0.002), TNM stage (p = 0.025) and tumor location (p = 0.047) were significantly associated with lower CSS. In multivariate analysis only the KPS < 80% (HR, 8.9; 95% CI 2.2–36.5; p = 0.002) and tumor location (HR, 8.1; 95% CI 1.4–46.7; p = 0.019) in patients classified as others (oral cavity and nasosinusal carcinoma) remained significant independent prognostic factors.
Disease-free survival
At last follow-up, 31 patients (53.4%) presented recurrence of their disease. Mean time to recurrence for the whole population was 31.6 months. Only KPS was found to be a significant factor influencing DFS (see Supplementary Table S3). Regarding metabolic parameters, SUVmax for the primary tumor and lymph nodes were not significantly related to DFS (see Fig. 2).
Locoregional control
Overall, locoregional recurrence occurred in 13 patients (22.4%). Mean time to failure for the whole population was 43.2 months. Locoregional recurrences were as follows: five patients recurred exclusively locally, one patient presented regional recurrence exclusively, two patients presented local and regional recurrence at the same time, two patients presented regional and distant metastasis at the same time, and finally three patients presented local, regional and distant metastasis all together.
Only the KPS, the age and T stage were significantly associated with LRC (results are detailed in Supplementary Table S4).
However, no significant association was found between SUVmax (primary tumor or lymph nodes) and LRC (see Fig. 2).
According to multivariate analysis, the KPS (HR, 11.8; 95% CI 1.6–83.1; p = 0.01) and the age (HR, 4.7; 95% CI 1.4–15.6; p = 0.01) remained as statistically significant prognostic factors.
Distant metastasis-free survival
Distant metastases were noted in 18 patients (31%) with a mean time to progression of 38.9 months. On univariate analysis, nodal SUVmax was the only factor associated with decreased DMFS (see Table 2).
Patients presenting a SUVmax ≤ 5.4 had a mean DMFS of 41.7 months (36.1–47.2) comparing to 32.1 months (23.6–40.7) for patients who had a SUVmax > 5.4 (p = 0.016). See Fig. 3.
Indeed, patients with pretreatment SUVmax that exceeded the median value (5.4) of the cohort demonstrated inferior 2-year DMFS relative to patients with SUVmax ≤ the median value of the cohort, 53.1 vs. 80.9%, respectively.
Patients with a nodal SUVmax > 5.4 presented an increased risk for distant metastases (HR, 3.3; 95% CI 1.17–9.25; p = 0.023).
Patients with higher stage (IVb) showed a higher incidence of distant metastasis compared to stages III or IVa (see Fig. 3). However, this clinical trend was not statistically significant.
Discussion
This study evaluated the prognostic utility of pretreatment SUVmax, in a uniform cohort of locally advanced HNSCC patients treated with curative intent, either with definitive chemoradiation or surgery and postoperative radiotherapy. Regarding overall results, the OS, LRC, DFS and DMFS rates are similar to those reported in other studies [8, 10, 22].
The prognostic value of SUVmax in patients with HNSCC remains controversial, and many reports have indicated that it has positive or negative associations with outcome [24]. Recent contemporary studies [8, 9, 22, 25,26,27,28,29,30,31,32,33,34,35] evaluating the prognostic role of pretreatment SUVmax are summarized in Table 3. According to our results, the pretreatment SUVmax of nodal disease was prognostic for distant recurrence (p = 0.023).
However, no significant association was found between nodal SUVmax and other outcomes such as OS, DFS or LRC. Moreover, no association was found between primary tumor SUVmax and outcomes.
We found that patients with stages IVa or IVb presented a worse OS rate than patients with stage III. Patients with larger tumors (T3-T4 vs T1-T2) also presented a worse LRC. This issue has been previously demonstrated by several authors [13, 36].
Several other authors have stated that higher primary tumor SUVmax was associated with worse OS or LRC [22, 27]. Allal et al. demonstrated that a primary tumor SUVmax exceeding 4.76 was associated with poorer local control (p = 0.003) and DFS (p = 0.005) than SUVmax of ≤4.76 in 120 patients with HNSCC treated with radiotherapy or surgery ± radiotherapy [22].
Rommeser et al. also dichotomized the patient population according to the median SUVmax of the primary tumor (<15.8 vs. ≥15.8; range 4.5–33.8). However, SUVmax did not correlate with local control (p = 0.229) or OS (p = 0.661) [23].
In the present study, primary tumor SUVmax was not associated with OS, LRC or DFS. We found an increased metabolic tumor activity in higher T stages. Other authors have also suggested that FDG uptake not only reflects tumor burden/stage but also expresses, at least in part, some intrinsic biologic characteristics of the tumor [22]. However, according to our results, although the tumor size (T stage) negatively influenced in LRC (in univariate analysis), the increasing metabolic activity at the primary site did not. Several authors have also stated that primary tumor SUVmax was not a good predictor for outcomes [8, 9, 23, 25, 29, 31, 32, 34], which is in agreement with our results (see Table 3).
In our series, nodal SUVmax rather than the primary tumor was significantly associated with DMFS. A similar tendency has also been reported in some previous studies [27, 28]. Kubicek et al. [27] showed that a nodal SUVmax exceeding 10.0 posed a greater increased risk of distant failure in 212 patients with HNSCC (p < 0.05). Inokuchi et al. [28] also reported that a nodal SUVmax exceeding 6.0 posed a greater risk of poor outcome regarding DMFS in 178 patients presenting with HNSCC carcinoma of in different subsites such as oral cavity, larynx, pharynx, or nasal sinus treated with chemoradiation (p = 0.016; 95% CI 1.25–8.92). However, in our study, nodal SUVmax was not associated with OS or LRC. Romesser et al. [9] found similar results (Table 3).
In this context, according to Tang et al. [31] total SUVmax (defined as the maximum of the primary tumor and nodal SUVmax) also failed to predict survival or local–regional progression (p = 0.54). However, it predicted distant metastatic failure (p = 0.026) (Table 3), which is in agreement with our results.
The data of the present study suggest that high FDG uptake in neck nodes is correlated with poor outcome. These patients may benefit from more aggressive treatment combinations. However, there is no currently evidence to support that this type of patients should receive different treatment approach. Hopefully, these parameters could be used to stratify patients in future clinical trials.
Regarding performance status it has been reported that patients with good performance status can benefit from more intensive treatments than patients with low performance status [5]. We found that patients with a KPS < 80% presented a worse DFS, LRC and OS. Indeed, most trials evaluating patients undergoing radical treatments usually include patients with a good performance status (IK ≥ 80%). Moreover, also in other tumor locations than HN, such as lung cancer it has been consistently reported that KPS ≥ 80% is positively associated with better survival [37]. Therefore, our results are in line with previous reports in the literature. Probably (according to our results), patients with KPS < 80% should not have been selected as candidates for treatment with radical intent. However, these results should be interpreted with caution considering that only a small number of patients (5/58) included in our study presented an IK < 80%.
Patients that underwent surgery and postoperative irradiation (with or without chemotherapy) presented a better OS than patients that underwent definitive radiochemotherapy. We do not have a clear explanation for this finding. However, it should be stressed that in our study there were 43 and 24% of patients with tumors located in the larynx in the group undergoing surgery and in the group undergoing radiotherapy, respectively. Considering that laryngeal tumors have better prognosis [36] than other sites including hypopharynx or oral cavity, we consider that this fact may have influenced our results. The evidence regarding whether patients with higher SUV should receive surgery instead of radiotherapy is scarce. In this context, Rogh et al. [38] reported that high FDG uptake is associated with poor survival in patients with advanced laryngopharyngeal SCC. Patients with SUV > 8.0 in the surgery group tended to have a higher 3-year DFS than those in the RT group (48% vs. 27%, p = 0.085), and therefore recommended that patients with high FDG uptake may be better treated by surgical resection.
Nowadays, PET imaging represents an area of very active research in oncology. Besides providing useful diagnostic information regarding pretreatment staging [11, 12], treatment decision and post-treatment follow-up [39], and intensity of FDG uptake is emerging as a valuable predictive factor regarding treatment outcome [11, 31, 35, 40, 41].
We acknowledge several limitations in our study. It should be stressed that SUV estimates suffer from poor reproducibility between centers because of the lack of standardization of the acquisition and processing protocols. Moreover, when considering the SUV, there is no standard cut-off for defining subgroups of differing prognoses. This makes direct comparison of different studies somewhat difficult.
Although widely used, SUVmax has a certain disadvantage. It is a single-pixel value representing the most intense FDG uptake in the tumor and may not represent total uptake for the whole tumor mass. More recently, volume-based metabolic parameters measured by FDG PET such as metabolic tumor volume (MTV) and total lesion glycolysis (TLG) have emerged as new and more reliable prognostic factors [24] [41, 42] (also see Table 3). Unfortunately, in our series, we were unable to measure MTV and TLG. This is one of several limitations of the present study. Our results should also be considered with caution considering that this study was performed at a single institution with a relatively small number of patients.
However, clinical factors such as stage and treatment were very homogenous within the cohort. Our results strongly indicate that pretreatment nodal FDG uptake provides additional outcome information, above that yielded by more traditional clinical or therapeutic parameters, especially regarding DMFS. These patients are considered at increased risk of distant failure and may benefit from more aggressive multimodality treatment combinations.
Conclusion
Identification of novel pretreatment prognostic factors that potentially predict long-term outcome is of great interest to tailor the treatment approach to individual patients with locally advanced HNSCC. Nodal SUVmax is strongly and negatively correlated with DMFS. However, given that some uncertainty still exists regarding the question which metabolic parameter is the strongest predictor for outcomes after treatment of HNSCC, prospective multicentric trials are needed to definitively settle this issue.
References
Chiesa F, Mauri S, Tradati N, Calabrese L, Giugliano G, Ansarin M, et al. Surfing prognostic factors in head and neck cancer at the millennium. Oral Oncol. 1999;35(6):590–6.
Haberkorn U, Strauss LG, Reisser C, Haag D, Dimitrakopoulou A, Ziegler S, et al. Glucose uptake, perfusion, and cell proliferation in head and neck tumors: relation of positron emission tomography to flow cytometry. J Nucl Med Off Publ Soc Nucl Med. 1991;32(8):1548–55.
Minn H, Clavo AC, Grénman R, Wahl RL. In vitro comparison of cell proliferation kinetics and uptake of tritiated fluorodeoxyglucose and l-methionine in squamous-cell carcinoma of the head and neck. J Nucl Med Off Publ Soc Nucl Med. 1995;36(2):252–8.
Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349(22):2091–8.
Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11(1):21–8.
Pignon J-P, le Maître A, Maillard E, Bourhis J. MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2009;92(1):4–14.
Bourhis J, Lapeyre M, Tortochaux J, Rives M, Aghili M, Bourdin S, et al. Phase III randomized trial of very accelerated radiation therapy compared with conventional radiation therapy in squamous cell head and neck cancer: a GORTEC trial. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(18):2873–8.
Higgins KA, Hoang JK, Roach MC, Chino J, Yoo DS, Turkington TG, et al. Analysis of pretreatment FDG PET SUV parameters in head-and-neck cancer: tumor SUV mean has superior prognostic value. Int J Radiat Oncol Biol Phys. 2012;82(2):548–53.
Romesser PB, Lim R, Spratt DE, Setton J, Riaz N, Lok B, et al. The relative prognostic utility of standardized uptake value, gross tumor volume, and metabolic tumor volume in oropharyngeal cancer patients treated with platinum based concurrent chemoradiation with a pre-treatment [(18)F] fluorodeoxyglucose positron emission tomography scan. Oral Oncol. 2014;50(9):802–8.
Kitajima K, Suenaga Y, Kanda T, Miyawaki D, Yoshida K, Ejima Y, et al. Prognostic value of FDG PET imaging in patients with laryngeal cancer. PLoS One. 2014;9(5):e96999.
Cacicedo J, Navarro A, Del Hoyo O, Gomez-Iturriaga A, Alongi F, Medina JA, et al. Role of fluorine-18 fluorodeoxyglucose PET/CT in head and neck oncology: the point of view of the radiation oncologist. Br J Radiol. 2016;89(1067):20160217.
Cacicedo J, Fernandez I, Del Hoyo O, Dolado A, Gómez-Suarez J, Hortelano E, et al. Should PET/CT be implemented in the routine imaging work-up of locally advanced head and neck squamous cell carcinoma? A prospective analysis. Eur J Nucl Med Mol Imaging. 2015;42(9):1378–89.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
NCCN Clinical Practice Guidelines in Oncology. [Internet]. 2016 [cited 2016 Apr 04]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf.
Peters LJ, Goepfert H, Ang KK, Byers RM, Maor MH, Guillamondegui O, et al. Evaluation of the dose for postoperative radiation therapy of head and neck cancer: first report of a prospective randomized trial. Int J Radiat Oncol Biol Phys. 1993;26(1):3–11.
Ang KK, Trotti A, Brown BW, Garden AS, Foote RL, Morrison WH, et al. Randomized trial addressing risk features and time factors of surgery plus radiotherapy in advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2001;51(3):571–8.
Lee N, Mechalakos J, Puri DR, Hunt M. Choosing an intensity-modulated radiation therapy technique in the treatment of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2007;68(5):1299–309.
Grégoire V, Ang K, Budach W, Grau C, Hamoir M, Langendijk JA, et al. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2014;110(1):172–81.
Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefèbvre J-L, Greiner RH, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350(19):1945–52.
Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350(19):1937–44.
Bernier J, Vermorken JB, Koch WM. Adjuvant therapy in patients with resected poor-risk head and neck cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(17):2629–35.
Allal AS, Slosman DO, Kebdani T, Allaoua M, Lehmann W, Dulguerov P. Prediction of outcome in head-and-neck cancer patients using the standardized uptake value of 2-[18F]fluoro-2-deoxy-d-glucose. Int J Radiat Oncol Biol Phys. 2004;59(5):1295–300.
Romesser PB, Qureshi MM, Shah BA, Chatburn LT, Jalisi S, Devaiah AK, et al. Superior prognostic utility of gross and metabolic tumor volume compared to standardized uptake value using PET/CT in head and neck squamous cell carcinoma patients treated with intensity-modulated radiotherapy. Ann Nucl Med. 2012;26(7):527–34.
Castelli J, De Bari B, Depeursinge A, Simon A, Devillers A, Roman Jimenez G, et al. Overview of the predictive value of quantitative 18 FDG PET in head and neck cancer treated with chemoradiotherapy. Crit Rev Oncol Hematol. 2016;108:40–51.
La TH, Filion EJ, Turnbull BB, Chu JN, Lee P, Nguyen K, et al. Metabolic tumor volume predicts for recurrence and death in head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2009;74(5):1335–41.
Chung MK, Jeong H-S, Park SG, Jang JY, Son Y-I, Choi JY, et al. Metabolic tumor volume of [18F]-fluorodeoxyglucose positron emission tomography/computed tomography predicts short-term outcome to radiotherapy with or without chemotherapy in pharyngeal cancer. Clin Cancer Res Off J Am Assoc Cancer Res. 2009;15(18):5861–8.
Kubicek GJ, Champ C, Fogh S, Wang F, Reddy E, Intenzo C, et al. FDG PET staging and importance of lymph node SUV in head and neck cancer. Head Neck Oncol. 2010;16(2):19.
Inokuchi H, Kodaira T, Tachibana H, Nakamura T, Tomita N, Nakahara R, et al. Clinical usefulness of [18F] fluoro-2-deoxy-d-glucose uptake in 178 head-and-neck cancer patients with nodal metastasis treated with definitive chemoradiotherapy: consideration of its prognostic value and ability to provide guidance for optimal selection of patients for planned neck dissection. Int J Radiat Oncol Biol Phys. 2011;79(3):747–55.
Lim R, Eaton A, Lee NY, Setton J, Ohri N, Rao S, et al. 18F-FDG PET/CT metabolic tumor volume and total lesion glycolysis predict outcome in oropharyngeal squamous cell carcinoma. J Nucl Med Off Publ Soc Nucl Med. 2012;53(10):1506–13.
Lee SJ, Choi JY, Lee HJ, Baek C-H, Son Y-I, Hyun SH, et al. Prognostic value of volume-based 18 F-fluorodeoxyglucose PET/CT parameters in patients with clinically node-negative oral tongue squamous cell carcinoma. Korean J Radiol. 2012;13(6):752.
Tang C, Murphy JD, Khong B, La TH, Kong C, Fischbein NJ, et al. Validation that metabolic tumor volume predicts outcome in head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2012;83(5):1514–20.
Moon SH, Choi JY, Lee HJ, Son Y-I, Baek C-H, Ahn YC, et al. Prognostic value of 18F-FDG PET/CT in patients with squamous cell carcinoma of the tonsil: comparisons of volume-based metabolic parameters. Head Neck. 2013;35(1):15–22.
Abd El-Hafez YG, Moustafa HM, Khalil HF, Liao C-T, Yen T-C. Total lesion glycolysis: a possible new prognostic parameter in oral cavity squamous cell carcinoma. Oral Oncol. 2013;49(3):261–8.
Garsa AA, Chang AJ, Dewees T, Spencer CR, Adkins DR, Dehdashti F, et al. Prognostic value of (18)F-FDG PET metabolic parameters in oropharyngeal squamous cell carcinoma. J Radiat Oncol. 2013;2(1):27–34.
Schwartz DL, Harris J, Yao M, Rosenthal DI, Opanowski A, Levering A, et al. Metabolic tumor volume as a prognostic imaging-based biomarker for head-and-neck cancer: pilot results from Radiation Therapy Oncology Group protocol 0522. Int J Radiat Oncol Biol Phys. 2015;91(4):721–9.
Ju J, Wang J, Ma C, Li Y, Zhao Z, Gao T, et al. Nomograms predicting long-term overall survival and cancer-specific survival in head and neck squamous cell carcinoma patients. Oncotarget. 2016;7(32):51059–68.
Käsmann L, Janssen S, Schild SE, Rades D. karnosky performance score and radiation dose predict survival of patients re-irradiated for a locoregional recurrence of small cell lung cancer. Anticancer Res. 2016;36(2):803–5.
Roh J-L, Pae KH, Choi S-H, Kim JS, Lee S, Kim S-B, et al. 2-[18F]-Fluoro-2-deoxy-D-glucose positron emission tomography as guidance for primary treatment in patients with advanced-stage resectable squamous cell carcinoma of the larynx and hypopharynx. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2007;33(6):790–5.
Mehanna H, Wong W-L, McConkey CC, Rahman JK, Robinson M, Hartley AGJ, et al. PET-CT surveillance versus neck dissection in advanced head and neck cancer. N Engl J Med. 2016;374(15):1444–54.
Wong KH, Panek R, Welsh LC, Mcquaid D, Dunlop A, Riddell A, et al. The predictive value of early assessment after one cycle of induction chemotherapy with 18F-FDG PET/CT and DW-MRI for response to radical chemoradiotherapy in head and neck squamous cell carcinoma. J Nucl Med Off Publ Soc Nucl Med. 2016;57(12):1843–50.
Pak K, Cheon GJ, Nam H-Y, Kim S-J, Kang KW, Chung J-K, et al. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med Off Publ Soc Nucl Med. 2014;55(6):884–90.
Castelli J, Depeursinge A, de Bari B, Devillers A, de Crevoisier R, Bourhis J, et al. Metabolic tumor volume and total lesion glycolysis in oropharyngeal cancer treated with definitive radiotherapy: which threshold is the best predictor of local control? Clin Nucl Med. 2017;42(6):e281–e285
Author information
Authors and Affiliations
Contributions
JC developed and oversaw the study design, and drafted the manuscript. IF collected data and OdH provided and collected data. AN helped in the study design and coordination. AGI provided and collected data. LMI statistical analysis and interpretation of the data. JIP and JE performed the statistical analysis, interpretation of the results. JGS collected data JFO and ROZ collected data and carried out the treatment data and designed treatment plans. PB provided and collected data. DR performed the interpretation of the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Human rights ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cacicedo, J., Fernandez, I., del Hoyo, O. et al. Prognostic value of maximum standardized uptake value measured by pretreatment 18F-FDG PET/CT in locally advanced head and neck squamous cell carcinoma. Clin Transl Oncol 19, 1337–1349 (2017). https://doi.org/10.1007/s12094-017-1674-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-017-1674-6