Abstract
Background
The role of the interaction between tumor cells and inflammatory cells in gallbladder carcinoma (GBC) is unclear. Inflammatory cells exist in both the tumor immune microenvironment and the host peripheral blood circulatory system. In the current study, we examined the prognostic value of inflammatory cells in the tumor microenvironment and peripheral blood in patients with GBC.
Methods
98 patients with GBC were recruited in this retrospective study. Using immunohistochemistry, we examined tumor-infiltrating CD3+ generic T-cells, CD8+ cytotoxic T-cells, CD45RO+ memory T-cells, and CD15+ neutrophils. Peripheral venous blood samples were also collected, and absolute neutrophil count (ANC), absolute lymphocyte count (ALC) and neutrophil/lymphocyte ratio (NLR) were measured. The relationships between these variables and patient outcome were evaluated.
Results
Survival analysis revealed that the density of CD3+ cell infiltrates in the tumor microenvironment was positively correlated with overall survival (OS) and the density of CD15+ cell infiltrates was negatively correlated with the OS. The combined analysis showed that a high density of CD3+ cell infiltrates combined with a low density of CD15+ cell infiltrates was an independent prognostic factor for GBC. In peripheral blood, survival analysis suggested that ANC and NLR were negatively correlated, while ALC was positively correlated with OS. Multivariate survival analysis showed that NLR was an independent prognostic factor for gallbladder cancer prognosis.
Conclusions
The results indicate that the combination of high density of CD3+ cell infiltrates combined with a low density of CD15+ cell infiltrates in tumor samples and pretreatment peripheral blood NLR were independent prognostic factors in patients with GBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gallbladder carcinoma (GBC) is the most common cancer of the biliary tract and the sixth most common gastrointestinal cancer [1]. It has characteristics of local invasion, lymph node metastasis, vascular invasion and distant metastasis [2]. Tumor progression is now thought to be controlled by the balance between tumor invasion and a defence system whose major component is the host immune response. The host immune reaction, as observed by the presence of tumor-infiltrating lymphocytes (TILs), is one of the leading factors influencing the tumor microenvironment [3].
Multiple immunohistochemical studies have described the relationship between TILs and tumor progression or prognosis in several malignant tumor types, including esophageal and renal cell carcinoma, as well as pancreatic, cervical and colorectal cancer [4–8]. However, the relationship between immune cell infiltration and prognosis in GBC has not been clarified. Inflammation plays a role in tumorigenesis and progression in various cancers by promoting cancer cell proliferation and angiogenesis and metastasis, as well as affecting tumor response to systemic therapies. Also, changes in systemic inflammation and immune status are closely related to the occurrence and development of tumors, thereby affecting patient prognosis [9]. Changes in peripheral blood cell counts are considered as immune response-related indicators [10]. As commonly used clinical parameters for inflammation, peripheral blood immune cell counts have been regarded to be associated with the prognosis of various tumors [11]. However, it is not known whether peripheral blood inflammatory cell counts are related to GBC prognosis.
In the current study, we investigated the role of tumor-infiltrating inflammatory cells and peripheral blood inflammatory cell counts in prognosis of patients with GBC. Furthermore, we evaluated the independent prognostic factors for GBC. This indicated a close relationship between immune cell status and prognosis in GBC.
Materials and methods
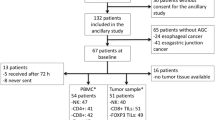
Initial screening identified 145 GBC patients who had undergone surgical treatment at the Qingdao Municipal Hospital from 2001 to 2013. Among these 145 patients, 98 were available with complete clinical and follow-up data and were enrolled in the current study. All data were obtained with the written informed consent of the patients prior to their inclusion in the study, according to the principles of the Declaration of Helsinki and approved by the Qingdao Municipal Hospital Ethics Commission.
The mean age of the patients was 63 years (range 39–88). The female/male ratio was 51/47. Each tumor sample was assigned a histological grade based on the World Health Organization (WHO) classification criteria. All patients were staged using the seventh edition of the International Union against Cancer (UICC) tumor–node–metastasis (TNM) staging system. Seven tumors were UICC stage I, 6 were stage II, 52 were stage III and 33 were stage IV. Information on post-resection adjuvant therapy was available for all patients: 8 received chemotherapy and radiotherapy, 4 received chemotherapy alone, 2 received radiotherapy alone and 84 did not receive any post-resection therapy. OS was measured from the date of surgery to the date of death or last follow-up for surviving patients. Clinical characteristics of patients, including age, gender, pathological types, degree of differentiation, TNM stage, incisal margin and operation modes were evaluated. Peripheral venous blood samples of 98 patients with GBC were collected within one week before surgery to detect absolute neutrophil count (ANC), absolute lymphocyte count (ALC), and the neutrophil/lymphocyte ratio (NLR).
Immunohistochemistry
Formalin-fixed paraffin-embedded surgical specimens were used for the immunohistochemical analysis. The presence of sufficient tumor tissue for immunohistochemical analysis was confirmed by haematoxylin and eosin staining. From each tissue block, we obtained four sections for immunohistochemical analysis (Supplementary Table 1). Sections were deparaffinized and rehydrated using graded ethanol. For antigen retrieval, the slides were immersed in EDTA (1 mmol/L, pH 8.0) and boiled for 3 min in a pressure cooker. After rinsing with PBS, endogenous peroxidase was blocked with 3 % hydrogen peroxide for 15 min at room temperature. The slides were incubated with the diluted primary monoclonal antibody (Zhongshan Golden Bridge Biotech, Beijing, China) in a moist chamber at 4 °C overnight. After primary antibody incubation, the slides were washed three times with PBS. The sections were then incubated with horseradish peroxidase-conjugated secondary antibody (Zhongshan Golden Bridge Biotech) for 30 min at room temperature. Following this incubation, the slides were washed three times in PBS. Finally, DAB was used to visualize the signal, and the sections were counterstained with 20 % haematoxylin. Each sample was incubated using the same isotype antibody dilution under the same experimental conditions for the negative control. For the positive controls, normal tonsil tissues and Hodgkin’s lymphoma tissues were stained for CD3, CD8, CD45RO and CD15.
Quantitative evaluation of tumor-infiltrating immune cells
After immunohistochemistry, the microscope images were imported as digital photo files using an inverted microscope (Olympus IX81, Japan), and we selected three areas that contained the most positively stained cells in each tissue section under 400× magnification. Areas that were confirmed under high magnification to contain invasive proliferating cancer cells were selected for further analysis. At 400× magnification, immunolabelled lymphocytes and neutrophils (except intravascular neutrophils) were counted by two independent investigators [9]. These observers were blinded to each other as well as to the clinical information regarding the outcome of the patients. The averages of the counts obtained for the three areas by the two observers were compared, and when the difference between their counts was <20 %, the average of the two was used as the final count. If the difference exceeded 20 %, the observers discussed the reasons for this difference and performed recounts until the difference became <20 %.
Statistical analysis
Quantitative values are expressed as mean ± SD or the median (range). The median values for all immunohistochemical variables and peripheral immune cell counts were used as the cutoff values for those variables. The Chi-squared test and nonparametric Wilcoxon matched-pairs test were used to assess the relationship between tumor-infiltrating immune cells, systemic inflammatory response and clinicopathological features. For the univariate analysis, survival curves were obtained using the Kaplan–Meier method and were compared by the log-rank test. The Cox proportional hazards regression model was used to identify independent prognostic factors, and P value <0.05 indicated significant differences.
Results
The relationship between tumor-infiltrating lymphocytes and clinicopathological factors in GBC.
Immunohistochemical stains were available for CD3, CD8, CD45RO in all 98 cases and for CD15 in 95 cases. The main clinical and histopathologic parameters of the study patients are summarized in Table 1. The following rates of immune marker expression were observed: CD3, 81.6 % (79 of 98); CD8, 52 % (51 of 98); CD45RO, 93.9 % (92 of 98); and CD15, 83.1 % (79 of 95). The median densities of CD3+, CD8+, CD45RO+ and CD15+ cells were 22.75, 1.17, 31.33 and 3.20 cells/HPF, respectively (Fig. 1). The median densities were used to separate the patients into high- and low-staining density groups. The infiltrating density of CD3+ cells was 49 cells/HPF in the clinical stage I + II groups and 20 cells/HPF in the clinical stage III + IV groups, and the CD3+ staining density significantly correlated with TNM stage (P < 0.05, Fig. 2a). GBC can be classified as moderately and poorly differentiated. Of the 83 invasive carcinomas, the density of CD3+ cells progressively decreased with the loss of histological differentiation (11 cells/HPF in the poorly differentiated group and 33 cells/HPF in the moderate to well differentiated group), and this difference was significant (P < 0.05, Fig. 2b). The levels of the other immune markers examined in tumor-infiltrating immune cells did not correlate with tumor grade. Among all the 98 gallbladder cancer patients, 78 were diagnosed as adenocarcinoma, 15 were malignant adenoma, 3 were squamous carcinoma, and 2 were adenosquamous carcinoma. The relationship between prognosis and infiltration density of inflammatory cells was analyzed between adenocarcinoma and malignant adenoma. The densities of CD3+ and CD45RO+ inflammatory cells in adenocarcinoma were lower than in adenoma, but the difference was not significant (P > 0.05, Fig. 2c).
a Distribution of tumor-infiltrating inflammatory cells in TNM stageI + II and III + IV. P values are calculated by nonparametric Wilcoxon matched-pairs test. Significance values were *P < 0.05. b Densities of tumor-infiltrating inflammatory cells in poor differentiated group (poor) and in moderate to well differentiated group (good). The difference was significant, *P < 0.05. c Densities of tumor-infiltrating inflammatory cells in adenoma (type 1) and in adenocarcinoma (type 2). The densities of CD3+ and CD45RO+ inflammatory cells in adenocarcinoma were lower than in adenoma, but the difference was not significant (P > 0.05)
The effect of inflammatory cell infiltrates on GBC patient survival
Kaplan–Meier survival analysis showed a correlation between higher infiltration levels and OS for CD3+ and CD15+ inflammatory cells but not for CD8+ and CD45RO+ inflammatory cells (Fig. 3). OS significantly differed between patients with high and low CD3+ densities (median: 18 vs 12 months, P < 0.05) and between patients with high and low CD15+ densities (median: 6 vs 22 months, P < 0.05). To more precisely determine the effects of tumor-infiltrating inflammatory cells on OS, we combined CD3+ and CD15+ densities to generate new potential prognostic indicators. When examining tumor-infiltrating cells that expressed both CD3+ and CD15+, the combined CD3+ high-density and CD15+ low-density group survived longer than the CD3+ low-density and CD15+ high-density group (median: 18 vs 5 months, P < 0.05).
a–d Kaplan–Meier plots of OS in primary resected GBC patients according to CD3+, CD8+, CD45RO+, CD15+ tumor-infiltrating inflammatory cell densities. e Kaplan–Meier survival curves showing comparison of OS among four groups of patients divided on the basis of combinations of CD3+ and CD15+. P values obtained from log-rank test. *P < 0.05
The clinicopathological factors significantly associated with OS were pathological type, histological grade, tumor stage, lymph node metastasis, advanced pTNM stage, incision margin and operation mode (Table 2). A multivariate analysis of the variables found to be significant by univariate analysis revealed that the combination of CD3+ low density and CD15+ high density was an independent prognostic factor for OS (Table 3).
The relationship between peripheral blood inflammatory cells and clinicopathological factors
In patient peripheral blood, the median pretreatment absolute neutrophil counts (ANC), absolute lymphocyte counts (ALC) and the neutrophil/lymphocyte ratio (NLR) were 4.03, 2.06, and 2.04/nL, respectively. The cutoff points are shown as the median. The main clinical and histopathologic parameters of the study patients are also summarized in Table 1. ANC were 3.02/nL in the clinical stage I + II group and 4.23/nL in the clinical stage III + IV group and the ANC significantly correlated with TNM stage (P < 0.05). ALC were 2.34/nL in the clinical stage I + II group and 1.94/nL in the clinical stage III + IV group and the ALC significantly correlated with TNM stage (P < 0.05). NLR increased in parallel with the advancement of clinical stage (1.35/nL in the stage I + II group and 2.19/nL in the stage III + IV group, P = 0.017) (Fig. 4a). The levels of ALC correlated with tumor grade (1.63/nL in high grade and 2.04/nL in low grade, P = 0.033) (Fig. 4b). Compared with malignant adenoma, NLR increased in adenocarcinoma (1.29 vs 2.09/nL, P = 0.026), while the lymphocyte count decreased (2.47 vs 1.90/nL, P = 0.025) (Fig. 4c).
a Peripheral blood inflammatory cell counts in TNM stageI + II and III + IV. ANC, ALC and NLR were different in TNM stage I + II and III + IV. *P < 0.05. b Peripheral blood inflammatory cell counts in the different tumor grade groups. ALC was significantly different, *P < 0.05. c Peripheral blood inflammatory cell counts in adenoma (type 1) and in adenocarcinoma (type 2). ALC and NLR were different in type 1 and type 2, and the difference was significant (P < 0.05)
Effect of peripheral blood inflammatory cells on GBC patient survival
Patients assigned to the high ALC group (ALC ≥2.06/nL) were documented to have superior OS (15 vs 6 months, P = 0.002) than those in the low ALC (<2.06/nL) group, whereas worse OS (17 vs 6 months, P = 0.011) was found in patients with increased ANC (≥4.03/nL), compared to those with decreased ANC (<4.03/nL). In addition, in contrast to patients in the elevated NLR group, patients with reduced NLR tended to have superior OS (6 vs 22 months, P < 0.001) (Fig. 5). The univariate survival analysis showed that the pathological types, histological grade, TNM stage, resection margin, operation mode and NLR were significantly related to the median survival period (Table 2). Furthermore, the multivariate prognosis analysis showed that pathological type, TNM stage, operation mode, and NLR (P = 0.004) were independent prognostic factors in GBC patients (Table 3).
Correlations between tumor-infiltrating and peripheral blood inflammatory cells
Further analysis of the correlation between inflammatory cells in the tumor microenvironment and inflammatory cells in peripheral blood showed that the infiltration density of CD3+, CD8+ and CD45RO+ T-cells does not correlate with ALC in peripheral blood (r = 0.051, P = 0.619; r = −0.067, P = 0.515; r = −0.031, P = 0.761). In addition, the infiltration density of CD15+ cells does not correlate with ANC in peripheral blood (r = 0.001, P = 0.992).
Discussion
The immune system is now commonly accepted to play a dual role in cancer development and progression. It can eradicate malignant cells via the regulated actions of its innate and adaptive branches to prevent tumor growth. Conversely, it can actively promote malignant cell growth, invasive capacity and metastatic ability [12]. Lymphocytes and neutrophils, which constitute the predominant proportion of total circulating leukocytes, play a key role in the host systemic immune response, but they mainly affect tumor progression via activities in the tumor microenvironment [13]. In the present study, we investigated the prognostic value of tumor-infiltrating inflammatory cells and peripheral blood inflammatory cells in GBC. Our study is the first to show that the densities of CD3+ and CD15+ tumor-infiltrating inflammatory cells are predictors of OS; furthermore, our multivariate analyses showed that the combination of CD3+ and CD15+ intratumoral cell densities were a significant and independent predictor of OS. Also, we found that a high lymphocyte count and low neutrophil count in peripheral blood were favorable prognostic factors and NLR was an independent prognostic factor in patients with GBC.
Tumor-infiltrating inflammatory cells
Tumor cells are often surrounded by infiltrating inflammatory cells, particularly lymphocytes and neutrophils. It is well recognized that lymphocytes constitute one of the most important effector mechanisms of anti-tumor immunity. T lymphocytes, the hallmark of cell-mediated adaptive immunity, are considered essential in tumor immunosurveillance [14]. We selected a panel of T-cell markers that represents the most validated and studied adaptive immune cells: CD3 (generic T-cell marker), CD45RO (memory T cells) and CD8 (cytotoxic T cells). We found that a high density of CD3+ cell infiltration and low density of CD15+ cell infiltration was associated with longer survival in GBC. In a previous study of a smaller cohort of GBC patients (n = 45), a high density of intratumoral infiltration of CD4+/CD8+ lymphocytes was associated with good prognosis, independent of tumor stage and nodal stage [15]. However, we did not find CD8+ lymphocyte infiltration to be a prognostic factor for GBC. CD45RO is the most suitable single marker of the memory T-cell population in humans and clearly indicates the activation status of T cells. Recent studies have reported that a high density of infiltrating CD45RO+ cells correlated with good clinical outcomes in several human cancers [16–18]. The current study examined the prognostic influence of intratumoral CD45RO+ memory T lymphocytes in primary resected GBC (n = 98). However, the OS did not differ between patients with high and low CD45RO+ density. Therefore, further research is needed to determine whether CD45RO+ is a valuable prognostic marker in GBC.
Neutrophils constitute a significant portion of the inflammatory cell infiltrate found in a wide variety of human cancers [19–21]. Several pieces of evidence have shown that neutrophils promote cancer cell migration and invasion as well as tumor-induced angiogenesis [22, 23]. The majority of clinical studies of tumor-infiltrating neutrophils (TIN) have demonstrated that their presence and high density are associated with poor clinical outcomes, including decreased survival [20, 24, 25] Because the role of CD15+ TINs in GBC has not been previously described, we herein evaluated the prognostic significance of CD15+ inflammatory cells by immunohistochemical analysis. We found that a high density of CD15+ TINs correlated with poor clinical outcome in GBC patients (median: 6 vs 22 months, P < 0.05). However, the level of CD15+ TINs alone was not found to be an independent prognostic factor for OS.
In the tumoral region of GBC, infiltrating neutrophils may suppress the response of CD3+ lymphocytes and thereby allow tumor cells to escape immune surveillance. However, in our study, the density of neutrophils was not correlated with that of CD3+ lymphocytes, which suggests that the recruitment of these two types of immune cells may differ and not be directly related.
Peripheral blood inflammatory cells
In the last decade, pretreatment peripheral differential leukocyte levels have been observed to be associated with prognosis in various cancers. High neutrophil counts have been proposed as a poor independent prognostic factor in patients with metastatic melanoma [26]. A high preoperative lymphocyte count was also reported as an independent favorable prognostic factor in patients with pancreatic ductal adenocarcinoma [27]. An elevated blood neutrophil count and elevated blood neutrophil/lymphocyte ratio (NLR) has been found to be related to an adverse outcome in patients with renal cell carcinoma, colorectal cancer, hepatocellular carcinoma, cholangiocarcinoma, glioblastoma, GIST, gastric, esophageal, lung, ovarian and head and neck cancer [11]. In agreement, we found significantly lower lymphocyte counts and higher neutrophil counts and NLR associated with shorter OS in patients with GBC.
Neutrophils are the main population of leukocytes in the blood and are considered the first line of the immune response to tissue injury. Besides a well-established function in host defence against bacterial infection, neutrophils are the major mediators of cancer-related inflammation. Circulating neutrophils have been shown to produce cytokines and vascular endothelial growth factor, which contribute to cancer progression. Therefore, a high peripheral neutrophil level may indicate a cancer-related inflammation or tumor progression, and predict poor prognosis.
Lymphocytes are crucial components of the adaptive immune system which surveys the body for tumors and also prevents maturation of tumor cells. A low peripheral lymphocyte level may indicate a poorer lymphocyte-mediated anti-tumor response. NLR shows the relative change between neutrophils and lymphocytes, and to some extent reflects the balance between inflammatory response at the site of a tumor and anti-tumor immunity. Through a study on the impact of NLR on the prognosis of 145 patients with GBC, we found that NLR was an independent risk factor of patient prognosis after surgical operation [28].
A previous study has shown the close relationship between circulating inflammatory markers and GBC [29]. This research further analyzed the influence of neutrophils and lymphocytes on prognosis, and found that though both could affect the GBC patient prognosis, they were not independent prognostic risk factors according to COX regression analysis. As an increase of neutrophils in both the tumor microenvironment and peripheral blood was considered as an adverse factor for patient prognosis, we analyzed the correlation between them, but this was not significant. Likewise, though an increase of lymphocytes in both the tumor microenvironment and peripheral blood presented a positive prognostic effect, we found no correlation between these two measures. We, therefore, speculate that the small sample might be responsible.
Conclusions
We have demonstrated that the presence of tumor-infiltrating inflammatory cells with a low density of CD3+ and high density of CD15+ markers correlated with shorter survival in GBC patients. Moreover, this was an independent prognostic factor for GBC. We found that high lymphocyte counts and low neutrophil counts were favorable prognostic factors and NLR was an independent prognostic factor in patients with GBC. However, further studies are still necessary to investigate the roles of tumor-infiltrating inflammatory cells and peripheral blood immune cells among patients with GBC in larger patient cohorts.
References
Coburn NG, Cleary SP, Tan JC, Law CH. Surgery for gallbladder cancer: a population based analysis. J Am Coll Surg. 2008;207:371–82.
Butte JM, Matsuo K, Gönen M, D’Angelica MI, Waugh E, Allen PJ, et al. Gallbladder cancer: differences in presentation, surgical treatment, and survival in patients treated at centers in three countries. J Am Coll Surg. 2011;212:50–61.
Hiraoka N, Yamazaki-Itoh R, Ino Y, Mizuguchi Y, Yamada T, Hirohashi S, et al. CXCL17 and ICAM2 are associated with a potential anti-tumor immune response in early intraepithelial stages of human pancreatic carcinogenesis. Gastroenterology. 2011;140:310–21.
Vayrynen JP, Tuomisto A, Klintrup K, Makela J, Karttunen TJ, Makinen MJ. Detailed analysis of inflammatory cell infiltration in colorectal cancer. Br J Cancer. 2013;109:1839–47.
Schumacher K, Haensch W, Roefzaad C, Schlag PM. Prognostic significance of activated CD8+ T cell infiltrations within esophageal carcinomas. Cancer Res. 2001;61:3932–6.
Ino Y, Yamazaki-Itoh R, Shimada K, Iwasaki M, Kosuge T, Kanai Y, et al. Immune cell infiltration as an indicator of the immune microenvironment of pancreatic cancer. Br J Cancer. 2013;108:914–23.
Carus A, Ladekarl M, Hager H, Nedergaard BS, Donskov F. Tumor-associated CD66b+ neutrophil count is an independent prognostic factor for recurrence in localised cervical cancer. Br J Cancer. 2013;108:2116–22.
Hotta K, Sho M, Fujimoto K, Shimada K, Yamato I, Anai S, et al. Prognostic significance of CD45RO+ memory T cells in renal cell carcinoma. Br J Cancer. 2011;105:1191–6.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The glasgow prognostic score, an inflammation based prognostic score, predicts survival in patients with hepatocellular carcinoma. BMC Cancer. 2013;13:52.
Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T, et al. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short-and long-term mortality in breast cancer patients. Ann Surg Oncol. 2012;19:217–24.
Donskov F. Immunomonitoring and prognostic relevance of neutrophils in clinical trials. Semin Cancer Biol. 2013;23(3):200–7.
Gutkin DW, Shurin MR. Clinical evaluation of systemic and local immune responses in cancer: time for integration. Cancer Immunol Immunother. 2014;63:45–57.
Wang J, Jia Y, Wang N, Zhang X, Tan B, Zhang G, et al. The clinical significance of tumor-infiltrating neutrophils and neutrophil-to-CD8+ lymphocyte ratio in patients with resectable esophageal squamous cell carcinoma. J Transl Med. 2014;12:7.
Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331:1565–70.
Nakakubo Y, Miyamoto M, Cho Y, Hida Y, Oshikiri T, Suzuoki M, et al. Clinical significance of immune cell infiltration within gallbladder cancer. Br J Cancer. 2003;89:1736–42.
Rauser S, Langer R, Tschernitz S, Gais P, Jutting U, Feith M, et al. High number of CD45RO+ tumor infiltrating lymphocytes is an independent prognostic factor in non-metastasized (stage I–IIA) esophageal adenocarcinoma. BMC Cancer. 2010;10:608–16.
Roxburgh CS, Richards CH, Macdonald AI, Powell AG, McGlynn LM, McMillan DC, et al. The in situ local immune response, tumor senescence and proliferation in colorectal cancer. Br J Cancer. 2013;109:2207–16.
Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353:2654–66.
Rice AJ, Griffiths AP, Martin IG, Dixon MF. Gastric carcinoma with prominent neutrophil infiltration. Histopathology. 2000;37:289–90.
Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H. Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol. 2009;27:4709–17.
Wislez M, Rabbe N, Marchal J, Milleron B, Crestani B, Mayaud C, et al. Hepatocyte growth factor production by neutrophils infiltrating bronchioloalveolar subtype pulmonary adenocarcinoma: role in tumor progression and death. Cancer Res. 2003;63:1405–12.
Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol. 2006;3:173–82.
Benelli R, Albini A, Noonan D. Neutrophils and angiogenesis: potential initiators of the angiogenic cascade. Chem Immunol Allergy. 2003;83:167–81.
Zhao JJ, Pan K, Wang W, Chen JG, Wu YH, Lv L, et al. The prognostic value of tumor-infiltrating neutrophils in gastric adenocarcinoma after resection. PLoS One. 2012;7:e33655.
Rao HL, Chen JW, Li M, Xiao YB, Fu J, Zeng YX, et al. Increased intratumoral neutrophil in colorectal carcinomas correlates closely with malignant phenotype and predicts patients’ adverse prognosis. PLoS One. 2012;7:e30806.
Schmidt H, Suciu S, Punt CJ, Gore M, Kruit W, Patel P, et al. American Joint Committee on Cancer Stage IV Melanoma; EORTC 18951. Pretreatment levels of peripheral neutrophils and leukocytes as independent predictors of overall survival in patients with American Joint Committee on Cancer Stage IV Melanoma: results of the EORTC 18951 Biochemotherapy Trial. J Clin Oncol. 2007;25(12):1562–9.
Shirai Y, Shiba H, Sakamoto T, Horiuchi T, Haruki K, Fujiwara Y, et al. Preoperative platelet to lymphocyte ratio predicts outcome of patients with pancreatic ductal adenocarcinoma after pancreatic resection. Surgery. 2015;158(2):360–5.
Zhang Y, Jiang C, Li J, Sun J, Qu X. Prognostic significance of preoperative neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in patients with gallbladder carcinoma. Clin Transl Oncol. 2015;17(10):810–8.
Wu XS, Shi BL, Li ML, Ding Q, Weng H, Wu WG, et al. Evaluation of two inflammation-based prognostic scores in patients with resectable gallbladder carcinoma. Ann Surg Oncol. 2014;21:449–57.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests to state.
Ethical standards
This study was approved by hospital medical ethics committee of the Qingdao Municipal Hospital.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Ma, C., Wang, M. et al. Prognostic significance of immune cells in the tumor microenvironment and peripheral blood of gallbladder carcinoma patients. Clin Transl Oncol 19, 477–488 (2017). https://doi.org/10.1007/s12094-016-1553-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1553-6