Abstract
Calcium sensing receptor, a pleiotropic G protein coupled receptor, activates secretory pathways in cancer cells and putatively exacerbates their metastatic behavior. Here, we show that various CaSR mutants, identified in breast cancer patients, differ in their ability to stimulate Rac, a small Rho GTPase linked to cytoskeletal reorganization and cell protrusion, but are similarly active on the mitogenic ERK pathway. To investigate how CaSR activates Rac and drives cell migration, we used invasive MDA-MB-231 breast cancer cells. We revealed, by pharmacological and knockdown strategies, that CaSR activates Rac and cell migration via the Gβγ-PI3K-mTORC2 pathway. These findings further support current efforts to validate CaSR as a relevant therapeutic target in metastatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The calcium sensing receptor (CaSR) controls parathyroid hormone (PTH) secretion in response to fluctuations of extracellular calcium. This G protein-coupled receptor (GPCR), in concert with PTH, regulates calcium removal from bone and renal calcium reabsorption (Brown and MacLeod, 2001; Riccardi and Valenti, 2016). Inherited point mutations in the CASR gene cause mild to severe parathyroid diseases characterized by altered calcium homeostasis (Mayr et al. 2016; Pollak et al. 1993). The structural consequences of these single amino acid changes and how they affect CaSR signaling are better understood in the context of the recent structural analysis of CaSR (Ling et al. 2021; Wen et al. 2021). Based on their localization, these mutations affect agonist binding, as those in the extracellular Venus Flytrap and cysteine-rich extracellular domains, or the conformational adjustments mechanistically linked to signal transduction, as those in the seven-helix transmembrane region or intracellular domains (Ling et al. 2021; Wen et al. 2021). CaSR functions as a constitutive homodimer which exhibits different conformations depending on the binding of agonists or allosteric modulators. In the active form, CaSR dimers are more compact and therefore the intracellular regions, involved in the dynamic association to signaling transducers and effectors, are closely engaged (Ling et al. 2021; Wen et al. 2021). Point mutations in these regions might affect the signaling properties not only of pathological CaSR variants known in parathyroid diseases, but also CaSR mutants potentially involved in cancer and other pathologies.
Beyond its physiological and pathological effects in the parathyroid glands, CaSR promotes contrasting effects in breast, colon and prostate cancer cells and contributes to tumor progression in mice models (Bhagavathula et al. 2005; Joeckel et al. 2014; Liao et al. 2006a; Sanders et al. 2000; Tennakoon et al. 2015). Specificities of CaSR signaling in various cancer cells might be related to cell differences on the available signaling repertoire, changes on CaSR expression and structural consequences of CaSR mutations. In colon cancer cells, elevated CaSR correlates with an ERK-dependent anti-proliferative effect linked to increased E-cadherin expression and differentiation (Bhagavathula et al. 2005). In the case of metastatic prostate cancer cells, CaSR promotes proliferation and AKT-dependent cell adhesion (Liao et al. 2006b). In breast cancer cells, CaSR promotes parathyroid hormone–related protein (PTHrP) production and proliferation, whereas in a conditional knockout mice model of breast cancer, ablation of CaSR slowed tumor growth (Kim et al. 2016). In breast cancer patients, elevated expression of CaSR was associated with significantly shorter survival (Kim et al. 2016), and might indicate metastatic progression (Mihai et al. 2006). Deep sequencing of human cancer genomes revealed that CASR is one of the most frequently mutated GPCRs (O'Hayre et al. 2013). An updated list of these mutations is maintained in the COSMIC v94 database (https://cancer.sanger.ac.uk/cosmic; (Tate et al. 2019)). Although the oncogenic capacity of mutant CaSR has not been fully characterized, it potentially contributes to the transforming effects of major driving oncogenes. These include PIK3CA, the gene coding for the catalytic subunit of phosphoinositide 3-kinase alpha (PI3Kα), which is frequently altered in the group of breast cancer patients with amplified or mutated CASR (https://www.cbioportal.org/ (Gao et al. 2013). To contribute to malignant transformation of breast epithelial cells, CaSR appears to switch its G-protein usage, gaining ability to couple to Gs as an abnormal mechanism to activate PKA-dependent production of PTHrP (Mamillapalli et al. 2008). Moreover, secretion of a variety of chemotactic, angiogenic, and growth factors by metastatic MDA-MB-231 breast cancer cells (MDA-MB-321 cells) is stimulated by CaSR (Hernandez-Bedolla et al. 2015), via the secretory Rab27b GTPase (Zavala-Barrera et al. 2021), indicating its potential to exacerbate the microenvironment in tumor settings. Furthermore, in metastatic tissues, overexpression of CaSR has been correlated with chemotactic behavior of cancer cells and with their osteolytic potential (Aguirre et al. 2010; Boudot et al. 2017; Olszak et al. 2000; Saidak et al. 2009; Yamaguchi et al. 1998a, 1998b). However, the molecular mechanisms by which CaSR promotes cell migration remain elusive.
The mechanistic target of rapamycin (mTOR) controls cell growth, proliferation, survival, and migration (Bracho-Valdes et al. 2011; Saxton and Sabatini, 2017; Wullschleger et al. 2006). This multifunctional kinase is the catalytic subunit of a rapamycin-sensitive complex, known as mTORC1, which reacts to nutritional status and energy levels (Bracho-Valdes et al. 2011; Saxton and Sabatini, 2017; Wullschleger et al. 2006). This signaling complex, the target of immunosuppressive therapies, controls cell growth by phosphorylating S6K1 (S6 kinase 1) and 4E-BP1 (eIF-4E binding protein 1), key regulators of protein synthesis (Bracho-Valdes et al. 2011; Saxton and Sabatini, 2017; Wullschleger et al. 2006). The mTOR kinase is also part of a distinct macromolecular and functional complex, known as mTORC2, containing Rictor, but not Raptor, as one of its defining subunits. This rapamycin-resistant complex phosphorylates AKT, widely known as a promoter of cell survival, but also recognized for its control over metabolic, proliferative, and cytoskeletal pathways (Bracho-Valdes et al. 2011; Huang and Fingar, 2014; Sarbassov et al. 2005). Although rapamycin does not inhibit mTORC2 catalytic activity, chronic treatment with this inhibitor prevents assembly of the mTORC2 complex (Bhaskar and Hay, 2007; Bracho-Valdes et al. 2011; Jacinto et al. 2004; Oh and Jacinto, 2011; Sarbassov et al. 2006).
To control cell migration, mTORC2 promotes dynamic adjustments of the actin cytoskeleton via Rho GTPase-dependent pathways (Jacinto et al. 2004; Sarbassov et al. 2004). Among the RhoGEFs linking mTOR signaling to cell migration, we identified P-Rex1 as an mTOR-interacting partner (Hernandez-Negrete et al. 2007). This guanine nucleotide exchange factor, specific for Rac, is activated by chemotactic GPCRs via PIP3 (phosphatidylinositol-3, 4, 5-triphosphate) and Gβγ (Cervantes-Villagrana et al. 2019, 2021; Hernandez-Negrete et al. 2007; Vazquez-Prado et al. 2016). Interestingly, Gβγ directly activates PI3Kβ and PI3Kγ, and also interacts with mTORC2, orchestrating chemotactic responses to agonists acting on Gi-coupled receptors (Houslay et al. 2016; Robles-Molina et al. 2014; Stephens et al. 1997). In the current study, we assessed how endogenous CaSR drives migration of MDA-MB-231 cells, and compared the wild type CaSR and four CaSR mutants in terms of their signaling to Rac and ERK pathways. These mutants differ by a single amino acid substitution, one of them at the first intracellular loop, other at the fourth transmembrane helix domain and two at the intracellular carboxyl-terminal region. The four CaSR mutants were found in breast cancer patients as reported in the Catalogue of Somatic Mutations In Cancer (COSMIC).
Materials and methods
DNA constructs, reagents, and antibodies
CaSR cDNA and anti-CaSR antibodies were kindly provided by Dr. Allen Spiegel (NIDDK/NIH); shRNA-CaSR was kindly donated by Dr. Laurie McCauley (University of Michigan). The CaSR mutants N639K, T732A, R886Q, V894I, R795W, and Δ895-1075 were obtained by the QuickChange™ mutagenesis kit (Stratagene) and confirmed by sequencing with the dRhodamine terminator cycle kit. Myc-mCherry-PKI was kindly provided by Dr. Silvio Gutkind (UC San Diego). PTX (Pertussis Toxin) was from MERCK & Co., Inc. The following antibodies were from Cell Signaling Technology, Inc.: anti-phospho-Erk p44/42 mitogen-activated protein kinase (MAPK (used at 1:40,000); Thr-202/Tyr-204); anti-phospho-mTOR (used at 1:10,000); anti-mTOR (used at 1:10,000); anti-phospho-S6 (used at 1:30,000; anti-S6 (used at 1:5,000); anti-phospho-S6K (used at 1:10,000); anti-S6K (used at 1:5,000); anti-pCREB Ser-133 (used at 1:30,000), and anti-CREB antibodies (used at 1:10,000). Anti-phospho-AKT (used at 1:5,000) and anti-AKT antibodies (used at 1:5,000) were from Santa Cruz Biotechnology, Inc. and RD Systems, respectively. Anti-Rac-1 antibody (used at 1:30,000) was purchased from BD Transduction Laboratories. The anti-mouse-HRP (used at 1:30,000) and anti-rabbit-HRP (used at 1:10,000) secondary antibodies were from Seracare KPL. R568 (calcimimetic) and NPS2143 (calcilytic) were from Tocris Bioscience.
Cell culture, transient transfection of wild type and CaSR mutant, lentiviral production, and cell infection
MDA-MB-231 and HEK-293 cells were maintained in DMEM (Sigma-Aldrich Co.) supplemented with 5% or 10% fetal bovine serum (FBS), respectively. HEK-293 cells were transfected as previously reported (Reyes-Cruz et al. 2001), using 2 µg of plasmid DNA and Lipofectamine (Invitrogen Co.) or Polyethylenimine (PEI, MW 25,000, from Polysciences, Inc.). MDA-MB-231 cells were transfected with control shRNA or shRNA-CaSR using Lipofectamine LTX and PLUS reagents (Invitrogen), as previously reported (Hernandez-Bedolla et al. 2015). HEK-293 and MDA-MB-231 cells were serum-starved in low calcium medium (prepared with calcium-free DMEM supplemented with 0.5 mM calcium) for 16 or 24 h, respectively. For experiments, cells were stimulated with 1 mM CaCl2 plus 1 µM R568 in MIX medium. This medium consisted of three volumes of calcium-free DMEM plus one volume DMEM containing 1.8 mM of calcium, but lacking sodium bicarbonate (MIX medium contains 0.45 mM calcium chloride) (Hernandez-Bedolla et al. 2015). Signaling inhibitors were added before cell stimulation as follows: PTX (200 ng/ml), 20 h; H89 (10 µM), rapamycin (20, 40, or 60 ng/ml), AG1478 (700 nM), UO126 (10 µM), wortmannin (Wm) (300 nM), 1 h, or U73122 (5 µM), 15 min as indicated in the Figure Legends. Then the cells were stimulated with calcium or 10 ng/ml EGF, as positive control. Lentiviral shRNA-Rictor was obtained as previously reported (Carretero-Ortega et al. 2010). Briefly, HEK-293 T cells (70% confluence) growing in 10-cm dishes were transfected with pTRIPZ-shRNA-Rictor or pTRIPZ-shRNA-control (2 μg), PAX2 packaging vector (1.8 μg), and pVSV-G (0.2 μg) (pTRIPZ Inducible Lentiviral shRNA was from GE Healthcare Dharmacon,Inc.) using Lipofectamine 2000 (Thermo Fisher Scientific, Inc.). The day after transfection, media were replaced, and viral supernatants were harvested at 48 and 72 h. MDA-MB-231 cells were incubated with media containing viral supernatants, previously filtered (0.45-μm filters) and supplemented with protamine sulfate (6 μg/ml; Sigma-Aldrich). After 4 h, media were substituted with fresh media. Cells were selected with 2 μg/ml puromycin for 5–7 days. Pilot studies confirmed that these conditions killed 100% of uninfected MDA-MB-231 cells. For knockdown experiments, pools of puromycin-resistant cells were induced with 2 μg/ml Doxycycline.
Immunoblot analyses
Serum-starved confluent cells were lysed with Buffer B containing 20 mM Tris–HCl (pH 7.5), 1 mM EDTA, 150 mM NaCl, 1% Triton X-100, 1 mM sodium vanadate, 1 mM NaF, 10 mM β-glycerophosphate, 1 mM PMSF, 1 μg/ml Leupeptin, and 1 µg/ml Aprotinin. Total cell extracts were forced through a 22-gauge needle (5–8 times) and centrifuged at 14,000 rpm for 15 min at 4 °C. Thirty micrograms of protein were resolved per lane on 6% or 10% SDS-PAGE and transferred onto nitrocellulose. Subsequently, membranes were incubated with the corresponding primary antibodies, followed by incubation with horseradish peroxidase-conjugated secondary antibodies and revealed by using autoradiography films and SuperSignal West Pico Substrate or ECL Western Blotting Substrate Chemiluminescent (Thermo Fisher Scientific). We normalized Westerns blots to low calcium concentrations, without R-568 (-, control or 0.25 mM), as these conditions are reported to have a minimal effect on CaSR signaling (Davey et al. 2012; Hauache et al. 2000).
Chemotactic and wound-healing assays
Cell migration was analyzed in Boyden chambers as reported (Hernandez-Bedolla et al. 2015). Briefly, the bottom wells of the chamber were filled with 159 μl of media containing or lacking 1 mM calcium in the presence or absence of 1 µM R568 as chemoattractant, 10% FBS was used as positive control. The lower part of the chamber was covered with gelatin-coated polycarbonate filters having 8-µm pores (Neuro Probe, Inc.). Filters were previously coated with 2% Gelatin (Calbiochem, Merck). MDA-MB-231 cells were placed in the upper wells of the chamber (100,000 cells/well). The effect of rapamycin, PTX, or wortmannin (Wm) on cell migration was assessed with cells previously treated with these agents for 24, 16, or 1 h, respectively. Chemotactic assays were carried out at 37 °C in a 5% CO2 atmosphere for 6 h. At the end of the experiment, cells in the filters were fixed with methanol, stained with 10 mg/ml crystal violet, and those that remained on the top side of the filter were removed with a cotton swab. Scratch assays were conducted as previously reported elsewhere (Liang et al. 2007). Briefly, serum-starved confluent MDA-MB-231 cells expressing pTRIPZ shRNA-Rictor or pTRIPZ shRNA-control were incubated in low calcium medium for 24 h. Then, they were incubated with 12 µM of mitomycin C (SIGMA) for 2 h at 37 °C in a 5% CO2 atmosphere. Cell monolayers were then scratched with a p20 pipette tip, washed with PBS, and stimulated with calcium and R568 for 24 h. Images were acquired with a 10X DIC objective using a Nikon Eclipse-TiE microscope. Densitometric analysis of cell migration was determined with ImageJ software (http://rsb.info.nih.gov/ij/).
Rac-GTP assay
Transfected HEK-293 cells or MDA-MB-231 cells, on 60-mm plates, were serum-starved in low calcium medium and stimulated with 1.5 mM calcium plus R568 for 3 min. Cells were washed with PBS containing 10 mM MgCl2 and lysed with 350 µl of ice-cold buffer B containing 10 mM MgCl2. Cell lysates were incubated with 40 µl of GST-CRIB beads for 45 min in a shaker. Beads were collected, washed three times with lysis buffer, and finally resuspended in 40 µl of Laemmli buffer, boiled for 5 min, and centrifuged at 13,000 rpm for 1 min. Proteins were resolved in 12% acrylamide gels, transferred onto nitrocellulose membranes, and immunoblotted using anti-Rac-1 monoclonal antibodies. As controls, total cell lysates were analyzed in parallel.
CASR-GNB1-MTOR pathway data mining
To address whether CASR and genes of the AKT-MTOR pathway were co-expressed in breast cancer tumors, transcriptomic datasets from 1084 patients/samples (TCGA, PanCancer Atlas) were obtained from cBioPortal (https://www.cbioportal.org/). This TCGA study includes six breast cancer types as follows: Invasive Ductal Carcinoma (n = 780); Invasive Lobular Carcinoma (n = 201); Invasive Carcinoma not otherwise specified (NOS, n = 77); Invasive Mixed Mucinous Carcinoma (n = 17); Metaplastic Breast Cancer (n = 8), and Invasive Breast Carcinoma (n = 1), the latter type was excluded from the analysis due to data unavailability. All transcripts were ordered according to the Spearman correlation value with co-expressed CASR and sorted by cancer type.
Statistics
Data are presented as the mean + standard deviation of the mean (SD) of at least three independent experiments. Blots were scanned at 300 dpi (dots per inch), background was subtracted, and densitometric quantitation of western blots was performed with ImageJ software. Statistical analysis was performed with version 6.0 GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Statistical tests are indicated in the Figure Legends. P < 0.05 was considered a statistically significant difference.
Results
CaSR mutants identified in breast cancer patients differ in their ability to stimulate Rac but not ERK
CaSR was identified as a mutated GPCR in cancer (O'Hayre et al. 2013). The COSMIC Cancer Genomics Database registers 1,012 mutations in the CASR gene (Fig. 1A) (https://cancer.sanger.ac.uk/cosmic/gene/analysis?ln=CASR_ENST00000639785#distribution), 32 of these in breast cancer patients (Fig. 1B). Point mutations that change the CaSR primary sequence are distributed throughout the extracellular, transmembrane, and intracellular regions of this receptor, which is a constitutive homodimer (Fig. 1C). Recent structural analysis of CaSR indicates that mutations in the extracellular Venus Flytrap domains affect agonist binding, whereas those in the 7-helix transmembrane domain might interfere on the conformational changes that bring CaSR monomers closer during agonist-elicited activation, affecting its signaling properties (Ling et al. 2021; Wen et al. 2021). Although the oncogenic impact of CaSR mutants found in breast cancer patients has not been characterized, we hypothesized that their signaling properties are likely affected by non-synonymous mutations that change its membrane or intracellular sequences. Therefore, we studied the signaling properties of CaSR mutants with single amino acid substitutions in the first intracellular loop (CaSR N639K), the fourth transmembrane domain (CaSR T732A), or the carboxyl-terminal region (CaSR R886Q, and CaSR V894I), as indicated in one of the subunits of the CaSR dimer shown in Fig. 1C (Protein Data Bank, 7DTV, (Ling et al. 2021)). All were expressed at similar levels as wild type CaSR and had comparable electrophoretic properties under reducing and non-reducing conditions in transfected HEK-293 cells (Fig. 1D).
CaSR mutants identified in breast cancer patients differ in their ability to stimulate Rac but not ERK. CaSR mutations detected in general (A) and in breast cancer patients (B), according to the COSMIC database. (C) Structure of CaSR dimers. Human Calcium-Sensing Receptor in the active state (Ling et al. 2021), corresponds to the 7DTV structure in the Protein Data Bank, the carboxyl terminal region was introduced in the model. The position of single amino acid changes in the CaSR mutants studied in this work is shown in the right CaSR monomer. (D) Expression of wild type and mutant CaSR. Electrophoretic mobility of wild type and mutant CaSR expressed in HEK-293. Immunoblots were revealed with the anti-CaSR ADD (1:15,000) monoclonal antibody. Cells transfected with empty vector served as control. (E) Hypothetical model showing CaSR signaling to Rac-GTPase via mTORC2. (F-I) CaSR mutants identified in breast cancer patients activate Rac-1 GTPase and the ERK pathway. Rac-1-GTP was isolated by pull-down with GST-PAK-CRIB-domain beads using lysates from HEK-293 cells transiently transfected with wild type CaSR or the indicated mutant. Cells were stimulated with R568 + extracellular calcium for 3 min, and isolated Rac-1-GTP was revealed by western blot. Graphs represent three independent experiments. Comparative analyses of Rac-1 activation by wild type and mutant CaSR (F-I, left panels). (F) Wild type CaSR vs N639K; * p = 0.0100, # p < 0.05; (unpaired Student t test; n = 3). (G) Wild type CaSR vs T732A; *p = 0.0226, # p = 0.0237; (unpaired Student t test; n = 3). (H) Wild type CaSR vs R886Q; **p = 0.0067, # p = 0.0256; (unpaired Student t test; n = 3). (I) Wild type CaSR vs. V894I; * p = 0.0232, *p = 0.0339; (n = 3). Comparative effect of wild type and CaSR mutants on ERK phosphorylation (F-I, right panels). HEK-293 cells expressing wild type CaSR or the indicated CaSR mutants were stimulated or not with 1 µM R-568 + 1.5 mM CaCl2 for 3 min. Graph represents the densitometric analysis of ERK phosphorylation. Bars represent mean ± standard deviation (SD). (F) Wild type CaSR vs N639K; ****p < 0.0001; (G) Wild type CaSR vs T732A; ** p = 0.0031, **p = 0.0064; (H) Wild type CaSR vs R886Q; *** p = 0.0005, **p = 0.0060; (I) Wild type CaSR vs. V894I; *** p = 0.0002, #p = 0.0151; (unpaired Student t test; n = 4)
Given that CaSR regulates breast cancer cell migration (Saidak et al. 2009), we aimed to address the signaling mechanisms involved in this process. We hypothesized that CaSR activates Rac via the PI3K/AKT/mTORC2 signaling pathway (Fig. 1E). We addressed this possibility in HEK-293 cells expressing wild type CaSR as well as the indicated CaSR mutants, and also compared their effects on ERK phosphorylation. To detect Rac activation, we used GST-PAK-CRIB beads to isolate Rac-GTP, which was revealed by western blot (Hernandez-Negrete et al. 2007). As depicted in Fig. 1F–I, extracellular calcium + R568 stimulated CaSR to activate Rac (Fig. 1F–I; Wt, left panels) and promoted ERK phosphorylation (Fig. 1F–I; Wt, right panels). These effects were inhibited by NPS-2143 (Supplemental Fig. 1A), an allosteric calcilytic characterized as a selective and potent CaSR antagonist (Nemeth et al. 2001). CaSR mutants exhibited differential abilities to stimulate Rac (Fig. 1F–I; Rac-GTP, left panels) but were similarly effective on Erk phosphorylation (Fig. 1F–I; pERK, right panels). CaSR N639K promoted the strongest effect on Rac (Fig. 1F), CaSR T732A was as effective as wild type CaSR (Fig. 1G), whereas CaSR R886Q had slightly increased baseline levels but did not elicit an agonist-dependent activation of Rac (Fig. 1H), despite that this mutant effectively activated ERK (Fig. 1H; pERK, right). Finally, CaSR V894I showed higher baseline activity on Rac, and exhibited a further increase when the receptor was stimulated (Fig. 1I). The CaSR mutants that activated Rac involved mTOR in the pathway as evidenced by the inhibitory effect of chronic rapamycin (Supplemental Fig. 1B–E).
Endogenous CaSR promotes Rac activation in MDA-MB-231 cells
To investigate how MDA-MB-231 cells migrate in response to stimulation of endogenous CaSR (Hernandez-Bedolla et al. 2015), we first analyzed the effect of R568 plus extracellular calcium on Rac activation in these cells. As depicted in Fig. 2A, in the presence of R568, 1- and 3-mM extracellular calcium promoted a significant increase in Rac activation. This response was inhibited by NPS-2143 (Fig. 2B) and was attenuated in shRNA-CaSR knockdown cells (Fig. 2C). These results confirmed the role of CaSR in the activation of Rac in MDA-MB-231 cells. Consistent with a potential role of AKT in this pathway, CaSR knockdown also prevented the activation of this serine/threonine kinase (Fig. 2C, third panel). The effect of CaSR as a promoter of Rac activation was also observed in human microvascular endothelial cells (HMEC) (Supplementary Fig. 2). Overall, our data indicate that endogenous CaSR activates Rac in MDA-MB-231 and HMEC cells, as it does in transfected HEK-293 cells, suggesting a broad potential of CaSR to activate Rac-dependent cellular effects.
Endogenous CaSR promotes Rac activation and cell migration in MDA-MB-231 cells. (A) Effect of CaSR stimulation on Rac-1 activation. MDA-MB-231 cells were stimulated for 10 min with R568 + calcium and total cell lysates were used to isolate Rac-1-GTP with GST-PAK-CRIB beads. The fraction of active Rac was revealed by western blot. Bars represent mean ± standard deviation (SD); * p = 0.0320; (one-way ANOVA followed by Sidak’s test; n = 3). (B) NPS-2143 prevents CaSR-dependent Rac-1 activation. Rac-1-GTP was detected by pull-down assays using lysates from MDA-MB-231 cells pre-incubated or not with 5 or 10 µM NPS-2143 before stimulation of CaSR. Bars represent mean ± SD, **p = 0.0022, ##p = 0.0032; (one-way ANOVA followed by Fisher test; n = 3). (C) CaSR knockdown prevents Rac-1 and AKT activation by R568 + calcium. Representative western blots showing CaSR knockdown and its effect on the activation of Rac-1 and AKT. (D) NPS-2143 prevents CaSR-dependent MDA-MB-231 cell migration. Cells were incubated in Boyden chambers to address the effect of extracellular calcium + R568 or NPS-2143 on CaSR-dependent cell migration. Bars represent mean ± standard deviation (SD), **p < 0.01, ###p < 0.001; (one-way ANOVA followed by Sidak's test; n = 3). (E) Effect of pertussis toxin (PTX) and wortmannin (Wm) on CaSR-dependent migration of MDA-MB-231 cells. Graph represents mean ± standard deviation (SD), *p = 0.0351, #p = 0.0445; (Student t test; n = 3). (F) Effect of chronic treatment with rapamycin (40 ng/ml) on CaSR-dependent MDA-MB-231 cell migration. Graph represents mean values, normalized to cell migration induced by fetal bovine serum (FBS); error bars represent SD, ***p = 0.001; (one-way ANOVA followed by Tukey’s; n = 3)
Endogenous CaSR promotes breast cancer cell migration
The metastatic behavior of breast cancer cells invading bone tissues is potentially linked to CaSR-dependent cell migration (Liao et al. 2006a; Saidak et al. 2009). Thus, we initially confirmed the role of CaSR in the chemotactic response of MDA-MB-231 cells to extracellular calcium (Saidak et al. 2009); then we addressed the signaling mechanisms sustaining this process. As shown in Fig. 2D, MDA-MB-231 cells demonstrated a significant chemotactic response to extracellular calcium in the presence of R568; this response was diminished by increasing the concentrations of NPS-2143. The chemotactic effect elicited by extracellular calcium and R568 was effectively reduced by inhibiting Gi with pertussis toxin and PI3K with wortmannin (Fig. 2E, PTX and Wm, respectively). We then tested whether the chemotactic migration of MDA-MB-231 cells, elicited by CaSR, involved mTORC2-dependent signaling pathways. As shown in Fig. 2F, chronic treatment with rapamycin inhibited the chemotactic effect elicited by CaSR. Thus, our results are consistent with the idea that CaSR stimulates MDA-MB-231 cell migration via a Gi/PI3K/mTORC2-dependent pathway.
CaSR regulates mTORC1 and mTORC2 signaling pathways in MDA-MB-231 cells
To characterize how CaSR activates mTORC1 complexes, we examined the effect of extracellular calcium and R568 on the phosphorylation of S6 in MDA-MB-231 cells (Fig. 3A) and of HEK-293 cells expressing CaSR (Supplementary Fig. 3A). S6 phosphorylation was maximal at 30 min and decreased at 60 min of calcium stimulation. In addition, in MDA-MB-231 cells, CaSR stimulated mTOR phosphorylation at Ser2448 (p-mTOR), which increased to above baseline levels at 5 min and decreased at 60 min (Fig. 3A, pmTOR). The effect of CaSR was prevented with NPS-2143 (Fig. 3B) as well as with Calhex (Supplementary Fig. 3B), a CaSR negative allosteric modulator. CaSR-induced S6 phosphorylation was inhibited with Gallein (Fig. 3C), a Gβγ-dependent signaling inhibitor (Casey et al. 2010; Tang et al. 2011), wortmannin (Fig. 3D, Wm), and by a 1-h incubation with rapamycin (Fig. 3E and Supplementary Fig. 3C). A similar effect was observed in the CaSR-dependent phosphorylation of S6K (p-S6K, Supplementary Fig. 3C). Phosphorylation of S6, downstream of mTORC1, was independent of the ERK pathway, as indicated by the lack of effect of U0126, which prevented the activation of ERK1/2 (Supplementary Fig. 3D). Then, we examined whether the activation of mTOR occurs via EGF-receptor transactivation, known to be relevant in proliferative signaling by CaSR (MacLeod et al. 2004; Tfelt-Hansen et al. 2005; Tomlins et al. 2005). As depicted in Supplementary Fig. 3D, AG1478, an inhibitor of the EGF-receptor tyrosine kinase, failed to suppress CaSR-dependent S6 phosphorylation; in contrast, it inhibited AKT phosphorylation. To further confirm the ability of CaSR to stimulate the mTOR pathway, we studied whether activating (CaSRΔ895-1075) or dominant negative (CaSR-R795W) CaSR mutants modulate mTOR signaling according to their phenotype (Bai et al. 1996, 1999; Lienhardt et al. 2000). As shown in Supplementary Fig. 3E, the phosphorylation of S6 (pS6) and mTOR at Ser2448 (pmTOR) were increased by extracellular calcium in cells expressing the CaSR-activating Δ895-1075 mutant. In contrast, the dominant negative CaSR-R795W mutant reduced mTOR and S6 phosphorylation. Our results indicate that CaSR activates mTORC1.
CaSR activates mTORC1 in MDA-MB-231 cells. (A) CaSR stimulates S6 phosphorylation. MDA-MB-231 cells were stimulated for 10 min with R568 + calcium at the indicated times. EGF was used as positive control. Total cell lysates were utilized for western blot analysis to reveal S6 phosphorylation, normalized to non-stimulated cells (NS) which was considered 100%. Bars indicate mean ± standard deviation (SD), *p = 0.0190; (Student t test; n = 3). (B) NPS-2143 calcilytic inhibits CaSR-dependent S6 phosphorylation in MDA-MB231. *p = 0.0247, #p = 0.0141, ##p = 0.0076; data was analyzed by one-way ANOVA followed by uncorrected Fisher; (n = 3). (C) Effect of Gallein on S6 phosphorylation stimulated by R568 + calcium. Error bars indicate SD, **p = 0.0096, #p = 0.0241; (unpaired Student t test; n = 3). (D) Effect of wortmannin (Wm) on S6 phosphorylation stimulated by CaSR in MDA-MB-231 cells. Error bars indicate SD, * p = 0.04; (one-way ANOVA followed by Bonferroni; n = 3). (E) Effect of rapamycin on CaSR-induced S6 phosphorylation in MDA-MB231 cells. Bars represent mean ± SD, **p = 0.01, ###p < 0.001; (one-way ANOVA followed by Tukey; n = 3)
Then we characterized the activation of mTORC2 as an effector of CaSR by assessing the phosphorylation of AKT at Ser473 (Fig. 4A) (Sarbassov et al. 2005). This mTOR signaling complex is characterized by the presence of Rictor and its resistance to acute inhibition by rapamycin; although chronic treatment with rapamycin prevents its assembly and has been utilized to address its functions (Sarbassov et al. 2006). CaSR promoted AKT phosphorylation (Fig. 4B and Supplementary Fig. 3D, F), which was attenuated with NPS-2143 (Fig. 4C and Supplementary Fig. 3F), Calhex (Supplementary Fig. 3F), Gallein (Fig. 4D), and wortmannin (Fig. 4E, Wm), indicating the participation of Gβγ and PI3K in the activation of mTORC2 by CaSR. As presented in Fig. 4F, CaSR promoted the phosphorylation of AKT and of PKC at 5 and 10 min of stimulation. In both cases, the effect was inhibited in cells pre-incubated for 24 h with rapamycin, revealing the involvement of mTORC2 in this pathway (Sarbassov et al. 2006), and further confirming that mTORC2 is an effector of CaSR. As shown previously, CaSR knockdown experiments were also consistent with the idea that CaSR stimulates the mTORC2 complex to activate AKT and Rac (Fig. 2C).
CaSR activates mTORC2 in MDA-MB-231 cells. (A) Hypothetical model of CaSR signaling to mTORC2 and downstream kinases. (B) Effect of CaSR stimulation on AKT phosphorylation in MDA-MB-231 cells. Bars represent mean ± standard deviation (SD), * p = 0.0118; (one-way ANOVA followed by Tukey; n = 3). (C) NPS-2143 calcilytic prevents CaSR-dependent phosphorylation of AKT in MDA-MB231 cells. Bars represent mean ± SD, *p = 0.0127, & p = 0.0127, ##p = 0.0033, ###p = 0.0004; (one-way ANOVA followed by uncorrected Fisher; n = 3). (D) Effect of Gallein on AKT phosphorylation stimulated by R568 + calcium. Bars indicate mean ± SD, **p = 0.0022, #p = 0.0198; (unpaired Student t test; n = 3). (E) Effect of wortmannin (Wm) on AKT phosphorylation in MDA-MB-231 cells. Bars indicate mean ± SD, *p < 0.05, ## p = 0.007; (one-way ANOVA followed by Bonferroni; n = 3). (F) Effect of rapamycin on CaSR-induced AKT and PKC phosphorylation. MDA-MB-231 cells were incubated for 24 h with rapamycin before stimulation with R568 + calcium for 5 or 10 min. Cell lysates were analyzed by western blot to detect AKT and PKC phosphorylation. Bars represent mean ± SD, **p < 0.01, #p < 0.05; (one-way ANOVA followed by Bonferroni; n = 3)
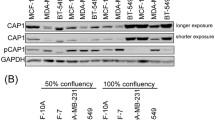
Rictor knockdown prevents CaSR-dependent Rac activation and cell migration in MDA-MB-231 cells
Initial results showing that CaSR-dependent cell migration and AKT activation in MDA-MB-231 cells were inhibited by chronic treatment with rapamycin (Figs. 2F and 4F) suggested that mTORC2 drives chemotactic pathways elicited by CaSR. Based on previous reports showing that Rac is activated downstream of mTORC2 (Hernandez-Negrete et al. 2007), we used Rictor-knockdown cells (Fig. 5A) to assess Rac activation by CaSR. Consistent with a central role of mTORC2 in CaSR-elicited signaling pathways driving cell migration, we found that CaSR-induced Rac-GTP (Fig. 5B) and cell migration, assessed as a chemotactic response (Fig. 5C), as well as in wound-healing assays (Fig. 5D), were notably reduced in Rictor-knockdown MDA-MB-231 cells (Figs. 5B-D). Taken together, our data indicate that CaSR, endogenously expressed in metastatic MDA-MB-231 cells, activates mTORC1 and mTORC2 complexes, promoting cell migration via Gβγ-PI3K and, as indicated by the Rictor knockdown experiments, it involves mTORC2 in this process (Fig. 5E).
mTORC2 participates in MDA-MB-231 cell migration elicited by CaSR. (A) Rictor-knockdown MDA-MB-231 cells. To achieve Rictor knockdown, cells were infected with lentiviral Rictor-shRNA. Bars represent mean ± standard deviation (SD) of Rictor expression (normalized to actin expression), ****p < 0.0001; (unpaired Student t test; n = 3). Anti-actin immunoblot served as loading control. (B) Effect of CaSR on Rac activation in control and Rictor-knockdown MDA-MB-231 cells. Control and Rictor-knockdown cells were stimulated for 10 min with R568 + calcium, and active Rac (Rac GTP) was isolated from cell lysates with GST-PAK-CRIB beads and revealed by western blot. Bars represent mean ± SD, ***p = 0.0009, ##p = 0.0091; (unpaired Student t test; n = 3). (C) Effect of Rictor-knockdown on CaSR-dependent MDA-MB-231 cell migration. Serum-starved Rictor-knockdown or control MDA-MB-231 breast cancer cells were stimulated with 2 mM calcium + 1 µM R568 ( +) for 6 h, or left in 0.25 mM calcium (-), EGF was used as control. Cell migration was tested in Boyden chambers. A representative filter is shown. Bars represent mean ± SD, **p = 0.005; (one-way ANOVA followed by Tukey; n = 3). (D) Effect of Rictor-knockdown on MDA-MB-231 cell migration in scratch assays. Wound-closure experiments were carried out with Rictor-knockdown and control MDA-MB-231 cells stimulated for 24 h with 2 mM calcium + 1 µM R568. Bars indicate mean ± SD, *p < 0.05, #p < 0.05; (one-way ANOVA followed Tukey’s; n = 3). (E) Model depicting how CaSR drives cell migration via the Gβγ/PI3K/AKT/mTORC2/Rac signaling pathway
Discussion
CaSR has been found to be mutated or overexpressed in cancer patients, indicating a potential contribution of this GPCR to cancer progression (Das et al. 2020; Iamartino et al. 2020). In the COSMIC database, this receptor was identified as one of the most frequently mutated GPCRs (O'Hayre et al. 2013). Here, we studied the signaling properties of four, not previously characterized, CaSR mutants originally identified in breast cancer patients (https://cancer.sanger.ac.uk/cosmic; (Tate et al. 2019)). Each had a single amino-acid substitution, one in the four transmembrane helix (CaSR T732A), other in the first intracellular loop (CasSR N639K) and two in the carboxyl-terminal intracellular region (CaSR R886Q and CaSR V894I). The functional consequences of these single amino acid changes are currently unknown but some possibilities might be speculated based on the recent structural analysis of dimeric CaSR which, upon agonist binding, forms a compact dimer that engages the intracellular regions (Ling et al. 2021; Wen et al. 2021). In the structure of CaSR, the intracellular domains appeared as disorganized regions (Ling et al. 2021; Wen et al. 2021), indicating its potential dynamism. Hypothetically, point mutations within these regions might have an impact on their conformational organization and their interactions with signaling transducers and effectors, affecting the signaling capacities of mutant receptors. To assess this possibility, we studied the effect of wild type and mutant CaSR on the Rac GTPase and ERK signaling pathways, known to be involved in cell migration and proliferation, and investigated how wild type CaSR activates Rac and promotes cell migration. We found that mutant CaSR receptors differed in the magnitude of their effect on Rac but were as effective as the wild type CaSR to activate ERK. CaSR stimulated ERK via Gi, as indicated by the inhibitory effect of PTX, which also prevented ERK activation by the four mutant CaSR (Supplementary Fig. 4). This pathway was not sensitive to PKI (a competitive PKA inhibitor), indicating that in our system CaSR was not coupled to Gs (Supplementary Fig. 4F), as it has been suggested in some cancer cells (Mamillapalli et al. 2008). Regarding Rac, we characterized that this small GTP-binding protein is activated by CaSR via the mTORC2 pathway and found that endogenous CaSR activates this pathway to guide MDA-MB-231 cells to migrate. Specifically, we characterized mTORC2 as a signaling effector of CaSR required to activate Rac and promote cell migration.
Knowing that Rac, a master regulator of the actin cytoskeleton at the leading edge of migrating cells, can be activated via the PI3K/AKT/mTORC2 signaling pathway (Hanna and El-Sibai, 2013; Lyda et al. 2019; Vazquez-Prado et al. 2016), we analyzed whether this pathway mediates the activation of Rac by wild type CaSR and CaSR mutants. CaSR mutants differed in the magnitude of their effects on Rac. CaSR N639K was the most effective activator of Rac, followed by CaSR T732A, which was as effective as wild type CaSR, whereas agonist-stimulated CaSR R886Q was unable to activate Rac, and CaSR V894I promoted constitutive Rac activation. However, because these mutants, as well as the wild type receptor, were similarly effective in promoting the phosphorylation of ERK and S6, these results indicate that CaSR mutants acquire differential properties to stimulate the mTORC2/Rac pathway. CaSR uses Gβγ as the main transducer to activate this pathway, as indicated by the inhibitory effect of Gallein. The Gβγ heterodimers implicated in this pathway are likely released from Gi, as shown by the inhibitory effect of PTX. In breast cancer patients, the signaling repertoire of the PI3K/mTOR pathway is well expressed and some of its components exhibit a positive correlation with CASR, suggesting that CaSR might activate this pathway within the tumor microenvironment (Supplementary Fig. 5).
Wild type and mutant CaSR receptors activate mTORC1 and mTORC2, as indicated by the phosphorylation of S6 and AKT, bona fide readouts of these pathways (Arvisais et al. 2006; Dada et al. 2008; Hou and Klann, 2004; Huang and Fingar, 2014; Zhang et al. 2007). Additionally, S6 phosphorylation was inhibited by acute incubation with rapamycin, which under these conditions specifically inhibits mTORC1 (Bracho-Valdes et al. 2011; Liu and Sabatini, 2020). CaSR proliferative pathways are elicited via the transactivation of EGFR, however mTORC1 pathway does not involve EGFR transactivation because AG1478 only inhibited EGF signaling but not signaling elicited by CaSR (El Hiani et al. 2009; Yano et al. 2004). In addition, CaSR promoted the phosphorylation of mTOR at Ser2448 (p-mTOR, Supplementary Fig. 3C), a post-translational modification that fine-tunes the regulatory loop by S6K (Arvisais et al. 2006; Reynolds et al. 2002). Regarding mTORC2 activation by CaSR, our findings extend the previously demonstrated role of mTORC2 as an effector of CaSR, promoting osteoblast differentiation and survival (Rybchyn et al. 2019). This pathway appears to also be relevant in other cancer cells, such as gastric cancer cells, in which NPS-2143 inhibits AKT and mTOR phosphorylation (Zong-Lin Zhang, 2020). The identification of mTORC2 as an effector in CaSR-dependent cell migration was confirmed in Rictor-knockdown cells, which exhibited reduced activation of Rac and cell migration in the absence of mTORC2, a complex that integrates Rictor as an essential component (Oh and Jacinto, 2011; Sarbassov et al. 2006; Xu et al. 2014). Furthermore, our findings showing that CaSR activates Rac via mTOR indicate the potential involvement of a RacGEF as an effector of mTOR, acting downstream of CaSR. A potential candidate for participation in this pathway is P-Rex1, a RacGEF that directly interacts with mTOR and which has been proposed as an effector of mTORC2 (Hernandez-Negrete et al. 2007). Interestingly, this GEF is a direct effector of Gβγ (Welch et al. 2002), which also interacts with mTOR (Robles-Molina et al. 2014). Altogether, our results indicate that CaSR promotes breast cancer cell migration via the Gβγ/PI3K/AKT/mTOR pathway (Fig. 5E).
Conclusion
CaSR mutants identified in breast cancer patients exhibit differential abilities to activate Rac but were similarly effective to activate ERK, indicating that some of these mutants display some biased signaling. In MDA-MB-231 cells, endogenously expressed CaSR promotes cell migration via a Gβγ/PI3K/AKT/mTOR /Rac signaling pathway.
References
Aguirre A, Gonzalez A, Planell JA, Engel E (2010) Extracellular calcium modulates in vitro bone marrow-derived Flk-1+ CD34+ progenitor cell chemotaxis and differentiation through a calcium-sensing receptor. Biochem Biophys Res Commun 393(1):156–161
Arvisais EW, Romanelli A, Hou X, Davis JS (2006) AKT-independent phosphorylation of TSC2 and activation of mTOR and ribosomal protein S6 kinase signaling by prostaglandin F2alpha. J Biol Chem 281(37):26904–26913
Bai M, Quinn S, Trivedi S, Kifor O, Pearce SH, Pollak MR, Krapcho K, Hebert SC, Brown EM (1996) Expression and characterization of inactivating and activating mutations in the human Ca2+o-sensing receptor. J Biol Chem 271(32):19537–19545
Bai M, Trivedi S, Kifor O, Quinn SJ, Brown EM (1999) Intermolecular interactions between dimeric calcium-sensing receptor monomers are important for its normal function. Proc Natl Acad Sci U S A 96(6):2834–2839
Bhagavathula N, Kelley EA, Reddy M, Nerusu KC, Leonard C, Fay K, Chakrabarty S, Varani J (2005) Upregulation of calcium-sensing receptor and mitogen-activated protein kinase signalling in the regulation of growth and differentiation in colon carcinoma. Br J Cancer 93(12):1364–1371
Bhaskar PT, Hay N (2007) The two TORCs and Akt. Dev Cell 12(4):487–502
Boudot C, Henaut L, Thiem U, Geraci S, Galante M, Saldanha P, Saidak Z, Six I, Clezardin P, Kamel S, Mentaverri R (2017) Overexpression of a functional calcium-sensing receptor dramatically increases osteolytic potential of MDA-MB-231 cells in a mouse model of bone metastasis through epiregulin-mediated osteoprotegerin downregulation. Oncotarget 8(34):56460–56472
Bracho-Valdes I, Moreno-Alvarez P, Valencia-Martinez I, Robles-Molina E, Chavez-Vargas L, Vazquez-Prado J (2011) mTORC1- and mTORC2-interacting proteins keep their multifunctional partners focused. IUBMB Life 63(10):896–914
Brown EM, MacLeod RJ (2001) Extracellular calcium sensing and extracellular calcium signaling. Physiol Rev 81(1):239–297
Carretero-Ortega J, Walsh CT, Hernandez-Garcia R, Reyes-Cruz G, Brown JH, Vazquez-Prado J (2010) Phosphatidylinositol 3,4,5-triphosphate-dependent Rac exchanger 1 (P-Rex-1), a guanine nucleotide exchange factor for Rac, mediates angiogenic responses to stromal cell-derived factor-1/chemokine stromal cell derived factor-1 (SDF-1/CXCL-12) linked to Rac activation, endothelial cell migration, and in vitro angiogenesis. Mol Pharmacol 77(3):435–442
Casey LM, Pistner AR, Belmonte SL, Migdalovich D, Stolpnik O, Nwakanma FE, Vorobiof G, Dunaevsky O, Matavel A, Lopes CM, Smrcka AV, Blaxall BC (2010) Small molecule disruption of G beta gamma signaling inhibits the progression of heart failure. Circ Res 107(4):532–539
Cervantes-Villagrana RD, Adame-Garcia SR, Garcia-Jimenez I, Color-Aparicio VM, Beltran-Navarro YM, Konig GM, Kostenis E, Reyes-Cruz G, Gutkind JS, Vazquez-Prado J (2019) Gbetagamma signaling to the chemotactic effector P-REX1 and mammalian cell migration is directly regulated by Galphaq and Galpha13 proteins. J Biol Chem 294(2):531–546
Cervantes-Villagrana RD, Beltran-Navarro YM, Garcia-Jimenez I, Adame-Garcia SR, Olguin-Olguin A, Reyes-Cruz G, Vazquez-Prado J (2021) Gbetagamma recruits and activates P-Rex1 via two independent binding interfaces. Biochem Biophys Res Commun 539:20–27
Dada S, Demartines N, Dormond O (2008) mTORC2 regulates PGE2-mediated endothelial cell survival and migration. Biochem Biophys Res Commun 372(4):875–879
Das S, Clezardin P, Kamel S, Brazier M, Mentaverri R (2020) The CaSR in pathogenesis of breast cancer: a new target for early stage bone metastases. Front Oncol 10:69
Davey AE, Leach K, Valant C, Conigrave AD, Sexton PM, Christopoulos A (2012) Positive and negative allosteric modulators promote biased signaling at the calcium-sensing receptor. Endocrinology 153(3):1232–1241
El Hiani Y, Lehen’kyi V, Ouadid-Ahidouch H, Ahidouch A (2009) Activation of the calcium-sensing receptor by high calcium induced breast cancer cell proliferation and TRPC1 cation channel over-expression potentially through EGFR pathways. Arch Biochem Biophys 486(1):58–63
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C, Schultz N (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6(269):pl1
Hanna S, El-Sibai M (2013) Signaling networks of Rho GTPases in cell motility. Cell Signal 25(10):1955–1961
Hauache OM, Hu J, Ray K, Xie R, Jacobson KA, Spiegel AM (2000) Effects of a calcimimetic compound and naturally activating mutations on the human Ca2+ receptor and on Ca2+ receptor/metabotropic glutamate chimeric receptors. Endocrinology 141(11):4156–4163
Hernandez-Bedolla MA, Carretero-Ortega J, Valadez-Sanchez M, Vazquez-Prado J, Reyes-Cruz G (2015) Chemotactic and proangiogenic role of calcium sensing receptor is linked to secretion of multiple cytokines and growth factors in breast cancer MDA-MB-231 cells. Biochem Biophys Acta 1853(1):166–182
Hernandez-Negrete I, Carretero-Ortega J, Rosenfeldt H, Hernandez-Garcia R, Calderon-Salinas JV, Reyes-Cruz G, Gutkind JS, Vazquez-Prado J (2007) P-Rex1 links mammalian target of rapamycin signaling to Rac activation and cell migration. J Biol Chem 282(32):23708–23715
Hou L, Klann E (2004) Activation of the phosphoinositide 3-kinase-Akt-mammalian target of rapamycin signaling pathway is required for metabotropic glutamate receptor-dependent long-term depression. J Neurosci 24(28):6352–6361
Houslay DM, Anderson KE, Chessa T, Kulkarni S, Fritsch R, Downward J, Backer JM, Stephens LR, Hawkins PT (2016) Coincident signals from GPCRs and receptor tyrosine kinases are uniquely transduced by PI3Kbeta in myeloid cells. Sci Signal 9(441):ra82
Huang K, Fingar DC (2014) Growing knowledge of the mTOR signaling network. Semin Cell Dev Biol 36:79–90
Iamartino L, Elajnaf T, Gall K, David J, Manhardt T, Heffeter P, Grusch M, Derdak S, Baumgartner-Parzer S (1867) Schepelmann M and Kallay E (2020) Effects of pharmacological calcimimetics on colorectal cancer cells over-expressing the human calcium-sensing receptor. Biochimica Et Biophysica Acta Molecular Cell Res 12:118836
Jacinto E, Loewith R, Schmidt A, Lin S, Ruegg MA, Hall A, Hall MN (2004) Mammalian TOR complex 2 controls the actin cytoskeleton and is rapamycin insensitive. Nat Cell Biol 6(11):1122–1128
Joeckel E, Haber T, Prawitt D, Junker K, Hampel C, Thuroff JW, Roos FC, Brenner W (2014) High calcium concentration in bones promotes bone metastasis in renal cell carcinomas expressing calcium-sensing receptor. Mol Cancer 13:42
Kim W, Takyar FM, Swan K, Jeong J, VanHouten J, Sullivan C, Dann P, Yu H, Fiaschi-Taesch N, Chang W, Wysolmerski J (2016) Calcium-sensing receptor promotes breast cancer by stimulating intracrine actions of parathyroid hormone-related protein. Can Res 76(18):5348–5360
Liang CC, Park AY, Guan JL (2007) In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc 2(2):329–333
Liao J, Schneider A, Datta NS, McCauley LK (2006a) Extracellular calcium as a candidate mediator of prostate cancer skeletal metastasis. Cancer Res 66(18):9065–9073
Liao J, Schneider A, Datta NS, McCauley LK (2006b) Extracellular calcium as a candidate mediator of prostate cancer skeletal metastasis. Can Res 66(18):9065–9073
Lienhardt A, Garabedian M, Bai M, Sinding C, Zhang Z, Lagarde JP, Boulesteix J, Rigaud M, Brown EM, Kottler ML (2000) A large homozygous or heterozygous in-frame deletion within the calcium-sensing receptor’s carboxylterminal cytoplasmic tail that causes autosomal dominant hypocalcemia. J Clin Endocrinol Metab 85(4):1695–1702
Ling S, Shi P, Liu S, Meng X, Zhou Y, Sun W, Chang S, Zhang X, Zhang L, Shi C, Sun D, Liu L, Tian C (2021) Structural mechanism of cooperative activation of the human calcium-sensing receptor by Ca(2+) ions and L-tryptophan. Cell Res 31(4):383–394
Liu GY, Sabatini DM (2020) mTOR at the nexus of nutrition, growth, ageing and disease. Nat Rev Mol Cell Biol 21(4):183–203
Lyda JK, Tan ZL, Rajah A, Momi A, Mackay L, Brown CM, Khadra A (2019) Rac activation is key to cell motility and directionality: An experimental and modelling investigation. Comput Struct Biotechnol J 17:1436–1452
MacLeod RJ, Yano S, Chattopadhyay N, Brown EM (2004) Extracellular calcium-sensing receptor transactivates the epidermal growth factor receptor by a triple-membrane-spanning signaling mechanism. Biochem Biophys Res Commun 320(2):455–460
Mamillapalli R, VanHouten J, Zawalich W, Wysolmerski J (2008) Switching of G-protein usage by the calcium-sensing receptor reverses its effect on parathyroid hormone-related protein secretion in normal versus malignant breast cells. J Biol Chem 283(36):24435–24447
Mayr B, Glaudo M, Schofl C (2016) Activating calcium-sensing receptor mutations: prospects for future treatment with calcilytics. Trends Endocrinol Metab 27(9):643–652
Mihai R, Stevens J, McKinney C, Ibrahim NB (2006) Expression of the calcium receptor in human breast cancer–a potential new marker predicting the risk of bone metastases. Eur J Surg Oncol 32(5):511–515
Nemeth EF, Delmar EG, Heaton WL, Miller MA, Lambert LD, Conklin RL et al (2001) Calcilytic compounds: potent and selective Ca2+ receptor antagonists that stimulate secretion of parathyroid hormone. J Pharm Exp Ther 299(1):323–331
Oh WJ, Jacinto E (2011) mTOR complex 2 signaling and functions. Cell Cycle 10(14):2305–2316
O’Hayre M, Vazquez-Prado J, Kufareva I, Stawiski EW, Handel TM, Seshagiri S, Gutkind JS (2013) The emerging mutational landscape of G proteins and G-protein-coupled receptors in cancer. Nat Rev Cancer 13(6):412–424
Olszak IT, Poznansky MC, Evans RH, Olson D, Kos C, Pollak MR, Brown EM, Scadden DT (2000) Extracellular calcium elicits a chemokinetic response from monocytes in vitro and in vivo. J Clin Invest 105(9):1299–1305
Pollak MR, Brown EM, Chou YH, Hebert SC, Marx SJ, Steinmann B, Levi T, Seidman CE, Seidman JG (1993) Mutations in the human Ca(2+)-sensing receptor gene cause familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. Cell 75(7):1297–1303
Reyes-Cruz G, Hu J, Goldsmith PK, Steinbach PJ, Spiegel AM (2001) Human Ca(2+) receptor extracellular domain Analysis of function of lobe I loop deletion mutants. J Biol Chem 276(34):32145–32151
Reynolds TH, Bodine SC, Lawrence JC (2002) Control of Ser2448 phosphorylation in the mammalian target of rapamycin by insulin and skeletal muscle load. J Biol Chem 277(20):17657–17662
Riccardi D, Valenti G (2016) Localization and function of the renal calcium-sensing receptor. Nat Rev Nephrol 12(7):414–425
Robles-Molina E, Dionisio-Vicuna M, Guzman-Hernandez ML, Reyes-Cruz G, Vazquez-Prado J (2014) Gbetagamma interacts with mTOR and promotes its activation. Biochem Biophys Res Commun 444(2):218–223
Rybchyn MS, Islam KS, Brennan-Speranza TC, Cheng Z, Brennan SC, Chang W, Mason RS, Conigrave AD (2019) Homer1 mediates CaSR-dependent activation of mTOR complex 2 and initiates a novel pathway for AKT-dependent beta-catenin stabilization in osteoblasts. J Biol Chem 294(44):16337–16350
Saidak Z, Boudot C, Abdoune R, Petit L, Brazier M, Mentaverri R, Kamel S (2009) Extracellular calcium promotes the migration of breast cancer cells through the activation of the calcium sensing receptor. Exp Cell Res 315(12):2072–2080
Sanders JL, Chattopadhyay N, Kifor O, Yamaguchi T, Butters RR, Brown EM (2000) Extracellular calcium-sensing receptor expression and its potential role in regulating parathyroid hormone-related peptide secretion in human breast cancer cell lines. Endocrinology 141(12):4357–4364
Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM (2004) Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol 14(14):1296–1302
Sarbassov DD, Guertin DA, Ali SM, Sabatini DM (2005) Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science 307(5712):1098–1101
Sarbassov DD, Ali SM, Sengupta S, Sheen JH, Hsu PP, Bagley AF, Markhard AL, Sabatini DM (2006) Prolonged rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol Cell 22(2):159–168
Saxton RA, Sabatini DM (2017) mTOR Signaling in growth, metabolism, and disease. Cell 169(2):361–371
Stephens LR, Eguinoa A, Erdjument-Bromage H, Lui M, Cooke F, Coadwell J, Smrcka AS, Thelen M, Cadwallader K, Tempst P, Hawkins PT (1997) The G beta gamma sensitivity of a PI3K is dependent upon a tightly associated adaptor, p101. Cell 89(1):105–114
Tang X, Sun Z, Runne C, Madsen J, Domann F, Henry M, Lin F, Chen S (2011) A critical role of Gbetagamma in tumorigenesis and metastasis of breast cancer. J Biol Chem 286(15):13244–13254
Tate JG, Bamford S, Jubb HC, Sondka Z, Beare DM, Bindal N, Boutselakis H, Cole CG, Creatore C, Dawson E, Fish P, Harsha B, Hathaway C, Jupe SC, Kok CY, Noble K, Ponting L, Ramshaw CC, Rye CE, Speedy HE, Stefancsik R, Thompson SL, Wang S, Ward S, Campbell PJ, Forbes SA (2019) COSMIC: the Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res 47(D1):D941–D947
Tennakoon S, Aggarwal A and Kallay E (2015) The calcium-sensing receptor and the hallmarks of cancer. Biochimica et biophysica acta 2015.
Tfelt-Hansen J, Yano S, John Macleod R, Smajilovic S, Chattopadhyay N, Brown EM (2005) High calcium activates the EGF receptor potentially through the calcium-sensing receptor in Leydig cancer cells. Growth Factors 23(2):117–123
Tomlins SA, Bolllinger N, Creim J, Rodland KD (2005) Cross-talk between the calcium-sensing receptor and the epidermal growth factor receptor in Rat-1 fibroblasts. Exp Cell Res 308(2):439–445
Vazquez-Prado J, Bracho-Valdes I, Cervantes-Villagrana RD, Reyes-Cruz G (2016) Gbetagamma Pathways in Cell Polarity and Migration Linked to Oncogenic GPCR Signaling: Potential Relevance in Tumor Microenvironment. Mol Pharmacol 90(5):573–586
Welch HC, Coadwell WJ, Ellson CD, Ferguson GJ, Andrews SR, Erdjument-Bromage H, Tempst P, Hawkins PT, Stephens LR (2002) P-Rex1, a PtdIns(3,4,5)P3- and Gbetagamma-regulated guanine-nucleotide exchange factor for Rac. Cell 108(6):809–821
Wen T, Wang Z, Chen X, Ren Y, Lu X, Xing Y, Lu J, Chang S, Zhang X, Shen Y, Yang X (2021) Structural basis for activation and allosteric modulation of full-length calcium-sensing receptor. Sci Adv 7(23):eabg1483
Wullschleger S, Loewith R, Hall MN (2006) TOR signaling in growth and metabolism. Cell 124(3):471–484
Xu K, Liu P, Wei W (2014) mTOR signaling in tumorigenesis. Biochem Biophys Acta 1846(2):638–654
Yamaguchi T, Chattopadhyay N, Kifor O, Butters RR Jr, Sugimoto T, Brown EM (1998a) Mouse osteoblastic cell line (MC3T3-E1) expresses extracellular calcium (Ca2+o)-sensing receptor and its agonists stimulate chemotaxis and proliferation of MC3T3-E1 cells. J Bone Miner Res 13(10):1530–1538
Yamaguchi T, Kifor O, Chattopadhyay N, Bai M, Brown EM (1998b) Extracellular calcium (Ca2+o)-sensing receptor in a mouse monocyte-macrophage cell line (J774): potential mediator of the actions of Ca2+o on the function of J774 cells. J Bone Miner Res 13(9):1390–1397
Yano SMR, Chattopadhyay N, Tfelt-Hansen J, Kifor O, Butters RR, Brown EM (2004) Calcium-sensing receptor activation stimulates parathyroid hormone-related protein secretion in prostate cancer cells: role of epidermal growth factor receptor transactivation. Bone 35(3):664–672
Zavala-Barrera C, Del-Rio-Robles JE, Garcia-Jimenez I, Egusquiza-Alvarez CA, Hernandez-Maldonado JP, Vazquez-Prado J, Reyes-Cruz G (2021) The calcium sensing receptor (CaSR) promotes Rab27B expression and activity to control secretion in breast cancer cells. Biochim Biophys Acta Mol Cell Res 1868(7):119026
Zhang H, Bajraszewski N, Wu E, Wang H, Moseman AP, Dabora SL, Griffin JD, Kwiatkowski DJ (2007) PDGFRs are critical for PI3K/Akt activation and negatively regulated by mTOR. J Clin Invest 117(3):730–738
Zong-Lin Zhang Z-RL, Li J-S, Wang S-R (2020) Calcium-sensing receptor antagonist NPS-2143 suppresses proliferation and invasion of gastric cancer cells. Cancer Gene Ther 27(7–8):548–557
Acknowledgements
We acknowledge the technical assistance provided by Estanislao Escobar-Islas, Jaime Estrada-Trejo, Israel Valencia-Martínez and David Pérez. The authors express their gratitude to Maggie Brunner, MA, for editorial/style corrections. The authors declare no conflict of interest. This work was supported by grants from CONACyT (240119 and CF-2019-1794 to G.R.C.) and (286274 to J.V.P.), Fondo Sep-CINVESTAV (FidSC2018/3 to G.R.C.). L.B. O-C, J.E. del-R-R, I. G-J, C. Z-B, Y.M. B-N, J. J. H-M, I. R-R, M.A, H-B; and A.P. R-I are and were graduate students supported by CONACyT fellowships. The authors declare that there are no competing interests associated with the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: L.B. O-C; J.E. del-R-R; I. R-R; J.V.P., and G.R.C. Supervised the study: G.R.C. Performed the experiments: L.B. O-C; J.E. del-R-R; C. Z-B; I. G-J; I. R-R; M.A. H-B; A.P. R-I, J. J.H-M, and M.V-S. Performed data mining: Y.M. B-N. Analyzed the data: L.B. O-C; J.E. del-R-R; C. Z-B; I.G-J; I.R-R, and M.A.H-B. Wrote the paper: L.B. O-C; J.V.P. and G.R.C. All authors reviewed and approved the final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Orduña-Castillo, L.B., del-Río-Robles, J.E., García-Jiménez, I. et al. Calcium sensing receptor stimulates breast cancer cell migration via the Gβγ-AKT-mTORC2 signaling pathway. J. Cell Commun. Signal. 16, 239–252 (2022). https://doi.org/10.1007/s12079-021-00662-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12079-021-00662-y