Abstract
Background
Immune checkpoint inhibitor (ICI)-based treatments have become the mainstay of first-line treatment for unresectable hepatocellular carcinoma (HCC), but there has been a concern that intrahepatic HCC lesions may be less responsive to ICI monotherapy. We aimed to investigate the organ-specific response patterns among unresectable HCC patients treated with first-line atezolizumab-bevacizumab or lenvatinib.
Methods
This retrospective study included 386 patients with Child–Pugh A unresectable HCC who were treated with first-line atezolizumab-bevacizumab (n = 217) or lenvatinib (n = 169). The organ-specific response was separately evaluated according to the site of the lesions: liver, lung, lymph node (LN), and intraabdomen based on a radiological evaluation adopted from RECIST v 1.1.
Results
The median age was 60 years. Hepatitis B infection was the most common etiology (n = 270, 69.9%), and 291 (75.4%) patients had a viral etiology. The proportion of patients achieving a ≥ 30% reduction in the tumor burden for each organ category was overall higher in the atezolizumab-bevacizumab group than that in the lenvatinib group: 20.2% vs. 11.8%, 23.0% vs. 12.2%, 27.9% vs. 17.9% and 33.3% vs. 15.0% for intrahepatic, lung, LN, and intraabdominal lesions, respectively. The corresponding values for the subgroup with a viral etiology were 17.3% vs. 8.1%, 18.8% vs. 13.3%, 28.9% vs. 3.6%, and 36.0% vs. 12.5%, respectively.
Conclusion
Compared to lenvatinib, atezolizumab-bevacizumab was associated with a favorable organ-specific response regardless of the site of the tumor lesions. Unlike anti-PD-1 monotherapy, atezolizumab-bevacizumab had a comparable organ-specific response between intrahepatic and extrahepatic lesions, especially for those with viral etiology HCCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the second leading cause of cancer-related deaths worldwide [1]. The increasing incidence and poor prognosis of HCC create a substantial socioeconomic burden, making HCC an important global health issue [2].
Based on the phase 3 IMBrave 150 [3] and HIMALAYA [4] studies, immune checkpoint inhibitor (ICI)-based combination regimens are now the standard first-line treatment for patients with unresectable HCC. Recently, rivoceranib, a VEGFR2-targeted multikinase inhibitor (MKI), combined with camrelizumab, an anti-PD-1 antibody [5], demonstrated an overall survival (OS) benefit over sorafenib as first-line therapy in a phase 3 trial.
Recently, the impact of differences in organ-specific immune microenvironments on the efficacy of ICI-based treatments has been increasingly recognized. For example, the difference in the abundance of dendritic cells between the lung and pancreas microenvironments was shown to drive divergent T-cell responses [6]. The liver, the primary site for HCC, is an immune tolerogenic organ of gut-derived microbial metabolites, required for its role in the maintenance of global homeostasis, which could potentially lead to decreased efficacy of ICIs for tumors in the liver [7]. Among the various immune subsets, hepatic myeloid cells are one of the important immune subsets limiting the efficacy of ICIs against tumors in the liver [8].
Different impacts of the site of HCC lesions have been reported for HCC patients treated with ICI monotherapy. In a previous study by Lu et al., it was suggested that intrahepatic HCC lesions may be less responsive to ICIs than extrahepatic lesions, with lung metastases most likely to respond to ICI [9]. Another retrospective analysis also found that intrahepatic HCC lesions were less responsive to nivolumab than lung or lymph node (LN) lesions [10]. However, given the absence of a control arm treated without ICI and heterogeneous ICI regimens and treatment lines, these findings need to be validated. Moreover, given that atezolizumab-bevacizumab is currently the most widely used first-line standard regimen, these findings will need to be reappraised in the setting of ICI plus anti-VEGF combination therapy.
In this study, we aimed to investigate the organ-specific response patterns among unresectable HCC patients treated with first-line atezolizumab-bevacizumab or lenvatinib. We also focused on the impact of the etiology of HCC on the organ-specific response for each treatment.
Materials and methods
Study patients
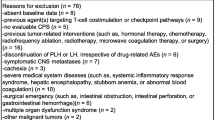
This retrospective analysis included patients with unresectable HCC who were diagnosed using a pathologic or noninvasive assessment according to the American Association for the Study of Liver Diseases criteria. Patients treated with atezolizumab-bevacizumab or lenvatinib as first-line treatment between October 2013 and October 2022 were included if patients had at least one measurable lesion according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. A total of 386 patients with unresectable HCC who were treated with first-line atezolizumab-bevacizumab (n = 217) or lenvatinib (n = 169) were included as the study population. Clinical data regarding baseline patient characteristics, including Eastern Cooperative Oncology Group (ECOG) performance status, albumin-bilirubin (ALBI) grade, Barcelona Clinic Liver Cancer (BCLC) stage, laboratory data, locoregional treatment history, and survival outcomes, were retrospectively obtained by reviewing medical records. This study was approved by the Institutional Review Board of Asan Medical Center (IRB No. 2021-0064) and was performed in accordance with the ethical standards of the Institutional Research Committee and the latest Declaration of Helsinki.
Treatment and follow-up
Atezolizumab-bevacizumab was administered every 3 weeks with 1200 mg of atezolizumab plus 15 mg/kg of bevacizumab intravenously. Lenvatinib was given orally once daily as monotherapy 12 mg QD (weight ≥ 60 kg) or 8 mg QD (weight < 60 kg). The doses were reduced or interrupted in accordance with the protocol of the IMBrave150 [3] and REFLECT [11] trials, respectively.
Overall tumor response evaluation was performed every 6–8 weeks by assessing radiological measures such as contrast-enhanced dynamic computed tomography or magnetic resonance imaging scans. Imaging studies were performed whenever clinically indicated due to a suspicion of tumor progression. RECIST version 1.1 was used for grading the overall tumor responses and making decisions about patient management [12].
Organ-specific response evaluation
The organ-specific response was separately evaluated according to the following categories: intrahepatic lesions, lung lesions, LN lesions, and intraabdominal lesions, including peritoneal, adrenal, splenic, and subphrenic metastases, as previously described [9]. Organ-specific response evaluation was performed for each organ system based on a size method that was modified from RECIST v1.1: for the non-LN lesions, measurable lesions in each organ with a longest diameter ≥ 10 mm and LN lesions with a short-axis diameter ≥ 15 mm were selected. Up to two lesions were chosen as target lesions in each organ for the organ-specific response evaluation. For intrahepatic lesions, an enhancement method based on the modified RECIST for intrahepatic lesions was additionally adopted for evaluating the liver lesion-specific response.
As most bone lesions are not measurable in the absence of a soft tissue component meeting the requirement for measurability according to RECIST v1.1 [12], bone-specific responses were not evaluated, and instead, PFS and OS were analyzed among patients with bone metastasis.
Statistical analysis
Progression-free survival (PFS) was defined as the time from the initiation of atezolizumab-bevacizumab or lenvatinib (index date) to the date of disease progression determined by RECIST v1.1 criteria or death, whichever came first. OS was defined as the time interval between the index date and the date of death from any cause. The Kaplan–Meier method was used to estimate survival outcomes, and the log-rank test was used to compare survival outcomes among the subgroups. The Chi-square test or Fisher’s exact test was used to compare categorical variables among the subgroups. A p-value of < 0.05 was considered statistically significant. Statistical analyses were performed using R (version 4.2.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
The baseline characteristics of the study patients are summarized in Table 1. Patients in the atezolizumab-bevacizumab group were slightly older than those in the lenvatinib group (median 62 years vs. 58 years). A majority of study patients were male in both groups (83.4% and 85.8% in the atezolizumab-bevacizumab and lenvatinib groups, respectively). There were no significant differences between the two groups in terms of ECOG performance status, BCLC stage, and ALBI grade. The etiology of HCC was similar between the two groups: hepatitis B virus infection was the most frequent etiology (73.3% and 65.7% in the atezolizumab-bevacizumab and lenvatinib groups, respectively) in both groups, while 21.2% and 29.0% of patients had non-viral etiology HCC, respectively. Extrahepatic spread was identified in 76.0% and 74.6% in the atezolizumab-bevacizumab and lenvatinib groups, respectively: lung, LN, and intraabdominal metastases were present in 39.6% vs. 39.1%, 30.0% vs. 33.1%, and 16.6% vs. 15.4% of patients, respectively. The profiles of previous locoregional treatments were similar between the two groups.
Overall efficacy outcomes
The median duration of follow-up was 11.1 months (interquartile range [IQR] 8.9–22.4) for the atezolizumab plus bevacizumab group and 16.1 months (IQR 10.3–28.4) for the lenvatinib group. The objective response rate (ORR) according to RECIST v1.1 tended to be higher in the atezolizumab-bevacizumab group (21.2%) than that in the lenvatinib group (14.8%) (p = 0.139) (Table 2). In the atezolizumab-bevacizumab and lenvatinib groups, the median PFS was 6.8 months (95% confidence interval [CI]: 5.5–7.6) and 6.3 months (95% CI: 5.4–8.0), respectively (p = 0.501), and the median OS was 18.9 months (95% CI: 17.2–26.6) and 14.1 months (95% CI: 12.8–25.6), respectively (p = 0.250) (Fig. 1). The proportion of death events associated with disease progression was 89.2% and 83.1% in the atezolizumab-bevacizumab and lenvatinib groups, respectively.
Organ-specific response
With atezolizumab-bevacizumab, 20.2%, 23.0%, 27.9%, and 33.3% of patients achieved a ≥ 30% reduction in the sum of the tumor diameter for intrahepatic (based on the size method), lung, LN, and intraabdominal lesions, respectively (Table 3 and Fig. 2). The proportion of patients achieving a ≥ 30% reduction in the tumor burden was overall higher in the atezolizumab-bevacizumab group than that in the lenvatinib group (Table 3 and Fig. 2): 20.2% vs. 11.8% (p = 0.170), 23.0% vs. 12.2% (p = 0.268), 27.9% vs. 17.9% (p = 0.421), and 33.3% vs. 15.0% (p = 0.263) for intrahepatic (based on the sized method), lung, LN, and intraabdominal lesions, respectively. This difference in the proportion of patients achieving a ≥ 30% reduction in the tumor burden was more prominent when assessed based on the enhancement method (36.0% vs. 18.7%, p = 0.028 for atezolizumab-bevacizumab vs. lenvatinib, respectively; Table 3 and Fig. 2). Among patients who were feasible for an organ-specific response evaluation for both intrahepatic and extrahepatic lesions (n = 84), there was no patient who showed discordance between the tumor response in intrahepatic and extrahepatic lesions; when any of the extrahepatic organs showed a tumor response, there was no case in which the intrahepatic lesions did not achieve a tumor response. Among patients with bone metastasis, PFS and OS were comparable between the two groups (Supplementary Fig. 1).
The proportions of patients achieving ≥ 50% and ≥ 80% reductions in the tumor burden were consistently higher with atezolizumab-bevacizumab than that with lenvatinib for intrahepatic lesions assessed based on the enhancement method (21.3% vs. 12.0% and 14.7% vs. 9.3, respectively for ≥ 50% and ≥ 80% reduction) and for lung (18.0% vs. 4.9% and 8.2% vs. 4.9%, respectively), LN (18.6% vs. 7.7% and 9.3% vs. 5.1%, respectively), and intraabdominal lesions (20.0% vs. 10.0% and 10.0% vs. 5.0%, respectively), but this was not the case for intrahepatic lesions assessed based on the size method (5.5% vs. 7.1% and 3.7% vs. 7.1%, respectively; Table 3 and Fig. 2).
Organ-specific response according to the etiology of HCC
The baseline characteristics for patients with a viral and non-viral etiology are summarized in Supplementary Table 2. While most characteristics were comparable between the two groups, patients in the viral etiology group were older and had higher alpha-fetoprotein (AFP) levels than those in the non-viral etiology group. When PFS and OS were analyzed according to the etiology of HCC, there was a trend toward favorable survival outcomes for atezolizumab-bevacizumab for HCCs with a viral etiology (HR: 0.81, 95% CI: 0.61–1.06, p = 0.129 and HR: 0.67, 95% CI: 0.47–0.96, p = 0.028 for PFS and OS, respectively), whereas lenvatinib showed a tendency for favorable outcomes for HCCs with a non-viral etiology (HR: 0.79, 95% CI: 0.49–1.28, p = 0.341 and HR: 0.79, 95% CI: 0.40–1.59, p = 0.516 for PFS and OS, respectively) (Fig. 3 and Supplemental Fig. 2).
For patients with a viral etiology HCC, the results were similar to those of the overall study population, with a consistently favorable organ-specific response with atezolizumab-bevacizumab (Table 4 and Supplemental Fig. 3): the proportions of patients achieving a ≥ 30% reduction in the tumor burden for intrahepatic, lung, LN, and intraabdominal lesions were consistently higher in the atezolizumab-bevacizumab group than those in the lenvatinib group: 17.3% vs. 8.1%, 18.8% vs. 13.3%, 28.9% vs. 3.6%, and 36.0% vs. 12.5%, respectively.
With regard to patients with non-viral etiology HCCs, atezolizumab-bevacizumab was not associated with a better organ-specific response for LNs compared to lenvatinib (20.0% vs. 54.5%; p = 0.308, respectively, for achieving a ≥ 30% tumor burden reduction) and intraabdominal lesions (20.0% vs. 25.0%; p > 0.999), respectively, for achieving a ≥ 30% tumor burden reduction. In addition, none of the patients (0 out of 28 patients) who achieved a ≥ 50% or a ≥ 80% reduction in the tumor burden as assessed with the size method adopted from RECIST v1.1 were treated with atezolizumab-bevacizumab for intrahepatic lesions (Table 4 and Supplemental Fig. 4).
Association between organ-specific response and survival outcomes
To assess the prognostic impact of a tumor response in each organ on the survival outcomes, we performed a pooled analysis combining the atezolizumab-bevacizumab and lenvatinib groups. In this analysis, tumor responders in each organ were significantly associated with better PFS and OS compared to non-tumor responders (p < 0.05 for all; Supplementary Fig. 5).
Safety profile
Profiles of the adverse events are summarized in Supplementary Table 1. The most common adverse events, regardless of the relationship with agents, in the atezolizumab-bevacizumab group were aspartate aminotransferase (AST) elevation (19.4%), followed by hypertension (10.1%) and skin rash (9.2%), whereas those in the lenvatinib group were AST elevation (49.7%), alanine aminotransferase elevation (38.5%), and total bilirubin elevation (35.5%). Adverse events leading to the discontinuation of treatment occurred in 9 (4.1%) and 10 (6.0%) patients in the atezolizumab-bevacizumab and lenvatinib groups, respectively.
Subsequent therapy
Among patients who failed first-line treatment (n = 146 for the atezolizumab-bevacizumab group and n = 117 for the lenvatinib group), 100 (68.5%) and 94 (80.3%) patients received subsequent treatments, respectively. Among patients in the atezolizumab-bevacizumab group, 99% (n = 99) received MKIs, such as sorafenib, regorafenib, or cabozantinib, while 23% (n = 23) received other ICIs, such as nivolumab (n = 16) or nivolumab-ipilimumab (n = 7). In the lenvatinib group, 46.4% (n = 44) received ICIs as subsequent treatments, while 97.9% (n = 92) received other MKIs (Supplementary Table 3).
Discussion
In this retrospective study, we investigated organ-specific response patterns in unresectable HCC patients treated with first-line atezolizumab-bevacizumab versus lenvatinib. Their overall efficacy and safety outcomes were generally consistent with previous reports, including real-world studies [3, 11, 13,14,15,16,17]. We found that, regardless of the site of the tumor lesions, atezolizumab-bevacizumab was consistently associated with a more favorable organ-specific response than lenvatinib, while there was no notable difference in the tumor response to atezolizumab-bevacizumab across different tumor sites, especially for HCCs with a viral etiology. To our knowledge, this is the first study to report organ-specific responses of HCC patients treated with ICI plus anti-VEGF combination treatment, providing practical insights into treating patients with unresectable HCC with these treatment regimens.
In contrast to the previous reports of organ-specific responses in HCC patients showing that intrahepatic lesions were less responsive to ICI monotherapy [9, 10], our results indicate that intrahepatic lesions also had a more favorable response with atezolizumab-bevacizumab than that with lenvatinib, which was more pronounced when assessed based on the enhancement method adopted from mRECIST. Although the exact mechanisms for this discrepancy remain to be understood, the difference is primarily deemed to be attributable to the addition of bevacizumab to atezolizumab therapy. Our results suggest that there should be no evidence to consider intrahepatic HCC lesions to be less responsive to atezolizumab-bevacizumab, especially for those with viral etiology HCCs.
Mechanistically, inhibition of the VEGF pathway could reverse the immune-suppressive gradient of myeloid cells, including tumor-associated and myeloid-derived suppressor cells [18, 19]. Given that intrahepatic HCC lesions are enriched with various immunosuppressive myeloid cells [20], it is possible that the addition of bevacizumab contributes to improved antitumor efficacy for intrahepatic lesions compared to ICI alone. Indeed, the addition of bevacizumab to atezolizumab improved survival outcomes, particularly in HCC patients with high expression levels of a myeloid gene signature, compared with atezolizumab alone [21]. On the contrary, in a study of metastatic gastric cancer, the presence of liver metastasis, which was associated with the enrichment of tumor-associated macrophages, was associated with poor PFS with anti-PD-1 monotherapy, whereas PFS was not affected by the presence of liver metastasis in patients treated with ICI plus MKIs [22]. These results suggest that the resistance to ICI monotherapy associated with the enrichment of immunosuppressive myeloid cells in the liver might at least, in part, be overcome by adding anti-VEGF agents.
Although our results indicated that intrahepatic HCC lesions were comparably responsive to atezolizumab-bevacizumab as extrahepatic lesions, it should be noted that the proportion of patients achieving a profound intrahepatic tumor burden reduction was limited (5.5% and 3.7% for a ≥ 50% and ≥ 80% reduction in tumor burden, respectively, as per the size method). Given that various novel combination first-line regimens involving novel agents, including anti-TIGIT or anti-LAG-3, are currently being investigated, it will be interesting to see whether these novel combinations could achieve a profound response of intrahepatic lesions.
Despite favorable organ-specific responses with atezolizumab-bevacizumab, there was no difference in PFS between the atezolizumab-bevacizumab and lenvatinib groups. This may be due to the fact that the ORR was not statistically different between the two groups despite the greater extent of the tumor response with atezolizumab-bevacizumab. Moreover, PFS could additionally be affected by the duration of response or disease stabilization. Nevertheless, a numerically higher ORR and a more prominent tumor response may at least in part explain the favorable trend for OS among patients treated with atezolizumab-bevacizumab. The results of the pooled analysis (combining the atezolizumab-bevacizumab and lenvatinib groups) showing that a tumor response in each organ translates into better PFS and OS support our findings. As no prospective head-to-head comparison between atezolizumab-bevacizumab and lenvatinib has been conducted to date, further investigation is required.
In the current analysis, we compared the organ-specific response patterns according to the etiology of HCC between atezolizumab-bevacizumab and lenvatinib. Potential discrepancies in the efficacy outcomes with ICIs according to the etiology have been noted, particularly for the limited ICI efficacy over MKIs in NASH-related HCC in a recent meta-analysis and a large multinational real-world study [23, 24]. Although recent post hoc analysis of the IMBrave150 study showed no relationship in terms of the efficacy outcomes with atezolizumab-bevacizumab per the etiology of HCC [25], our study suggests that the relatively favorable efficacy outcomes with atezolizumab-bevacizumab over lenvatinib may be predominantly seen in patients with a viral etiology HCC, which is in line with a previous report [24]. Unlike the case for HCCs with a viral etiology, which was associated with a consistently better organ-specific response regardless of the site of the tumor lesions, the organ-specific response was not clearly better with atezolizumab-bevacizumab than that with lenvatinib for LN and intraabdominal metastasis. In addition, a profound tumor response (≥ 50% and ≥ 80% reduction in tumor burden) was not observed for intrahepatic HCC lesions with a non-viral etiology. Since the interpretation of this data is limited owing to the small number of patients with a non-viral etiology, these findings need to be validated in an independent cohort. Nevertheless, our results suggest that the etiology of HCC and the site of metastasis should be taken into consideration when making clinical decisions.
There are some limitations to be considered in the current study. Its retrospective nature, the single center-based analysis, and the absence of a validation cohort may limit the interpretation and generalizability of our data. Nevertheless, given the limited reports on organ-specific responses in HCC patients treated in this setting, our results could provide practical insights into selecting ICI-based treatments for patients with HCC. Because our study included only patients in the first-line setting, a bias potentially caused by the development of resistance to previous treatments could be precluded. Moreover, the use of a control group involving patients uniformly treated with lenvatinib enabled us to compare the effect of ICI-based treatment on each specific organ with this multikinase inhibitor. Finally, due to the retrospective nature of the current study, adverse events may not have been fully captured.
In conclusion, atezolizumab-bevacizumab was consistently associated with a more favorable organ-specific response than lenvatinib, regardless of the site of the tumor lesions in patients with unresectable HCC. Intrahepatic HCC lesions should not be considered to be less responsive to atezolizumab-bevacizumab, especially for patients with viral etiology HCCs. The uncertain benefits of organ-specific responses in non-viral etiology HCCs highlight the need to address this question further in future studies.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- ICI:
-
Immune checkpoint inhibitor
- MKI:
-
Multikinase inhibitor
- OS:
-
Overall survival
- LN:
-
Lymph node
- ECOG:
-
Eastern Cooperative Oncology Group
- ALBI:
-
Albumin-bilirubin
- BCLC:
-
Barcelona Clinic Liver Cancer
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- PFS:
-
Progression-free survival
- AST:
-
Aspartate aminotransferase
- IQR:
-
Interquartile range
- ORR:
-
Objective response rate
- CI:
-
Confidence interval
- AFP:
-
Alpha-fetoprotein
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249
Vogel A, Meyer T, Sapisochin G, et al. Hepatocellular carcinoma. Lancet. 2022;400:1345–1362
Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382:1894–1905
Abou-Alfa GK, Lau G, Kudo M, Chan SL, Kelley RK, Furuse J, et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. NEJM Evid. 2022;1:8
Qin S, Chan SL, Gu S, et al. Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): a randomised, open-label, international phase 3 study. Lancet. 2023;402:1133–1146
Hegde S, Krisnawan VE, Herzog BH, et al. Dendritic cell paucity leads to dysfunctional immune surveillance in pancreatic cancer. Cancer Cell. 2020;37(289–307): e9
Donne R, Lujambio A. The liver cancer immune microenvironment: Therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77:1773–1796
Yu J, Green MD, Li S, et al. Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat Med. 2021;27:152–164
Lu LC, Hsu C, Shao YY, et al. Differential organ-specific tumor response to immune checkpoint inhibitors in hepatocellular carcinoma. Liver Cancer. 2019;8:480–490
Kim HS, Kim CG, Hong JY, et al. The presence and size of intrahepatic tumors determine the therapeutic efficacy of nivolumab in advanced hepatocellular carcinoma. Ther Adv Med Oncol. 2022;14:17588359221113266
Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247
Cheon J, Chon HJ, Bang Y, et al. Real-world efficacy and safety of lenvatinib in Korean patients with advanced hepatocellular carcinoma: a multicenter retrospective analysis. Liver Cancer. 2020;9:613–624
Casadei-Gardini A, Scartozzi M, Tada T, et al. Lenvatinib versus sorafenib in first-line treatment of unresectable hepatocellular carcinoma: an inverse probability of treatment weighting analysis. Liver Int. 2021;41:1389–1397
Kuo YH, Lu SN, Chen YY, et al. Real-world lenvatinib versus sorafenib in patients with advanced hepatocellular carcinoma: a propensity score matching analysis. Front Oncol. 2021;11: 737767
Xu YJ, Lai ZC, He MK, et al. Toripalimab combined with hepatic arterial infusion chemotherapy versus lenvatinib for advanced hepatocellular carcinoma. Technol Cancer Res Treat. 2021;20:15330338211063848
Campani C, Vallot A, Ghannouchi H, et al. Impact of radiological response and pattern of progression in patients with hepatocellular carcinoma treated by atezolizumab- bevacizumab. Hepatology. 2023. https://doi.org/10.1016/S0168-8278(23)01389-2
Yang J, Yan J, Liu B. Targeting VEGF/VEGFR to modulate antitumor immunity. Front Immunol. 2018;9:978
Zhang Y, Huang H, Coleman M, et al. VEGFR2 activity on myeloid cells mediates immune suppression in the tumor microenvironment. JCI Insight. 2021. https://doi.org/10.1172/jci.insight.150735
Wu C, Lin J, Weng Y, et al. Myeloid signature reveals immune contexture and predicts the prognosis of hepatocellular carcinoma. J Clin Invest. 2020;130:4679–4693
Zhu AX, Abbas AR, de Galarreta MR, et al. Molecular correlates of clinical response and resistance to atezolizumab in combination with bevacizumab in advanced hepatocellular carcinoma. Nat Med. 2022;28:1599–1611
Yukami H, Kawazoe A, Lin YT, et al. Updated efficacy outcomes of anti-PD-1 antibodies plus multikinase inhibitors for patients with advanced gastric cancer with or without liver metastases in clinical trials. Clin Cancer Res. 2022;28:3480–3488
Pfister D, Nunez NG, Pinyol R, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592:450–456
Casadei-Gardini A, Rimini M, Tada T, et al. Atezolizumab plus bevacizumab versus lenvatinib for unresectable hepatocellular carcinoma: a large real-life worldwide population. Eur J Cancer. 2023;180:9–20
Espinoza M, Muquith M, Lim M, et al. Disease etiology and outcomes after atezolizumab plus bevacizumab in hepatocellular carcinoma: post-hoc analysis of IMbrave150. Gastroenterology. 2023;165:286–8.e4
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Study concepts: HDK and CY; study design: HDK and CY; data acquisition: HDK, YGP, SK, KPK, SRP, MHR, BYR, and CY; data analysis and interpretation: HDK, YGP, and CY; statistical analysis: HDK and YGP; manuscript preparation: HDK and YGP; manuscript editing: HDK, YGP, and CY; manuscript review and approval: HDK, YGP, SK, KPK, SRP, MHR, BYR, and CY.
Corresponding author
Ethics declarations
Conflict of interest
CY received honoraria from Servier, Bayer, AstraZeneca, Merck Sharp & Dohme, Eisai, Celgene, Bristol Myers Squibb, Ipsen, Novartis, Boryung Pharmaceuticals, Mundipharma, and Roche, and received research grants from Servier, Bayer, AstraZeneca, Ono Pharmaceuticals, Ipsen, and Boryung Pharmaceuticals. HDK received honoraria from AstraZeneca, Bristol Myers Squibb, Ono Pharmaceuticals, Boryung Pharmaceuticals, and Boostimmune. The other authors have nothing to disclose.
Ethical approval and informed consent
This study was approved by the Institutional Review Board of Asan Medical Center (IRB No. 2021-0064) and was performed in accordance with the ethical standards of the Institutional Research Committee and the latest Declaration of Helsinki. The need for informed consent was waived by the Institutional Review Board of Asan Medical Center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, HD., Park, YG., Kim, S. et al. Organ-specific response with first-line atezolizumab-bevacizumab versus lenvatinib for patients with advanced hepatocellular carcinoma. Hepatol Int 18, 973–983 (2024). https://doi.org/10.1007/s12072-023-10626-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10626-6