Abstract
Background and aims
Fatty liver disease (FLD) is associated with several metabolic derangements. We conducted a retrospective cross-sectional and longitudinal study to evaluate the role of FL severity in the risk of new-onset and co-existing hypertension (HTN) and diabetes mellitus (DM).
Methods
The cross-sectional cohort consisted of 41,888 adults who received health checkups in a tertiary hospital of Taiwan from 1999 to 2013. Of them, 34,865 without HTN and/or DM at baseline and within 1 year after enrollment were included as a longitudinal cohort (mean, 6.45 years for HTN; 6.75 years for DM). FL severity based on the degree of hepatic steatosis was assessed by ultrasound sonography.
Results
In cross-sectional cohort, 22,852 (54.6%) subjects had FL (18,203 [43.46%] mild FL and 4,649 [11.10%] moderate/severe FL); 13.5% (n = 5668) had HTN; and 3.4% (n = 1411) had DM. Moderate/severe FL and mild FL had significantly higher risks of existing HTN (adjusted odds ratio/95% confidence interval [CI] 1.59/1.43–1.77 and 1.22/1.13–1.32, respectively). In longitudinal cohort, 3,209 and 822 subjects developed new-onset HTN and DM, respectively (annual incidence, 14.3 and 3.5 per 1000 person-years; 10-year cumulative incidence, 14.35% and 3.89%, respectively). Moderate/severe and mild FL had significantly higher risks of new-onset HTN (adjusted hazard ratio [aHR]/CI 1.54/1.34–1.77 and 1.26/1.16–1.37, respectively) and DM (aHR/CI 5.88/4.44–7.81 and 3.22/2.56–4.07, respectively). Resolved FL during follow-up decreased the risk of HTN and/or DM.
Conclusions
Patients with FL are at high risk of prevalent and incident HTN and/or DM. The risk increases with the severity of FL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is the most common form of chronic liver disease, which can lead to hepatocellular carcinoma and end-stage liver disease [1, 2]. Approximately 25% of people have NAFLD globally [3]. Despite the growing disease burden of NAFLD, there remains a significant gap in the awareness and knowledge of NAFLD among physicians and policy makers [4, 5].
NAFLD is considered to be a hepatic component of a multisystem disease stemming from insulin resistance and is highly associated with metabolic syndrome, including hypertension (HTN), type 2 diabetes mellitus (DM), and dyslipidemia [6,7,8]. NAFLD is associated with a significantly higher risk of developing incident HTN [9, 10] and incident DM [11, 12], which have been the major causes of death for NAFLD and metabolic syndrome [13]. However, little is known about the risk of NAFLD severity and risk of HTN and DM.
Recently, a new nomenclature of FLD, metabolic dysfunction-associated FLD (MAFLD), was proposed based on the co-existence of FL and metabolic abnormality, without excluding other etiologies such as chronic viral hepatitis [14, 15]. The spectrum of MAFLD may help identify individuals with metabolically complicated FL, who are at higher risk of cardiovascular disease [16].
In this study, we aimed to evaluate the role of FL severity and the risk of HTN and DM in Taiwan, a country hyperendemic for hepatitis B virus (HBV) and hepatitis C virus (HCV) infections [17, 18]. We adopted a cross-sectional and longitudinal cohort design to investigate the risk factors associated with co-existing (prevalent) and new-onset (incident) HTN and DM.
Materials and methods
Population
A total of 509,239 person-visits (225,308 subjects) to the Department of Preventive Medicine and Health Management Center, Kaohsiung Medical University Hospital (KMUH) for health checkups between 1999 and 2013, were screened for the current study. Information that identifies the research subjects were eliminated from the dataset before commencement.
Cross-sectional cohort
A total of 41,922 subjects (259,927 person-visits), who visited the department at least twice, were aged 18–65 years during the first visit, and had complete anthropometric measurement, blood test data available, and liver ultrasound sonography (USG), were initially enrolled in the study. Twenty-three subjects with suspected alcoholic-related liver disease (ratio of serum aspartate aminotransferase (AST) to alanine aminotransferase (ALT) level > 2 and AST level > 2 times the upper limit of normal or with heavy alcohol consumption (≥ 5 drinks on any day or ≥ 15 per week in men and ≥ 4 drinks on any day or ≥ 8 per week in female for > 5 years) [19, 20] and 11 subjects with a history of major organ transplantation were excluded. Consequently, the cross-sectional cohort was established with a total 41,888 subjects to evaluate the correlation between FL and the presence of existing HTN and DM at enrollment (Supplementary Fig. 1).
Longitudinal cohort
To evaluate the impact of FL on the incidence of new-onset HTN and/or DM, 6,529 subjects with HTN and/or DM at baseline and 445 subjects with HTN and/or DM diagnosed within 1 year after enrollment, and 49 subjects with an estimated glomerular filtration rate < 30 mL/min/1.73 m2 were excluded. Finally, 34,865 subjects were included as the longitudinal cohort for statistical analyses (Supplementary Fig. 1).
Assessment of FL
Abdominal USG was performed by 8 well-trained and qualified hepatologists at KMUH, using Toshiba SSA-250, SSA-520A, and SSA-660A devices with 3.5 MHz convex transducers (Toshiba, Tokyo, Japan). The diagnosis of FL was based on brightness of the liver on USG compared with the kidney, vascular blurring of the hepatic vein trunk, and deep attenuation in the right hepatic lobe. The severity of FL was classified as: 1) no FL, a normal echo texture and absence of fatty changes; 2) mild FL, a mild increase in fine echoes in the liver parenchyma with blurring of diaphragm and intrahepatic vessels; and 3) moderate/severe FL, a marked increase in fine echoes in the parenchyma with poorly visible or invisible intrahepatic vessels, diaphragm, and posterior right lobe of the liver. USG is a reliable and accurate imaging technique to screen FL [21, 22].
Follow-up FL examination
During each follow-up visit, the participants underwent USG examination. Follow-up FL status was defined as the severity of FL measured by USG at the time when participants developed new-onset HTN or DM. For participants who did not develop new-onset HTN or DM, the FL measured by USG findings at the last visit were used as their follow-up FL status.
Definitions of pre-HTN, HTN, impaired fasting glucose, and DM
Pre-HTN is defined as a systolic blood pressure (SBP) of 120–139 mmHg and diastolic BP (DBP) of 80–89 mmHg. HTN is defined as persistent SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or the use of antihypertensive agents [23]. The year of new-onset HTN was defined as the first year in the series during which time the subjects met the definition of HTN or began using antihypertensive agents.
Impaired fasting glucose (IFG) is defined as a serum FG level of 100–125 mg/dL, and DM is defined as FG ≥ 126 mg/dL or the use of antihyperglycemic agents [24]. The year of new-onset DM was defined as the first year during which time the subjects met the definition of DM or began taking antihyperglycemic agents.
Laboratory data
FG, AST, ALT, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), total cholesterol and triglycerides, HBV surface antigen (HBsAg), HCV antibody (anti-HCV), and histories of antihypertensive and antihyperglycemic treatments were retrieved. Body mass index (BMI) cut-offs were suggested by the Health Promotion Administration in Taiwan (normal weight 18.5–23.9 kg/m2, overweight 24–26.9 kg/m2, and obese ≥ 27 kg/m2).
Statistical analyses
Data were analyzed with JMP version 10 (SAS Inc., Cary, NC, USA). Cohort characteristics were described using numbers with percentage (%), and the results of continuous variables are expressed as the mean ± standard deviation. Pearson’s chi-square test was used to analyze the dichromatic differences. Factors with p < 0.1 in univariate analyses were further evaluated in multiple logistic regression analyses [25]. Kaplan–Meier survival curves were used to determine the cumulative incidences and lifetime risk of new-onset HTN and DM. Adjusted hazard ratios (aHRs) for factors associated with new-onset HTN and DM were determined using the Cox proportional hazards model. All tests were two-tailed, and statistical significance was set at p < 0.05.
Results
Cross-sectional cohort
Of the 41,888 subjects in the cross-sectional cohort (Table 1, mean age: 40.4 years) 80.9% were male, 19.4% seropositive for HBsAg, and 2.7% seropositive for anti-HCV. A total of 22,852 (54.6%) subjects had FL, including 18,203 (43.46%) with mild FL and 4,649 (11.10%) with moderate/severe FL (Supplementary Table 1 and Supplementary Table 2). The prevalence rates of existing HTN and DM were 13.5% (n = 5668) and 3.4% (n = 1411), respectively.
Factors associated with existing HTN in the cross-sectional cohort
The prevalence of existing HTN in the cross-sectional cohort was 7.75% (1476/19036), 16.66% (3033/18203), and 24.93% (1159/4649) among subjects without FL, with mild FL, and with moderate/severe FL, respectively. In multivariate regression analyses, older age (56–65 years) and (46–55 years), obesity, and DM had leading adjusted odds ratio (aORs) of 7.11, 5.37, 3.51, and 2.13 respectively. Moderate/severe and mild FL were significantly associated with a higher risk of existing HTN (aOR/95% confidence intervals [CIs] 1.59/1.43–1.77 and 1.22/1.13–1.32, respectively). Male, hypercholesterolemia, hypertriglyceridemia, higher AST and ALT levels, smoking, and HBsAg seropositivity were also associated with existing HTN (Supplementary Table 1).
Factors associated with existing DM in the cross-sectional cohort
The prevalence of existing DM in the cross-sectional cohort was 1.46% (277/19,036), 4.21% (766/18,203), and 7.92% (368/4,649) among subjects without FL, with mild FL, and with moderate/severe FL, respectively. In multivariate regression analyses for risk of existing DM, older age (56–65 years) and (46–55 years), moderate/severe FL, and HTN had leading aORs of 16.48, 10.70, 2.63, and 2.36 respectively, followed by hypertriglyceridemia, AST and ALT levels, and obesity. Moderate/severe FL and mild FL were significantly associated with a higher risk of existing DM (aOR/CI: 2.63/2.17–3.19 and 1.72/1.48–2.01). High BMI, pre-HTN and HTN, hypertriglyceridemia, and higher AST and ALT levels were also significantly associated with existing DM (Supplementary Table 2).
Longitudinal cohort
Of 34,865 subjects in the longitudinal cohort (Table 1, mean age 39.4 years) 78.9% were male, 19.6% seropositive for HBsAg, and 2.5% seropositive for anti-HCV. We censored the date according to the events analyzed, such as the time of HTN or DM development if the participants developed new-onset of HTN or DM. On an average, participants underwent the health check-up process 6 times before reaching to their endpoints or last visit. In the assessment of HTN development, the mean follow-up period was 6.45 (± 4.18) years (range, 1–14 years). The mean follow-up period was 6.75 (± 4.31) years (range, 1–14 years) in the assessment of DM development.
Incidence and risk of new-onset HTN in the longitudinal cohort
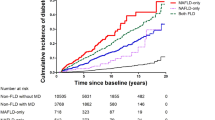
A total of 3,208 subjects developed new-onset HTN during 224,810 person-years follow-up (annual incidence, 14.3/1,000 person-years). The 3-, 5-, 7- and 10-year cumulative incidences of HTN were 2.56%, 5.57%, 8.92%, and 14.35%, respectively. The cumulative lifetime risk of HTN at 40, 50, 60, and 65 years old was 1.35%, 8.71%, 24.41%, and 32.93%, respectively (Fig. 1, Supplementary Table 3).
Risk of new-onset HTN and severity of FL
Among the 17,233 subjects without FL, 1,037 (6.02%) developed HTN during 109,981 person-years follow-up (annual incidence, 9.4/1000 person-years). For the 14,427 subjects with mild FL, 1,834 (12.71%) developed HTN during 100,695 person-years follow-up (annual incidence, 18.2/1000 person-years). Of the 4,649 subjects with moderate/severe FL, 337 (10.51%) developed HTN during 14,134 person-years follow-up (annual incidence, 23.8/1000 person-years).
In Kaplan–Meier analysis, the 3-, 5-, 7- and 10-year cumulative incidences of HTN were 1.57%, 3.51%, 5.79% and 9.49%, respectively, in subjects without FL, compared to 3.21%, 6.96%, 11.08%, and 17.89%, respectively, in subjects with mild FL (crude HR [cHR]/CI 1.89/1.75–2.04), and 4.96%, 10.71%, 16.97% and 26.16%, respectively, in subjects with moderate/severe FL (cHR/CI 2.97/2.62–3.36). The cumulative lifetime risk of HTN at 40, 50, 60, and 65 years old was 0.73%, 5.93%, 18.65%, and 25.88%, respectively, in subjects without FL, compared to 1.59%, 10.46%, 28.57%, and 37.23%, respectively, in subjects with mild FL (cHR/CI: 1.74/1.61–1.88), and 3.54%, 14.66%, 32.18%, and 45.92%, respectively, in subjects with moderate/severe FL (cHR/CI: 2.37/2.10–2.69; Fig. 2, Supplementary Table 4 and Supplementary Table 5).
Factors associated with new-onset HTN
In Cox proportional regression analyses, pre-HTN at baseline had the highest risk of developing HTN (aHR/CI 4.23/3.75–4.75) followed by older age (56–65 years; aHR/CI 2.31/1.75–3.07) (46–55 years; aHR/CI 2.22/1.99–2.50) and obesity (aHR/CI: 1.93/1.74–2.14). Subjects with mild FL and moderate/severe FL remained at significantly higher risk of new-onset HTN (aHR/CI: 1.26/1.16–1.37 and 1.54/1.34–1.77, respectively), compared to those without FL. Male sex, smoking, anti-HCV seropositivity, IFG, and higher level of TG were also significantly associated with new-onset HTN (Table 2).
Risk of new-onset HTN and change in severity of FL during follow-up (Table 3)
Among 17,233 subjects without FL at baseline, 3604 (20.91%) developed mild FL and 758 (4.39%) developed moderate/severe FL at censored date or last visit. The annual incidence of new-onset HTN was 8.2/1000 person-years for subjects with persistent no FL, 12.2/1000 person-years for subjects progressing to mild FL and 15.5/1000 person-years for those progressing to moderate/severe FL. Cox proportional regression analyses showed that the risk of new-onset HTN was significantly higher in those developing mild FL (aHR/CI 1.54/1.33–1.78) and moderate/severe FL (aHR/CI: 1.76/1.41–2.19) compared to those who remained no FL.
Among 14,427 subjects with mild FL at baseline, 4,528 (31.39%) regressed to no FL and 3,577 (24.79%) progressed to moderate/severe FL at censored date or last visit. The annual incidence of HTN was 10.7/1000 person-years for FL regressed subjects, 23.3/1000 person-years for persistent mild FL subjects, and 20.5/1000 person-years for FL progressed subjects. Cox proportional regression analysis showed that FL regressed individuals had a significantly lower risk of new-onset HTN (aHR/CI: 0.46/0.40–0.52 and aHR/CI: 0.59/0.52–0.68, respectively), compared to those who remained with mild FL and those who progressed to moderate/severe FL.
Among 4649 subjects with moderate/severe FL at baseline, 266 (5.72%) had no FL at end-of-follow-up and 841 (18.09%) regressed to mild FL at censored date or last visit. The annual incidence of HTN was 17.7/1,000 person-years for FL resolved subjects, 24.1/1,000 person-years for subjects with regression to mild FL, and 24.8/1000 person-years for those with persistent moderate/severe FL. Cox proportional regression analysis showed that FL resolved individuals had a significantly lower risk of new-onset HTN (aHR/CI 0.66/0.44–1.00) compared to those who remained with moderate/severe FL.
Incidence and risk of new-onset DM in the longitudinal cohort
A total of 822 subjects developed new-onset DM during 235,499 person-years follow-up (annual incidence, 3.5/1000 person-years). The 3-, 5-, 7- and 10-year cumulative incidences of DM were 0.62%, 1.39%, 2.36%, and 3.89%, respectively. The cumulative lifetime risk of DM at 40, 50, 60, and 65 years old was 0.30%, 1.94%, 6.90%, and 10.57%, respectively (Fig. 1, Supplementary Table 3).
Risk of new-onset DM and severity of FL
Among the 17,233 subjects without FL, 93 (0.54%) developed DM during 114,081 person-years follow-up (annual incidence, 0.8/1000 person-years). For the 18,203 subjects with mild FL, 560 (4.21%) developed DM during 106,582 person-years follow-up (annual incidence, 5.3/1000 person-years). Of the 4649 subjects with moderate/severe FL, 169 (7.92%) developed DM during 14,836 person-years follow-up (annual incidence, 11.4/1000 person-years).
In Kaplan–Meier analysis, the 3-, 5-, 7- and 10-year cumulative incidences of DM were 0.12%, 0.34%, 0.57%, and 0.85%, respectively, in subjects without FL, compared to 0.93%, 2.02%, 3.41%, and 5.73%, respectively, in subjects with mild FL (cHR/CI 6.26/5.03–7.80), and 1.99%, 4.54%, 8.64%, and 15.38%, respectively, in subjects with moderate/severe FL (cHR/CI 16.18/12.55–20.87). The cumulative lifetime risk of DM at 40, 50, 60, and 65 years old was 0.08%, 0.47%, 1.85%, and 2.54%, respectively, in subjects without FL, compared to 0.37%, 2.78%, 9.71%, and 14.03%, respectively, in subjects with mild FL (cHR/CI 5.83/4.68–7.27), and 1.19%, 5.78%, 20.75%, and 40.20%, respectively, in subjects with moderate/severe FL (cHR/CI 13.58/10.53–17.51; Fig. 3, Supplementary Tables 6 and 7).
Factors associated with new-onset DM
In Cox proportional regression analyses, moderate/severe FL (aHR/CI 5.88/4.44–7.81) had the highest risk of developing new-onset DM followed by IFG (aHR/CI 4.54/3.92–5.25), older age (56–65 years, aHR/CI 3.84/2.36–6.24), and mild FL (aHR/CI 3.22/2.56–4.07). Male sex, obesity, smoking, anti-HCV seropositivity, pre-HTN, IFG, and higher levels of TG and ALT were also significantly associated with the risk of new-onset DM (Table 4).
Risk of new-onset DM and change in severity of FL during follow-up (Table 5)
Among the 17,233 subjects without FL at baseline, 3572 (20.72%) developed mild FL and 792 (4.60%) developed moderate/severe FL at censored date or last visit. The annual incidence of new-onset DM was 0.34/1000 person-years for subjects with persistent no FL, 0.98/1,000 person-years for subjects progressing to mild FL and 1.77/1000 person-years for those progressing to moderate/severe FL. Cox proportional regression analyses showed that subjects developing mild FL and moderate/severe FL had significantly higher risks of new-onset DM (aHR/CI 2.22/1.41–3.48 and 2.81/1.51–5.21, respectively), compared to those who remained without FL.
Among 14,427 subjects with mild FL at baseline, 4,572 (31.70%) resolved FL and 3,745 (25.96%) deteriorated to moderate/severe FL at censored date or last visit. The annual incidence of DM was 1.42/1000 person-years for FL regressed subjects, 3.83/1000 person-years for persistent mild FL subjects, and 6.97/1000 person-years for FL progressed subjects. Cox proportional regression analysis showed that subjects who resolved FL had a significantly lower risk of new-onset DM (aHR/CI: 0.36/0.27–0.47 and 0.32/0.24–0.42, respectively) compared to those who remained mild FL and those who progressed to moderate/severe FL.
Among 4,649 subjects with moderate/severe FL at baseline, 256 (5.51%) resolved FL, while 837 (18.00%) regressed to mild FL at censored date or last visit. Cox regression analysis showed that subjects who resolved FL had a significantly lower risk of new-onset DM compared to those who regressed to mild FL and those who remained with moderate/severe FL (aHR/CI: 0.22/0.08–0.63 and 0.20/0.08–0.55, respectively).
Incidence of new onset of concomitant HTN and DM in the longitudinal cohort
A total of 252 subjects developed new-onset concomitant HTN and DM during 238,058 person-years follow-up (annual incidence, 1.1/1000 person-years). The 3-, 5-, 7- and 10-year cumulative incidences of concomitant HTN and DM were 0.05%, 0.23%, 0.55%, and 1.20%, respectively. The cumulative lifetime risk of concomitant HTN and DM at 40, 50, 60, and 70 years old was 0.06%, 0.52%, 2.31%, and 4.42%, respectively (Fig. 1, Supplementary Table 3).
Risk of new-onset concomitant HTN and DM and severity of FL
Among the 17,233 subjects without FL, 21 (0.12%) developed both HTN and DM during 114,400 person-years follow-up (annual incidence, 0.2/1,000 person-years). For the 14,427 subjects with mild FL, 163 (1.13%) developed DM during 108,416 person-years follow-up (annual incidence, 1.5/1,000 person-years). Of the 3,205 subjects with moderate/severe FL, 68 (2.12%) developed both HTN and DM during 15,242 person-years follow-up (annual incidence, 4.5/1,000 person-years).
In Kaplan–Meier analysis, the 3-, 5-, 7-, and 10-year cumulative incidences of both HTN and DM were 0.01%, 0.02%, 0.08%, and 0.18%, respectively, in subjects without FL, compared to 0.07%, 0.33%, 0.73%, and 3.16%%, respectively, in subjects with mild FL (cHR/CI 7.66/4.86–12.07), and 0.17%, 0.96%, 3.16%, and 11.758%, respectively, in subjects with moderate/severe FL (cHR/CI 33.41/20.46–54.56). The cumulative lifetime risk of both HTN and DM at 40, 50, 60, and 70 years old was 0.01%, 0.10%, 0.46%, and 0.69%, respectively, in subjects without FL, compared to 0.08%, 0.74%, 3.12%, and 6.91%, respectively, in subjects with mild FL (cHR/CI 7.39/4.69–11.64), and 0.29%, 1.74%, 9.36%, and 14,36%, respectively, in subjects with moderate/severe FL (cHR/CI 23.71/14.54–38.69; Fig. 4, Supplementary Tables 8 and 9).
Factors associated with new-onset concomitant HTN and DM
In Cox proportional regression analyses, moderate/severe FL (aHR/CI 9.10/5.33–15.54) had the highest risk of developing both HTN and DM, followed by pre-HTN (aHR/CI: 4.18/2.54–6.86), mild FL (aHR/CI 3.42/2.13–5.50), IFG (aHR/CI 3.40/2.63–4.40), and obesity (BMI ≥ 27 kg/m2, aHR/CI 3.09/2.07–4.63). Age, obesity, smoking, anti-HCV seropositivity, and higher levels of TG, AST, and ALT were also significantly associated with the risk of new-onset DM and HTN (Table 6).
Discussion
In the current large-scale study, we demonstrated that patients with FL were at a high risk of HTN and DM in both cross-sectional and longitudinal settings, and the risk increased with the FL severity. The prevalence of HTN and DM among subjects without FL, with mild FL, and with moderate/severe FL was 7.75% and 1.46%, 16.66% and 4.21%, and 24.93% and 7.92%, respectively. The annual incidences of incident HTN and DM among subjects without FL, with mild FL, and with moderate/severe FL were 9.4 and 0.8, 18.2 and 5.3, and 23.8 and 11.4 per 1000 person-years, respectively, with a 10-year cumulative incidence rate of 9.49% and 0.85%, 17.89% and 5.73%, 26.16% and 15.38%, respectively.
Consistent with previous studies [12, 26,27,28], we further demonstrated that mild FL and moderate/severe FL were correlated with a 1.22- and 1.59-fold risk of co-existing HTN, respectively, in the general population and a 1.26- and 1.54-fold risk of developing new-onset HTN, respectively, among those without baseline HTN. Similarly, we also found that mild FL and moderate/severe FL were associated with a 1.72- and 2.63-fold risk of co-existing DM, respectively, in the general population and a 3.22- and 5.88-fold risk of developing new-onset DM, respectively.
Studies have shown that the combination of HTN and DM increases the risk of stroke and microvascular and macrovascular complications [29,30,31]. Notably, in our study, mild FL and moderate/severe FL were associated with a 3.42- and 9.1-fold risk of developing new-onset concomitant DM and HTN, even among younger subjects. Our findings show that moderate/severe FL is the leading risk factor for developing concurrent DM and HTN, and patients should be monitored carefully for the development of these conditions. Therefore, screening of FL allows the early identification of risk of HTN and DM, which could help with the application of early intervention with lifestyle modification and weight reduction to avoid the progression of FL and prevent HTN and DM development [32].
Uncontrolled HTN is found in more than half of FL patients with HTN [28]. Cardiovascular disease is the leading cause of mortality in FL patients [13]. Therefore, screening for HTN in patients with FL and implementing appropriate interventions to control BP as well as cardiovascular risk would benefit the overall health outcomes.
We also observed that pre-HTN, older age, obesity, male sex, smoking, and hypertriglyceridemia were significantly associated with a higher risk of new-onset HTN, as observed in a nationwide survey in Japan [33]. Similarly, IFG, older age, obesity, hypertriglyceridemia, smoking, and male sex were also the leading factors of developing DM. These results suggest that early lifestyle modification such as quitting smoking, weight reduction, and control of pre-HTN and/or IFS play important roles in preventing HTN and/or DM.
Notably, we observed a significant impact of resolved and progressed FL during follow-up in the risk of HTN and DM. It demonstrated that the development or progression of FL are significantly associated with increased risks of developing HTN and DM. Conversely, FL regression or resolved are associated with reduced risks of developing HTN and DM. These findings suggest the importance of monitoring and managing fatty liver as a potential risk factor for HTN and DM. Life style modification, exercise and diet control, which have been associated with improvement of FL [34], might have benefits in risk reduction for HTN and DM among subjects with significant FL.
Moreover, we observed a strong interaction between HTN and DM. Patients with IFG have a higher risk of developing HTN as previously reported [35], and patients with pre-HTN have a higher risk of developing DM. A possible pathophysiology is that insulin resistance affects the body’s ability to regulate BP, causing an increase in peripheral vascular resistance and volume of circulatory fluid, which further activates the sympathetic nervous system, leading to the development of HTN in patients with DM [36].
This study had some limitations. First, no data on mortality was available. We were unable to evaluate the risk of mortality among subjects who developed HTN and/or DM. Second, the severity of FL was assessed by USG instead of a pathologic method or other new technologies, such as controlled attenuation parameter or magnetic resonance imaging [37]. However, abdominal USG is a widely used, well-established, and lower-cost imaging technique with high sensitivity and specificity. Although liver biopsy is the gold standard for the diagnosis of FL, it has limitations such as costliness, sampling error, and invasiveness [38]. Third, because no pharmaceutical agents approved for FL in the study period, all patients with FL were advised to execute life style modification, exercise and diet control. However, we were unable to obtain the data regarding the adherence of the advice among the participants.
In conclusion, FL is a significant risk factor for both prevalent and incidental HTN and DM; the risk increases with the severity of FL. Subjects with moderate/severe FL are at high risk of developing concomitant HTN and DM. Regression of or resolved FL reduced the risks of HTN and DM. Thus, early intervention for FL with lifestyle modification and regular surveillance for HTN and DM should be mandatory for FL patients.
Data availability
The datasets generated and analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- aHR:
-
Adjusted hazard ratio
- ALT:
-
Alanine aminotransferase
- aOR:
-
Adjusted odds ratio
- AST:
-
Aspartate aminotransferase
- BS:
-
Blood sugar
- cHR:
-
Crude HR
- CLR:
-
Cumulative lifetime risk
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes
- FL:
-
Fatty liver
- FLD:
-
Fatty liver disease
- HDL-C:
-
High-density lipoprotein cholesterol
- HTN:
-
Hypertension
- IFG:
-
Impaired fasting glucose
- LDL-C:
-
Low-density lipoprotein cholesterol
- NAFLD:
-
Non-alcoholic fatty liver disease
- SBP:
-
Systolic blood pressure
- USG:
-
Ultrasound sonography
References
Alqahtani SA, Chan WK, Yu ML. Hepatic outcomes of nonalcoholic fatty liver disease including cirrhosis and hepatocellular carcinoma. Clin Liver Dis 2023;27(2):211–223. https://doi.org/10.1016/j.cld.2023.01.019
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15(1):11–20. https://doi.org/10.1038/nrgastro.2017.109
Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77(4):1335–1347. https://doi.org/10.1097/HEP.0000000000000004
Younossi ZM, Ong JP, Takahashi H, et al. A global survey of physicians knowledge about nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2022;20(6):e1456–e1468. https://doi.org/10.1016/j.cgh.2021.06.048
Lazarus JV, Mark HE, Anstee QM, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol 2022;19(1):60–78. https://doi.org/10.1038/s41575-021-00523-4
Dietrich P, Hellerbrand C. Non-alcoholic fatty liver disease, obesity and the metabolic syndrome. Best Pract Res Clin Gastroenterol 2014;28(4):637–653. https://doi.org/10.1016/j.bpg.2014.07.008
Wu KT, Kuo PL, Su SB, et al. Nonalcoholic fatty liver disease severity is associated with the ratios of total cholesterol and triglycerides to high-density lipoprotein cholesterol. J Clin Lipidol 2016;10(2):420-425.e1. https://doi.org/10.1016/j.jacl.2015.12.026
Hsiao PJ, Kuo KK, Shin SJ, et al. Significant correlations between severe fatty liver and risk factors for metabolic syndrome. J Gastroenterol Hepatol 2007;22(12):2118–2123. https://doi.org/10.1111/j.1440-1746.2006.04698.x
Huh JH, Ahn SV, Koh SB, et al. A prospective study of fatty liver index and incident hypertension: the KoGES-ARIRANG study. PLoS One 2015;10(11):e0143560. https://doi.org/10.1371/journal.pone.0143560
Tang X, Shi Y, Du J, et al. Clinical outcome of non-alcoholic fatty liver disease: an 11-year follow-up study. BMJ Open 2022;12(6):e054891. https://doi.org/10.1136/bmjopen-2021-054891
Park SK, Seo MH, Shin HC, Ryoo JH. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology. 2013;57(4):1378–1383. https://doi.org/10.1002/hep.26183
Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis. Diabetes Care 2018;41(2):372–382. https://doi.org/10.2337/dc17-1902
Francque S, Szabo G, Abdelmalek MF, et al. Nonalcoholic steatohepatitis: the role of peroxisome proliferator-activated receptors. Nat Rev Gastroenterol Hepatol 2021;18(1):24–39. https://doi.org/10.1038/s41575-020-00366-5
Eslam M, Sanyal AJ, George J, International Consensus P. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999-2014.e1. https://doi.org/10.1053/j.gastro.2019.11.312
van Kleef LA, Ayada I, Alferink LJM, Pan Q, de Knegt RJ. Metabolic dysfunction-associated fatty liver disease improves detection of high liver stiffness: the Rotterdam study. Hepatology. 2022;75(2):419–429. https://doi.org/10.1002/hep.32131
Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol 2021;19(10):2138-2147.e10. https://doi.org/10.1016/j.cgh.2020.12.022
Yang JF, Lin CI, Huang JF, et al. Viral hepatitis infections in southern Taiwan: a multicenter community-based study. Kaohsiung J Med Sci 2010;26(9):461–469. https://doi.org/10.1016/S1607-551X(10)70073-5
Tsai PC, Huang CI, Yeh ML, et al. Significant amelioration of hepatitis C virus infection in a hyperendemic area: longitudinal evidence from the COMPACT Study in Taiwan. BMJ Open 2021;11(3):e042861. https://doi.org/10.1136/bmjopen-2020-042861
European Association for the Study of L. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol 2012;57(2):399–420. https://doi.org/10.1016/j.jhep.2012.04.004
Dunn W, Angulo P, Sanderson S, et al. Utility of a new model to diagnose an alcohol basis for steatohepatitis. Gastroenterology. 2006;131(4):1057–1063. https://doi.org/10.1053/j.gastro.2006.08.020
Hernaez R, Lazo M, Bonekamp S, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54(3):1082–1090. https://doi.org/10.1002/hep.24452
Lee CM, Yoon EL, Nakajima A, et al. A reappraisal of the diagnostic performance of b-mode ultrasonography for mild liver steatosis. Am J Gastroenterol 2023;118(5):840–847. https://doi.org/10.14309/ajg.0000000000002020
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol 2018;71(19):e127–e248. https://doi.org/10.1016/j.jacc.2017.11.006
Love-Osborne K. Chapter 4—prediabetes and type 2 diabetes: an emerging epidemic among obese youth. In Bagchi D, editor., Global perspectives on childhood obesity. 2nd ed. Cambridge: Academic Press; 2019. 37–47
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285(19):2486–97. doi:https://doi.org/10.1001/jama.285.19.2486
Li G, Peng Y, Chen Z, Li H, Liu D, Ye X. Bidirectional association between hypertension and NAFLD: a systematic review and meta-analysis of observational studies. Int J Endocrinol 2022;2022:8463640. https://doi.org/10.1155/2022/8463640
Ryoo JH, Suh YJ, Shin HC, Cho YK, Choi JM, Park SK. Clinical association between non-alcoholic fatty liver disease and the development of hypertension. J Gastroenterol Hepatol 2014;29(11):1926–1931. https://doi.org/10.1111/jgh.12643
Kasper P, Martin A, Meyer Zu Schwabedissen A, et al. Uncontrolled hypertension: a neglected risk in patients with NAFLD. J Intern Med 2022;292(1):162–164. https://doi.org/10.1111/joim.13476
Hu G, Sarti C, Jousilahti P, et al. The impact of history of hypertension and type 2 diabetes at baseline on the incidence of stroke and stroke mortality. Stroke. 2005;36(12):2538–2543. https://doi.org/10.1161/01.STR.0000190894.30964.75
Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol 2018;34(5):575–584. https://doi.org/10.1016/j.cjca.2017.12.005
Ninomiya T, Kubo M, Doi Y, et al. Impact of metabolic syndrome on the development of cardiovascular disease in a general Japanese population: the Hisayama study. Stroke. 2007;38(7):2063–2069. https://doi.org/10.1161/STROKEAHA.106.479642
Francque SM, Marchesini G, Kautz A, et al. Non-alcoholic fatty liver disease: a patient guideline. JHEP Rep 2021;3(5):100322. https://doi.org/10.1016/j.jhepr.2021.100322
Toshikuni N, Tsuchishima M, Fukumura A, Arisawa T, Tsutsumi M. Associations of fatty liver disease with hypertension, diabetes, and dyslipidemia: comparison between alcoholic and nonalcoholic steatohepatitis. Gastroenterol Res Pract 2017;2017:9127847. https://doi.org/10.1155/2017/9127847
Eslam M, Sarin SK, Wong VW, et al. The Asian pacific association for the study of the liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int 2020;14(6):889–919. https://doi.org/10.1007/s12072-020-10094-2
Ding X, Xu Y, Wang Y, et al. Nonalcoholic fatty liver disease and associated metabolic risks of hypertension in type 2 diabetes: a cross-sectional community-based study. Int J Endocrinol 2017;2017:5262560. https://doi.org/10.1155/2017/5262560
Przezak A, Bielka W, Pawlik A. Hypertension and type 2 diabetes & mdash; the novel treatment possibilities. Int J Mol Sci 2022. https://doi.org/10.3390/ijms23126500
Lv S, Jiang S, Liu S, Dong Q, Xin Y, Xuan S. Noninvasive quantitative detection methods of liver fat content in nonalcoholic fatty liver disease. J Clin Transl Hepatol 2018;6(2):217–221. https://doi.org/10.14218/JCTH.2018.00021
Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128(7):1898–1906. https://doi.org/10.1053/j.gastro.2005.03.084
Acknowledgements
This study was supported by the Ministry of Health and Welfare, Pingtung Hospital, Kaohsiung Medical University Hospital, Taiwan Liver Research Foundation, and " Center For Intelligent Drug Systems and Smart Bio-devices (IDS2B), National Yang Ming Chiao Tung University " and “ Center of Excellence for Metabolic Associated Fatty Liver Disease, National Sun Yat-sen University” from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.. The authors thank the secretaries of the Hepatobiliary Division of Kaohsiung Medical University Hospital.
Funding
This work was supported in part by a grant from 1. Kaohsiung Medical University (MOHW112-TDU-B-221-124007, MOST111-2314-B-037-069-MY2) 2. Kaohsiung Medical University Hospital (KMUH111-1R04, KMUH110-0M03).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design, material preparation, and data collection. The first draft of the manuscript was written by Chin-I Shih. Ming-Lung Yu critically reviewed and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Ming-Lung Yu has received research support from Abbvie, Abbott, BMS, Gilead, Merck, and Roche diagnostics; served as a consultant of Abbvie, Abbott, BMS, Gilead, Merck, Novartis, Roche, and Roche diagnostics; and served as a speaker of Abbvie, Abbott, BMS, Gilead, Merck, Roche, and Roche diagnostics. Chin-I Shih, Kuan-Ta Wu, Meng-Hsuan Hsieh, Jeng-Fu Yang, Yi-Yu Chen, Wei-Lun Tsai, Wen-Chi Chen, Po-Cheng Liang, Yu-Ju Wei, Pei-Chien Tsai, Po-Yao Hsu, Ming-Yen Hsieh, Yi-Hung Lin, Tyng-Yuan Jang, Chih-Wen Wang, Ming-Lun Yeh, Chung-Feng Huang, Jee-Fu Huang, Chia-Yen Dai, Chi-Kung Ho, Wan-Long Chuang declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of KMUH.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shih, CI., Wu, KT., Hsieh, MH. et al. Severity of fatty liver is highly correlated with the risk of hypertension and diabetes: a cross-sectional and longitudinal cohort study. Hepatol Int 18, 138–154 (2024). https://doi.org/10.1007/s12072-023-10576-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10576-z