Abstract
Ascites represents the most common decompensating event in patients with liver cirrhosis. The appearance of ascites is strongly related to portal hypertension, which leads to splanchnic arterial vasodilation, reduction of the effective circulating volume, activation of endogenous vasoconstrictor systems, and avid sodium and water retention in the kidneys. Bacterial translocation further worsens hemodynamic alterations of patients with cirrhosis and ascites. The first-line treatment of uncomplicated ascites is a moderate sodium-restricted diet combined with diuretic treatment. In patients who develop refractory ascites, paracentesis plus albumin represents the most feasible option. Transjugular intrahepatic portosystemic shunt placement is a good alternative for selected patients. Other treatments such as vasoconstrictors and automated low-flow pumps are two potential options still under investigations. Ascites is associated with a high risk of developing further complications of cirrhosis such as dilutional hyponatremia, spontaneous bacterial peritonitis and/or other bacterial infections and acute kidney injury (AKI). Hepatorenal syndrome (HRS) is the most life-threatening type of AKI in patients with cirrhosis. The most appropriate medical treatment in patients with AKI-HRS is the administration of vasoconstrictors plus albumin. Finally, ascites impairs both the quality of life and survival in patients with cirrhosis. Thus, all patients with ascites should be evaluated for the eligibility for liver transplantation. The aim of this article is to review the management of patients with cirrhosis, ascites and HRS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
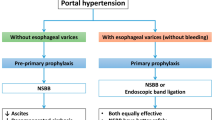
Patients with liver cirrhosis and portal hypertension may develop several complications such as ascites, gastrointestinal bleeding, and hepatic and/or hepatic encephalopathy. Ascites is defined by the appearance of fluid in the peritoneal cavity and is the most common complication of cirrhosis, with an incidence of 60% within 10 years [1].
Pathophysiology of ascites
For several years, splanchnic arterial vasodilation has been considered the main determinant of the avid water and sodium retention observed in patients with cirrhosis and ascites [2]. In particular, it has been observed that portal hypertension may cause the release of vasodilators in the splanchnic circulation such as nitric oxide, carbon monoxide, etc., which can cause a relevant vasodilation. It results in a reduction of the effective circulating volume (ECV) and activation of baroreceptors with the activation of the sympathetic nervous system (SNS), renin-angiotensin-aldosterone system (RAAS) and non-osmotic secretion of vasopressin. These mechanisms increase cardiac output and cause water and sodium retention to compensate for the reduction of ECV. With the progression of liver disease, portal hypertension and splanchnic arterial vasodilation, the heart is not able to compensate for the further reduction in ECV, and the further activation of RAAS increases the renal reabsorption of sodium and water, causing the appearance of ascites [3]. In addition, the hyperactivation of the SNS causes an increase in the proximal tubular absorption of sodium and water in the nephrons [4]. More recently, the role of pathological translocation of bacteria or bacterial products from the gut to the systemic circulation has been highlighted in determining the systemic abnormalities observed in patients with cirrhosis [5]. In fact, the pathogen-associated molecular patterns (PAMPs) stimulate the release of pro-inflammatory cytokines leading to inflammation and further release of NO and CO, thus increasing splanchnic arterial vasodilation [6, 7]. In addition, PAMPs may induce cardiomyocyte dysfunction with a consequent reduction in cardiac output [8].
Clinical impact of ascites
Ascites is associated with a high incidence of further complications of cirrhosis. In fact, patients with ascites have a high risk of developing dilutional hyponatremia, bacterial infections and acute kidney injury (AKI) [9, 10]. Furthermore, patients with cirrhosis and ascites may develop a peculiar type of infection, namely spontaneous bacterial peritonitis (SBP), and a specific type of AKI, namely hepatorenal syndrome (HRS). Following a bacterial infection and/or an episode of gastrointestinal bleeding, ascites confers a higher risk of developing AKI and a worse survival [10, 11]. Most importantly, ascites is associated with a reduction in both the quantity and the quality of life in patients with cirrhosis [12, 13]. In more detail, the probability of survival after the appearance of ascites is 85 and 57% at 1 and 5 years, respectively [9].
Classification and management of ascites
Ascites can be classified into complicated and uncomplicated ascites. Uncomplicated ascites is defined as not associated with hyponatremia, refractoriness to diuretic treatment, acute kidney injury and SBP [13]. In addition, ascites can be quantified in three grades according to its amount in the peritoneal cavity: (1) mild ascites only detectable by ultrasound; (2) moderate ascites with symmetrical distension of the abdomen; (3) tense ascites. The first step in the management of ascites is to collect a detailed medical history and to perform liver and renal blood tests and an abdominal ultrasound. A paracentesis should be performed in all patients with first onset of grade 2/3 ascites and/or acutely decompensated. Peritoneal fluid analysis can provide relevant information such as the confirmation of ascites as a consequence of portal hypertension [serum albumin ascites gradient (SAAG) ≥1.1 g/dl], the presence/absence of an SBP (neutrophil cell count >250 cells/µl) and the risk of developing SBP during follow-up (total protein content <1.5 g/dl) [14, 15]. Before discussing the specific treatment of complicated and uncomplicated ascites, it should be highlighted that the most important issue in the management of patients with cirrhosis is the treatment of the underlying cause of liver disease. In fact, several data suggest that the antiviral treatment of HBV and HCV and/or alcohol abstinence may lead to a progressive improvement of liver function with the potential resolution of ascites.
The measurement of urinary sodium excretion may be a helpful parameter; however the 24-h urine sodium excretion analysis is not always feasible in outpatients. In this case urinary spot sodium may be helpful if very low (0 mmol/l) or very high (>100 mmol/l) [12]. A random ‘spot’ urine sodium concentration greater than the potassium concentration correlates better with a 24-h sodium excretion analysis. The higher the ratio is, the greater the urine sodium excretion [12].
Uncomplicated ascites
The treatment of uncomplicated ascites should be adapted to the ascites grade (Fig. 1). The natural history and clinical impact of grade 1 ascites have not been extensively investigated and no specific treatment has been suggested for these patients. The aim of treatment of moderate ascites is to induce a negative sodium balance by means of (1) a moderate restriction in salt intake and (2) diuretic use to increase renal sodium excretion.
Sodium restriction
Although there is no clear evidence of the efficacy of low sodium intake in the management of ascites in cirrhosis, the current guidelines suggest a moderate restriction of dietary salt (80–120 mmol of sodium/day, equivalent to approximately 4.6–6.9 g of salt/day) [13]. A lower sodium intake has no further benefit for the sodium balance and may be associated with a lower caloric intake [16].
Diuretics
The increased release of aldosterone is considered the main factor responsible for the increased reabsorption of sodium in the kidneys of patients with cirrhosis and ascites [17]. The administration of aldosterone antagonists to cirrhotic patients with ascites is more effective than loop diuretics or other potassium-sparing diuretics [18, 19]. Aldosterone antagonists should be administered starting from 100 to 200 mg/day. A stepwise increase of aldosterone antagonist doses (up to 400 mg/day) may be effective in mobilising ascites in 60–80% of nonazotemic cirrhotic patients with ascites [20, 21]. However, a sequential increase of aldosterone antagonists requires a long time to find the effective dose, given the latency of action of aldosterone. A combined diuretic treatment has been proposed with the administration of 40 mg/day of furosemide and 100–200 mg/day of an aldosterone antagonist. In a randomised controlled trial (RCT) the combined diuretic therapy was effective in a shorter period of time and safer than the sequential diuretic therapy [22]. The aim of diuretic treatment is to achieve a reduction in body weight of more than 1 kg per week of treatment until the ascites is adequately controlled [13]. Weight loss should be <500 g per day in patients without peripheral edema and 1 kg per day in those with peripheral edema to avoid complications of diuretic treatment such as AKI or hyponatremia [13]. Diuretic overdose may precipitate hepatic encephalopathy or cause muscle cramps. Thus, diuretics are contraindicated in patients with overt hepatic encephalopathy, AKI, severe hyponatremia (sodium <120 mmol/l) or incapacitating muscle cramps.
Large and tense ascites
In patients with large and tense ascites the first-line treatment should be therapeutic paracentesis combined with the infusion of albumin because it has been shown to be more effective than the standard diuretic treatment [23]. In addition, side effects such as hyponatremia, AKI and hepatic encephalopathy are significantly lower with paracentesis than with diuretic treatment. The mobilisation of ascites can be completed in one single tap. After large volume paracentesis there is a significant alteration of the systemic circulation such as an acute increase of cardiac output and a reduction in the systemic vascular resistance and arterial blood pressure [24, 25]. These alterations led the experts to define post-paracentesis-induced circulatory dysfunction (PICD), a condition characterised by a ≥50% increase of plasma renin activity 1 week after the procedure [25]. PICD is a relevant complication, being associated with a rapid recurrence of ascites, a high incidence of HRS, dilutional hyponatremia and death [26]. PICD can be prevented by plasma volume expansion. The administration of human albumin, at the dose of 8 g/l of ascites removed, is the most effective measure to prevent PICD and to reduce the mortality rate in patients with ascites [27] and it has been shown to be more effective than other plasma expanders [26]. After a large-volume paracentesis, all patients should immediately receive diuretics, when tolerated, to prevent early recurrence of ascites [13]. Recently, the final results of a randomised controlled trial showed that the long-term administration of albumin (40 g twice a week followed by 40 g per week) was able to reduce the incidence of refractory ascites, hepatorenal syndrome and other complications of cirrhosis and to improve survival in patients with cirrhosis and ascites [28].
Complicated ascites
Patients with complicated ascites represent a very fragile population with a high mortality and a high risk of early readmission after hospitalisation. The management of these patients is complex and the development of new models of specialist care is required to improve the survival and quality of life [29]. The management of complicated ascites is summarised in Table 1.
Refractory ascites
Refractory ascites is defined as “ascites that cannot be mobilised or the early recurrence of which (i.e. after paracentesis) cannot be satisfactorily prevented by sodium restriction and diuretic treatment” [30]. Two different types of RA have been described: diuretic-resistant ascites [that do not respond to dietary sodium restriction and maximal diuretic dose (furosemide 160 mg/day and aldosterone antagonists 400 mg/day)] and diuretic-intractable ascites (caused by the development of diuretic-induced complications) [30]. The latter accounts for more than 90% of patients with refractory ascites [30]. Refractory ascites occurs in 5–10% of patients with cirrhosis and ascites and is associated with a low probability of survival, about 50% at 6 months [31]. The treatment includes large-volume paracenteses with albumin, insertion of a transjugular intrahepatic portosystemic shunt (TIPS), liver transplantation (LT), vasoconstrictors or implantation of automated pumps.
TIPS
The effects of TIPS in patients with refractory ascites have been evaluated in six RCTs [32,33,34,35,36]. The two most recent meta-analyses including the first four studies showed that TIPS was associated with better control of ascites and a higher incidence of hepatic encephalopathy than large-volume paracentesis [37, 38]. Results on survival were conflicting. Saab et al. [37] found no difference in survival. Conversely, Salerno et al. [38] found a benefit in terms of survival in patients treated with TIPS. In the most recent RCT, also including patients with recurrent ascites (not just refractory), TIPS with covered stents improved survival when compared to large-volume paracentesis [36]. Furthermore, patients treated with TIPS had a lower rate of portal hypertension-related bleeding and fewer days of hospitalisation than those treated with large-volume paracentesis [36].
The main limitation to the extensive use of TIPS for the treatment of refractory ascites is the presence of contraindications to TIPS placement, making TIPS use available for less than 40% of patients.
Liver transplantation
LT represents the best treatment of patients with refractory ascites who have a poor survival, even worse that predicted by the MELD score. Thus, in several countries refractory ascites is considered an exception to the MELD score in the allocation of priority in patients with cirrhosis on the waiting list [39]. However, many patients with refractory ascites cannot be considered eligible for LT. Therefore, some patients have contraindications to both TIPS and LT. These patients need some other therapeutic options such as vasoconstrictors or other invasive procedures such as automated pump systems.
Vasoconstrictors
Administration of vasoconstrictors may ameliorate the splanchnic arterial vasodilatation and thereby improve the renal perfusion and filtration. In patients with ascites, a single oral dose of the α1-adrenergic agonist midodrine increases the arterial blood pressure, renal perfusion, glomerular filtration rate (GFR) and sodium excretion [40]. In a small RCT the administration of midodrine was found to be associated with a better control of ascites than standard medical treatment [41]. The administration of terlipressin, a vasopressin-1(V1) receptor agonist, has been shown to be effective in the treatment of refractory ascites in a small pilot study [42]. Recently, terlipressin has been used even in outpatients with cirrhosis and RA by continuous intravenous infusion [43]. However, considering the lack of large prospective studies, and the high risk of adverse events, outpatient administration of terlipressin cannot be recommended.
Automated pump system
The alpha pump is a new device that can be used in the management of refractory ascites. Its principle is to place a pump in the abdominal wall for the automated removal of ascites from the peritoneal cavity into the bladder to be eliminated with the urine. It has been shown to be safe in a small pilot study, pending some measures such as the administration of norfloxacin, abrogation of non-steroidal anti-inflammatory drugs to treat pain after surgery and periprocedural albumin administration [44]. The alpha pump has been recently tested in comparison with therapeutic paracentesis in a randomised clinical trial [45]. Preliminary results of this RCT are promising; in particular, the alpha pump results in a reduction of the need for paracentesis without relevant side effects. However, it should be highlighted that some technical issues were still observed and no effect on survival was found [45].
Hyponatremia
Hypervolemic hyponatremia, defined as a serum sodium concentration <135 mmol/l, occurs in 49% of patients with cirrhosis and ascites [46].
Hypervolemic hyponatremia is the consequence of an abnormal increase in water retention that occurs because of (1) the non-osmotic production of arginine vasopressin (AVP), (2) a decrease in the delivery of pre-urine to the ascending limb of the loop of Henle (the diluting segment of the nephron) and (3) the reduced production of prostaglandins [47, 48].
hyponatremia has a relevant clinical impact in patients with decompensated cirrhosis since it may precipitate hepatic encephalopathy by inducing swelling of the astrocytes [49]. Hyponatremia was found to be a major risk factor for the development of overt encephalopathy in patients with cirrhosis and ascites [50]. Hyponatremia is also a relevant prognostic factor, being associated with poor survival [51, 52]. Thus, serum sodium has been incorporated in the MELD score for use in the priority allocation of LT candidates [52]. Finally, hyponatremia was found to be an independent predictive factor of impaired quality of life in patients with cirrhosis and ascites [53].
Management of hyponatremia
The aim of treatment of hypervolemic hyponatremia is to improve the free water excretion with the urine. The administration of hypertonic sodium chloride cannot be recommended since it would further increase ascites and edema. The current available treatments for hypervolemic hyponatremia in cirrhosis include: (1) fluid restriction, (2) albumin and (3) antagonists of AVP V2 receptors (vaptans). Fluid restriction to about 1 l per day has been suggested for these patients but its efficacy is poor [13]. Some reports suggest that albumin may increase the serum sodium concentration in patients with cirrhosis and ascites by increasing the effective circulating volume [54, 55]. Vaptans increase renal solute-free water excretion through the inhibition of the V2 receptors in the collecting ducts. Satavaptan and tolvaptan were investigated in the treatment of hypervolemic hyponatremia in cirrhotic patients [56,57,58,59]. Satavaptan was more effective than placebo in increasing the serum sodium concentration, but control of ascites was not improved [56] and it was associated with high mortality rates. Hence, the development of satavaptan was abandoned.
Tolvaptan was more effective than placebo in treating hyponatremia in patients with cirrhosis and ascites [58]. However, after the withdrawal of tolvaptan the serum sodium concentration reverted almost to the baseline values [58] and tolvaptan showed poor efficacy in the treatment of patients with cirrhosis and severe hyponatremia (<125 mEq/l) [60]. Nevertheless, the Food and Drug Administration (FDA) raised an alert about the risk of hepatotoxicity related to tolvaptan administration. Thus, nowadays the role of vaptans in the management of hyponatremia in cirrhosis is still uncertain.
Spontaneous bacterial peritonitis
SBP is defined a bacterial infection of ascitic fluid without any intra-abdominal, surgically treatable source of infection [15]. The prevalence of SBP is about 20% in hospitalised patients with cirrhosis and ascites [10, 15]. The pathogenesis of SBP includes both a pathological bacterial translocation from the gut to the systemic circulation and an impaired ability of the local and systemic immunity to control the spread of these bacteria [61]. Bacterial translocation occurs because of (1) an increased intestinal permeability, (2) an intestinal bacterial overgrowth, (3) a change in the quality of bacteria and (4) the ineffective activity of the intestinal immune system [61]. SBP is associated with a high risk of AKI [62] and poor short-term survival and should be identified and treated as soon as possible [15]. SBP is diagnosed when neutrophils in ascitic fluid are >250 cells/µl [15].
Management of SBP: antibiotic treatment
Antibiotic treatment should be administered as soon as possible in patients with SBP, since any delay in the administration of an effective treatment impairs survival in these patients [63]. Third-generation cephalosporins represent the optimal treatment in patients with community-acquired SBP, being effective in more than 80% of patients [64, 65]. The combination of beta-lactams plus beta-lactamases inhibitors showed a similar efficacy [66]. In hospital-acquired episodes of SBP, the efficacy of the above-mentioned antibiotics is poor, because those episodes are frequently sustained by multi-drug-resistant (MDR) bacteria [65, 67]. In hospital-acquired SBP a broader spectrum empirical antibiotic treatment should be used according to local epidemiology [68]. In RCT in an Italian centre with a high prevalence of MDR, the combination of meropenem plus daptomycin was shown to be more effective than ceftazidime [67]. In addition, the administration of an effective empirical treatment was an independent predictor of survival [67]. If a broad-spectrum antibiotic treatment is administered, it should be narrowed when culture results are available to minimise the risk of further antibiotic resistance.
Management of SBP: prevention of acute kidney injury
As reported above, patients with SBP have a high risk of developing AKI, which is associated with poor survival [10, 62]. In RCT, the administration of albumin (1.5 g/kg of body weight on day 1 and 1 g/kg of body weight on day 3) has been shown to reduce the incidence of AKI and improve survival in patients with SBP [69]. Albumin infusion exerts a positive effect in these patients beyond the plasma volume expansion. In fact, in RCT albumin, but not hydroxyethyl starch, improved the cardiac stroke work index and systemic vascular resistance in patients with SBP [70]. These effects may be due to the non-oncotic properties of albumin. Indeed, in cirrhotic rats, albumin exerted a positive cardiac inotropic effect, mainly counteracting oxidative stress- and TNF-α-induced activation of the NF-κB and iNOS pathway [71]. In addition, albumin in patients with cirrhosis is not only reduced in quantity, but also the quality and function are impaired because of oxidative stress and post-transcriptional changes. Thus, the positive effects of albumin administration may also be related to the replacement of dysfunctional albumin with exogenous administration [72].
Prophylaxis of SBP
The probability of SBP recurrence is about 70% at 1 year [73]. In these patients, secondary prophylaxis with norfloxacin was shown to be effective in preventing the recurrence of SBP [73]. Currently, primary prophylaxis of SBP is recommended in two conditions: (1) after episodes of gastrointestinal bleeding and (2) in patients with a protein concentration in ascitic fluid below 1.5 g/dl and advanced liver disease (Child-Pugh ≥9 and bilirubin ≥3 mg/dl or serum creatinine ≥1.2 mg/dl or serum sodium ≤130 mmol/l). Norfloxacin is effective in preventing SBP after an episode of gastrointestinal bleeding [74]; however in patients with gastrointestinal bleeding and severe cirrhosis (at least two of the following: ascites, severe malnutrition, encephalopathy or bilirubin >3 mg/dl) ceftriaxone was shown to be more effective than norfloxacin in preventing bacterial infections [75]. The latter findings were probably also related to the progressive increase in resistance to quinolones observed in the last 2 decades [65]. In RCT norfloxacin significantly reduced the incidence of SBP and HRS and improved survival in patients with cirrhosis, protein concentration in ascites <1.5 g/dl and advanced liver disease (see above) when compared to placebo [76].
Hepatorenal syndrome
Renal dysfunction is a severe complication of advanced cirrhosis as well as of acute-on-chronic liver failure (ACLF). Traditionally renal dysfunction in patients with liver disease has been defined as a serum creatinine (sCr) ≥1.5 mg/dl [29, 77] while AKI has been defined as a percent increase of sCr 50% to a final value >1.5 mg/dl [22, 26, 69, 78]. In patients with cirrhosis AKI can have different clinical and pathophysiological features such as prerenal, intrinsic, HRS and post-renal AKI [79]. HRS has been defined as a syndrome that occurs in patients with advanced liver disease, characterised by impaired renal function and marked abnormalities in the arterial circulation and over-activity of the endogenous vasoactive systems. In the kidney, there is marked renal vasoconstriction that results in a low GFR. In the extrarenal circulation there is a predominance of arterial vasodilation that results in the reduction of systemic vascular resistance and arterial hypotension [29, 77]. HRS has been classified into two different clinical types: type-1 HRS, characterised by a rapidly progressive reduction of renal function, defined by a doubling of the serum creatinine to a level >2.5 mg/dl in less than 2 weeks, and type-II HRS, in which the renal failure does not have a rapidly progressive course [29, 77]. During the last few years, a new syndrome has been described, ACLF [80]; new relevant data have emerged on the nature and pathophysiology [81, 82] of AKI as well as on the nature of HRS [83]. In addition, new KDIGO criteria have been introduced for the definition of AKI in patients with cirrhosis [84]. Accordingly, the classification, pathophysiology and management of HRS need to be updated.
Pathophysiology of HRS
The pathophysiology of HRS involves both macrovascular dysfunction and systemic inflammation (Fig. 2). Systemic inflammation is due to pathological bacterial translocation, which is the main mechanism by which portal hypertension induces macrocirculatory dysfunction [5]. Following bacterial translocation, PAMPs are recognised by monocytes through the pattern recognition receptors. The consequent activation of the monocytes results in the release of pro-inflammatory cytokines such as tumor necrosis factor-α, interleukin-6 and interleukin-1-β. The release of these pro-inflammatory cytokines has been found to be associated with impairment of the renal function in patients with SBP as well as the development of renal failure in patients with ACLF [85, 86]. Patients with HRS-AKI frequently show failure of organs other than the kidney [80]. Multiple organ failure cannot be explained by macrovascular dysfunction and suggests that also kidney damage may occur through mechanisms other than severe renal arterial vasoconstriction. Such confirming clinical [81] and experimental studies [82] performed in cirrhosis and superimposed infection/inflammation have shown an up-regulation of renal tubular TLR4 associated with the development of renal tubular damage and apoptosis. Although the mechanism of up-regulation of tubular TLR4 is not entirely clear, it seems likely to be a consequence of bacterial translocation [61, 81]. Significant tubular damage was detected in rats with cirrhosis following the administration of a sub-lethal dose of lipopolysaccharide (LPS) [82]. Stretching this concept, the pathophysiology of AKI in the presence of a high degree of inflammation seems to deviate from that traditionally theorised for HRS. Recently, a new hypothesis on the pathogenesis of sepsis-induced AKI has been proposed [87]. Accordingly, the interplay of inflammation and microvascular dysfunction characterises and amplifies this signal that PAMPs and DAMPs exert on some epithelial cells of the proximal tubules. The recognition of this signal and its spread to other epithelial cells of the proximal tubule, a mitochondria-mediated metabolic down-regulation and reprioritisation of cell functions favour survival processes at the expense of other functions such as the absorption of sodium and chloride on the lumen side. The consequent increases of NaCl delivery to the macula densa trigger the further intrarenal activation of the renin-angiotensin system, causing a fall in GFR. Finally, a severe cholestasis may further impair renal function by worsening the inflammation and/or macrovascular dysfunction or by promoting bile salt-related direct tubular damage. All these features can develop even in the absence of macrovascular dysfunction and thus of renal hypoperfusion (Fig. 2) [88]. These new concepts have relevant implications for clinical practice. In fact, the current treatment of HRS (i.e. vasoconstrictors plus albumin) is mainly focussed on circulatory dysfunction. However, recent data suggest that when inflammation increases, as observed in more advanced grades of ACLF [86], the efficacy of vasoconstrictors plus albumin decreases regardless of the baseline values of sCr [89].
Diagnosis and management of HRS
Patients with cirrhosis and AKI should be managed according to the International Club of Ascites recommendations (Fig. 3) [84]. The first measure is to minimise or to stop any potential nephrotoxic drug (i.e., diuretics, antibiotics, NSAIDs, angiotensin-converting enzyme inhibitors, etc.). Then, it is important to verify the presence of hypovolemia and, if present, to correct it. In patients with AKI stage ≥2 (increase of serum creatinine ≥2-fold from baseline) diuretics should be withdrawn and plasma expansion with albumin (1 g/kg of body weight for 2 days) should be administered. In patients without a response to albumin expansion the main differential diagnosis is between HRS and acute tubular necrosis (ATN). Thus, the HRS criteria should be investigated (Table 2). Briefly, if there has been no recent use of nephrotoxic drugs, no hematuria, no significant proteinuria, no shock and no alterations of renal ultrasonography, the diagnosis is HRS. It should be highlighted that these criteria are not able to rule out a mild parenchymal renal damage that may be present in patients with HRS. Urinary biomarkers of tubular damage may improve the differential diagnosis of AKI. Indeed, urinary neutrophil gelatinase-associated lipocalin (NGAL) was found to be increased in patients with cirrhosis and ATN versus patients with HRS [90]. Other urinary biomarkers such as liver fatty acid-binding protein, kidney injury molecule-1 and interleukin-18 were found to be significantly increased in patients with ATN versus patients with HRS; however their accuracy was lower than NGAL, but their combination significantly increased the diagnostic accuracy [91]. In future, these biomarkers may be used in the differential diagnosis of AKI.

*Modified from Ref. [81]
Management of acute kidney injury in cirrhosis*. AKI acute kidney injury, NSAIDs non-steroidal anti-inflammatory drugs, HRS hepatorenal syndrome
In Fig. 4 targets of treatment of HRS have been reported. LT is the best treatment both for type-1 and type-2 HRS [92, 93]. Unfortunately, not all patients are eligible for LT. Thus, medical treatments have been developed in the last 15 years, the most effective being the combination of vasoconstrictors plus albumin. The rationale behind the use of vasoconstrictors is to counteract splanchnic arterial vasodilation. Albumin counteracts the reduction in effective circulating volume and improves cardiac contractility [72]. Three types of vasoconstrictors are currently available. Among them, terlipressin is the most widely used, while α-adrenergic drugs have been claimed to be a potential alternative. Among α-adrenergic drugs, midodrine given orally (2.5 up to 12.5 qid) together with octreotide given subcutaneously (125 up to 250 μgr bid) [94] or norepinephrine given by continuous intravenous infusion (0.1–1 mg per hour) [95, 96] has been used. Recently, terlipressin was shown to be superior to midodrine plus octreotide in the treatment of type-1 HRS [97]. Regarding norepinephrine, two small RCTs in patients with type-1 HRS showed that it is as effective as terlipressin in terms of reversal of HRS and 1-month survival [95, 96]. In the last two randomised RCTs using terlipressin plus albumin, the percentage of patients who showed a resolution of HRS was 56% [97, 98]. Regarding the administration route of terlipressin in patients with HRS, it has been recently shown that the continuous intravenous infusion of terlipressin moving from the initial dose of 2 mg/day is the most suitable since it is associated with a lower rate of adverse effects than the administration by intravenous boluses [98]. Albumin should be administered at a dose of 20–40 g/day [97, 98]. The treatment with vasoconstrictors plus albumin should be continued until sCr reaches a value below 1.5 mg/dl. The dose and timing of treatment for HRS are summarised in Table 3. About 20% of patients may present a recurrence of HRS after treatment withdrawal, and retreatment is usually effective. Some patients may show a continuous recurrence of HRS at any attempt to discontinue terlipressin. For these patients, a high priority on the LT waiting list [99] and/or outpatient infusion [100] has been suggested. The use of TIPS is a potential treatment because it reduces portal hypertension and increases cardiac output. TIPS improves renal perfusion, sodium and water excretion and has been reported to reduce sCr in selected patients with HRS [101, 102]. However, data available on the use of TIPS in patients with type-1 HRS are mainly based on case series and RCTs are needed to evaluate the use of TIPS in these patients. Too few data are available on the role of renal replacement therapy (RRT) in patients with HRS. No survival advantage has been demonstrated in patients with HRS treated with RRT. However, in patients not responding to vasoconstrictors plus albumin, RRT may be indicated in case of volume overload and/or metabolic acidosis and/or hyperkalemia and/or hepatic encephalopathy refractory to the standard medical treatment [103], in particular in patients on the LT waiting list. No data are available regarding the optimal technique of RRT (intermittent hemodialysis vs. continuous RRT) in these patients. However, continuous RRT may be the best option considering the lower risk of hypotension than intermittent hemodialysis. In patients who are not eligible for LT the decision to perform RRT should be made case by case to avoid futility of treatment.
Finally in non-responders to the medical treatment who are candidates for LT, a simultaneous kidney-liver transplantation (SKL) should be considered in one of the following conditions: (1) persistent AKI for ≥4 weeks with one of the following: stage 3 AKI as defined by KDIGO, sCr ≥4.0 mg/dl with an acute increase of ≥0.5 mg/dl or on renal replacement therapy, persistent AKI with an estimated GFR ≤35 ml/min (MDRD-6 equation) or GFR ≤25 ml/min (iothalamate clearance) for ≥4 weeks [104].
Abbreviations
- AKI:
-
Acute kidney injury
- HRS:
-
Hepatorenal syndrome
- ECV:
-
Effective circulating volume
- SNS:
-
Sympathetic nervous system
- RAAS:
-
Renin angiotensin aldosterone system
- PAMPs:
-
Pathogen-associated molecular patterns
- NO:
-
Nitric oxide
- CO:
-
Carbon monoxide
- SBP:
-
Spontaneous bacterial peritonitis
- SAAG:
-
Serum albumin ascites gradient
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- RCT:
-
Randomized controlled trial
- PICD:
-
Paracentesis induced circulatory dysfunction
- TIPS:
-
Transjugular intrahepatic portosystemic shunt
- LT:
-
Liver transplantation
- MELD:
-
Model of end stage liver disease
- GFR:
-
Glomerular filtration rate
- AVP:
-
Arginine vasopressin
- FDA:
-
Food and Drug Administration
- MDR:
-
Multi-drug resistant
- TNF-α:
-
Tumor necrosis factor alpha
- iNOS:
-
Inducible nitric oxide synthase
- ACLF:
-
Acute on chronic liver failure
- sCr:
-
Serum creatinine
- TLR4:
-
Toll like receptor 4
- LPS:
-
Lipopolysaccharide
- DAMPs:
-
Danger associated molecular patterns
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- ATN:
-
Acute tubular necrosis
- NGAL:
-
Neutrophil gelatinase-associated lipocalin
- RRT:
-
Renal replacement therapy
- SKL:
-
Simultaneous kidney liver transplantation
- KDIGO:
-
Kidney disease improving global outcomes
References
Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987;7:122–128
Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arteriolar vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 1988;8:151–1157
Arroyo V, Terra C, Ginès P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. J Hepatol 2007;46:935–946
Angeli P, Gatta A, Caregaro L et al. Tubular site of renal sodium retention in ascitic liver cirrhosis evaluated by lithium clearance. Eur J Clin Invest 1990;20:111–117
Bernardi M, Moreau R, Angeli P et al. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J Hepatol 2015;63:1272–1284
Tazi KA, Moreau R, Hervé P, et al. Norfloxacin reduces aortic NO synthases and proinflammatory cytokine up-regulation in cirrhotic rats: role of Akt signaling. Gastroenterology 2005;129:303–314
Angeli P, Fernández-Varo G, Dalla Libera V, et al. The role of nitric oxide in the pathogenesis of systemic and splanchnic vasodilation in cirrhotic rats before and after the onset of ascites. Liver Int 2005;25:429–437
Yang YY, Liu H, Nam SW et al. Mechanisms of TNFalpha-induced cardiac dysfunction in cholestatic bile duct-ligated mice: interaction between TNFalpha and endocannabinoids. J Hepatol 2010;53:298–306
Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol 2006;4:1385–1394
Fasolato S, Angeli P, Dallagnese L et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology 2007;45:223–229
Cárdenas A, Ginès P, Uriz J, et al. Renal failure after upper gastrointestinal bleeding in cirrhosis: incidence, clinical course, predictive factors, and short-term prognosis. Hepatology 2001;34:671–676
Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009; 50: 2087–2107
Ginès P, Angeli P, Lenz K, et al. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol 2010;53:397–417
Runyon BA, Montano AA, Akriviadis EA, et al. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med 1992;117:215–220
Rimola A, Garcia-Tsao G, Navasa M, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol 2000;32:142–153
Morando F, Rosi S, Gola E, et al. Adherence to a moderate sodium restriction diet in outpatients with cirrhosis and ascites: a real-life cross-sectional study. Liver Int 2015;35:1508–1515
Bernardi M, Servadei D, Trevisani F, et al. Importance of plasma aldosterone concentration on natriuretic effect of spironolactone in patients with liver cirrhosis and ascites. Digestion 1985;31:189–193
Pérez-Ayuso RM, Arroyo V, Planas R, et al. Randomized comparative study of efficacy of furosemide versus spironolactone in nonazotemic cirrhosis with ascites. Gastroenterology 1984;84:961–968
Angeli P, Dalla Pria M, De Bei E, et al. Randomized clinical study of the efficacy of amiloride and potassium canrenoate in nonazotemic cirrhotic patients with ascites. Hepatology 1994;19:72–79
Gatta A, Angeli P, Caregaro L, et al. A pathophysiological interpretation of unresponsiveness to spironolactone in a stepped-care approach to the diuretic treatment of ascites in nonazotemic cirrhotic patients with ascites. Hepatology 1991;14:231–236
Santos J, Planas R, Pardo A, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol 2003;39:187–192
Angeli P, Fasolato S, Mazza E, et al. Combined versus sequential diuretic treatment of ascites in non-azotemic patients with cirrhosis: results of an open randomised clinical trial. Gut 2010;59:98–104
Gines P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology 1987;92:234–241
Simon DM, McCain JR, Bonkovsky HL, et al. Effects of therapeutic paracentesis on systemic and hepatic hemodynamics and on renal and hormonal function. Hepatology 1987;7:423–429
Ruiz del Arbol L, Monescillo A, Jimenez W, et al. Paracentesis-induced circulatory dysfunction: mechanism and effect on hepatic hemodynamics in cirrhosis. Gastroenterology 1997;113:579–586
Gines A, Fernandez-Esparrach G, Monescillo A, et al. Randomized controlled trial comparing albumin, dextran-70 and polygelin in cirrhotic patients with ascites treated by paracentesis. Gastroenterology 1996;111:1002–1010
Bernardi M, Caraceni P, Navickis RJ, et al. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology 2012; 55:1172–1181
Caraceni P, Riggio O, Angeli P, et al. Long-term albumin administration improves survival in patients with decompensated cirrhosis: final results of the “ANSWER” study. J Hepatol 2017;66:S93 (abstract)
Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol 2013;59:257–264
Arroyo V, Gines P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology 1996;23:164–176
Moreau R, Delegue P, Pessione F, et al. Clinical characteristics and outcome of patients with cirrhosis and refractory ascites. Liver Int 2004;24:457–464
Lebrec D, Giuily N, Hadengue A, et al. Transjugular intrahepatic portosystemic shunts: comparison with paracentesis in patients with cirrhosis and refractory ascites: a randomized trial. J Hepatol 1996;25:135–44
Rössle M, Ochs A, Gülberg V, et al. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med 2000;342:1701–1707
Gines P, Uriz J, Calahorra B, et al. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology 2002;123:1839–1847
Salerno F, Merli M, Riggio O, et al. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 2004;40:629–635
Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology 2017;152:157–163
Saab S, Nieto JM, Lewis SK, et al. TIPS versus paracentesis for cirrhotic patients with refractory ascites. Cochrane Database Syst Rev 2006; CD004889
Salerno F, Camma C, Enea M, et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology 2007;133:825–834
Cillo U, Burra P, Mazzaferro V, et al. A multistep, consensus-based approach to organ allocation in liver transplantation: toward a “Blended Principle Model”. Am J Transplant 2015;15:2552–2561
Angeli P, Volpin R, Piovan D, et al. Acute effects of the oral administration of midodrine, an alpha-adrenergic agonist, on renal hemodynamics and renal function in cirrhotic patients with ascites. Hepatology 1998;28:937–943
Singh V, Dhungana SP, Singh B, et al. Midodrine in patients with cirrhosis and refractory or recurrent ascites: a randomized pilot study. J Hepatol 2012;56:348–354
Fimiani B, Guardia DD, Puoti C, et al. The use of terlipressin in cirrhotic patients with refractory ascites and normal renal function: a multicentric study. Eur J Intern Med 2011;22:587–590
Gow PJ, Ardalan ZS, Vasudevan A, et al. Outpatient terlipressin infusion for the treatment of refractory ascites. Am J Gastroenterol 2016;111:1041–1042
Bellot P, Welker MW, Soriano G, et al. Automated low flow pump system for the treatment of refractory ascites: a multi-center safety and efficacy study. J Hepatol 2013;58:922–927
Adebayo D, Bureau C, De Rieu MC, et al. Alphapump system versus large volume paracentesis in the treatment of refractory ascites; results from a multicentre randomised controlled clinical study. J Hepatol 2016;64:(Suppl. 2) S185 (abstract)
Angeli P, Wong F, Watson H, et al. Hyponatremia in cirrhosis: results of a survey. Hepatology 2006;44:1535–1542
Porcel A, Diaz F, Rendom P, et al. Dilutional hyponatremia in patients with cirrhosis and ascites. Arch Intern Med 2002;162:323–328
Ginès P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology 2008;48:1002–1010
Restuccia T, Gomez-Anson B, Guevara M, et al. Effects of dilutional hyponatremia on brain organic osmolytes and water content in patients with cirrhosis. Hepatology 2004:39;1613–1622
Guevara M, Baccaro ME, Torre A, et al. Hyponatremia is a risk factor of hepatic encephalopathy in patients with cirrhosis: a prospective study with time dependent analysis. Am J Gastroenterol 2009;1004:1382–1389
Arroyo V, Rodes J, Gutierrez-Lizarraga MA. Prognostic value of spontaneous hyponatremia in cirrhosis with ascites. Dig Dis 1976;21:249–256
Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med 2008;359:1018–1026
Solà E, Watson H, Graupera I, et al. Factors related to quality of life in patients with cirrhosis and ascites: relevance of serum sodium concentration and leg edema. J Hepatol 2012;57:1199–1206
McCormick PA, Mistry P, Kaye G, et al. Intravenous albumin infusion is an effective therapy for hyponatremia in cirrhotic patients with ascites. Gut 1990;31:204–207
Minhtri K, Nguyen MK, Ornekian V, Kao L, Butch AW, Kurtz I. Defining the role of albumin infusion in cirrhosis-associated hyponatremia. Am J Physiol 2014;307:G229–G232
Wong F, Watson H, Gerbes A, et al. Satavaptan for the management of ascites in cirrhosis: efficacy and safety across the spectrum of ascites severity. Gut 2012;61:108–116
Schrier RW, Gross P, Gheorghiade M, et al for the SALT Investigators. Tolvaptan a selective oral vasopressin V2-receptor antagonist, for hyponatremia. New Engl J Med 2006:355–420
Cardenas A, Gines P, Marotta P, et al. Tolvaptan, an oral vasopressin antagonist, in the treatment of hyponatremia in cirrhosis. J Hepatol 2012;56:571–578
Ahluwalia V, Heuman DM, Feldman G, et al. Correction of hyponatremia improves cognition, quality of life, and brain oedema in cirrhosis. J Hepatol 2015;62:75–82
Pose E, Solà E, Piano S, et al. Limited efficacy of tolvaptan in patients with cirrhosis and severe hyponatremia: real-life experience. Am J Med 2017;130:372–375
Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol 2014;60:197–209
Follo A, Llovet JM, Navasa M, et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: course, predictive factors and prognosis. Hepatology 1994;20:1495–1501
Karvellas CJ, Abraldes JG, Arabi YM, et al. Appropriate and timely antimicrobial therapy in cirrhotic patients with spontaneous bacterial peritonitis-associated septic shock: a retrospective cohort study. Aliment Pharmacol Ther 2015;41:747–757
Felisart J, Rimola A, Arroyo V, Perez-Ayuso RM, Quintero E, Gines P, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology 1985;5:457–462
Fernández J, Acevedo J, Castro M, Garcia O, de Lope CR, Roca D, et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology 2012;55:1551–1561
Ricart E, Soriano G, Novella MT, Ortiz J, Sàbat M, Kolle L, et al. Amoxicillin-clavulanic acid versus cefotaxime in the therapy of bacterial infections in cirrhotic patients. J Hepatol 2000;32:596–602
Piano S, Fasolato S, Salinas F, Romano A, Tonon M, Morando F, et al. The empirical antibiotic treatment of nosocomial spontaneous bacterial peritonitis: results of a randomized, controlled clinical trial. Hepatology 2016;63:1299–1309
Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol 2014;60:1310–1324
Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 1999;341:403–409
Fernández J, Monteagudo J, Bargallo X, et al. A randomized unblinded pilot study comparing albumin versus hydroxyethyl starch in spontaneous bacterial peritonitis. Hepatology 2005;42:627–634
Bortoluzzi A, Ceolotto G, Gola E, et al. Positive cardiac inotropic effect of albumin infusion in rodents with cirrhosis and ascites: molecular mechanisms. Hepatology 2013;57:266–276
Arroyo V, García-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. J Hepatol 2014;61:396–407
Gines P, Rimola A, Planas R, et al. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology 1990;12:716–724
Soriano G, Guarner C, Tomas A, et al. Norfloxacin prevents bacterial infection in cirrhotics with gastrointestinal hemorrhage. Gastroenterology 1992;103:1267–1272
Fernández J, Ruiz del Arbol L, Gómez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology 2006;131:1049–1056
Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 2007;133:818–824
Salerno F, Gerbes A, Gines P, et al. Diagnosis, prevention and treatment of the hepatorenal syndrome in cirrhosis a consensus workshop of the International Ascites Club. Gut 2007;56:1310–1318
Piano S, Rosi S, Maresio G, et al. Evaluation of the Acute Kidney Injury Network criteria in hospitalized patients with cirrhosis and ascites. J Hepatol 2013;59:482–489
Moreau R, Lebrec D. Acute renal failure in patients with cirrhosis: perspectives in the age of MELD. Hepatology 2003;37:233–243
Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–1437
Shah N, Mohamed FE, Jover-Cobos M, et al. Increased renal expression and urinary excretion of TLR4 in acute kidney injury associated with cirrhosis. Liver Int 2013;33:398–409
Shah N, Dhar D, El Zahraa Mohammed F, et al. Prevention of acute kidney injury in a rodent model of cirrhosis following selective gut decontamination is associated with reduced renal TLR4 expression. J Hepatol 2012;56:1047–1053
Trawalé JM, Paradis V, Rautou PE, et al. The spectrum of renal lesions in patients with cirrhosis: a clinicopathological study. Liver Int 2010;30:725–732
Angeli P, Gines P, Wong F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. J Hepatol 2015;62:968–974
Navasa M, Follo A, Filella X, et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology 1998;27:1227–1232
Clària J, Stauber RE, Coenraad MJ, et al. CANONIC Study Investigators of the EASL-CLIF Consortium and the European Foundation for the Study of Chronic Liver Failure (EF-CLIF). Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology 2016;64:1249–1264
Gomez H, Ince C, De Backer D, et al. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 2014;41:3–11
Angeli P, Tonon M, Pilutti C, et al. Sepsis-induced acute kidney injury in patients with cirrhosis. Hepatol Int 2016;10:115–123
Piano S, Schmidt HH, Ariza X, et al. Impact of acute-on-chronic liver failure on response to treatment with terlipressin and albumin in patients with type 1 hepatorenal syndrome. J Hepatol 2017;66:S572 (Abstract)
Fagundes C, Pépin MN, Guevara M, et al. Urinary neutrophil gelatinase-associated lipocalin as biomarker in the differential diagnosis of impairment of kidney function in cirrhosis. J Hepatol 2012;57:267–273
Belcher JM, Sanyal AJ, Peixoto AJ, et al. Kidney biomarkers and differential diagnosis of patients with cirrhosis and acute kidney injury. Hepatology 2014;60:622–632
Boyer TD, Sanyal AJ, Garcia-Tsao G, et al. Impact of liver transplantation on the survival of patients treated for hepatorenal syndrome type 1. Liver Transplant 2011;17(11):1328–1332
Angeli P, Gines P. Hepatorenal syndrome, MELD score and liver transplantation: an evolving issue with relevant implications for clinical practice. J Hepatol 2012;57(5):1135–1140
Angeli P, Volpin R, Gerunda G, et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology 1999;29:1690–1697
Singh V, Ghosh S, Singh B, et al. Noradrenaline vs. terlipressin in the treatment of hepatorenal syndrome: a randomized study. J Hepatol 2012;56:1293–1298
Sharma P, Kumar A, Shrama BC, et al. An open label, pilot, randomized controlled trial of noradrenaline versus terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am J Gastroenterol 2008;103:1689–1697
Cavallin M, Kamath PS, Merli M, et al. Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: a randomized trial. Hepatology 2015;62:567–574
Cavallin M, Piano S, Romano A, et al. Terlipressin given by continuous intravenous infusion versus intravenous boluses in the treatment of hepatorenal syndrome: a randomized controlled study. Hepatology 2016;63:983–992
Piano S, Morando F, Fasolato S, et al. Continuous recurrence of type 1 hepatorenal syndrome and long-term treatment with terlipressin and albumin: a new exception to MELD score in the allocation system to liver transplantation? J Hepatol 2011;55:491–496
Vasudevan A, Ardalan Z, Gow P, et al. Efficacy of outpatient continuous terlipressin infusions for hepatorenal syndrome. Hepatology 2016;64:316–318
Wong F, Pantea L, Sniderman K. Midodrine, octreotide, albumin, and TIPS in selected patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 2004;40:55–64
Guevara M, Ginès P, Bandi JC, et al. Transjugular intrahepatic portosystemic shunt in hepatorenal syndrome: effects on renal function and vasoactive systems. Hepatology 1998;28:416–422
Nadim MK, Durand F, Kellum JA, et al. Management of the critically ill patient with cirrhosis: a multidisciplinary perspective. J Hepatol 2016;64:717–735
Nadim MK, Sung RS, Davis CL, et al. Simultaneous liver-kidney transplantation summit: current state and future directions. Am J Transplant 2012;12:2901–2908
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.P. and M.T. have nothing to disclose. P.A.: scientific advisory board of Sequana Medical.
Rights and permissions
About this article
Cite this article
Piano, S., Tonon, M. & Angeli, P. Management of ascites and hepatorenal syndrome. Hepatol Int 12 (Suppl 1), 122–134 (2018). https://doi.org/10.1007/s12072-017-9815-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-017-9815-0