Abstract
Background and aim
Liver biopsy is the gold standard for assessment of fibrosis in patients with hepatitis B. However, it has some disadvantages, including inter-observer and intra-observer variability in biopsy interpretation and specimen variation. A standard biopsy specimen represents only about 0.0002 % of the whole liver. It has been shown that two biopsy samples collected during a procedure have significant influence on the diagnostic performance of interpretation in patients with hepatitis C or non-alcoholic steatohepatitis. Therefore, we aimed to assess the influence of collecting two liver biopsy samples during a single procedure for staging and grading chronic hepatitis B.
Patients and methods
27 patients were included in the study. The median age of the patients was 43.51 ± 11.69. Fifteen patients were female, 12 patients were male. In the biopsy procedure, two samples of liver lobes were obtained. Grade and stage scores were compared between the two samples. Fibrosis staging and grading were assessed according to the Ishak scoring system.
Results
Numbers of portal tract and biopsy size were equal in the two samples. There was a significant difference between the samples in terms of histological activity index (p value = 0.04). However, the difference was not enough to distinguish the mild and moderate stages. On the other hand, no significant difference in fibrosis staging between the two samples was found.
Conclusions
With this relatively small size of patients, in this study, we showed that a proper liver biopsy size is sufficient to predict treatment decisions in chronic hepatitis B patients. However, further studies are needed to show the association of sampling variability in patients with hepatitis B.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B (HBV) infection is an important worldwide health problem, and it infects about 350–400 million people in the world. It is estimated that a million people chronically infected with HBV die of cirrhosis and its complications every year [1]. Therefore, it is most important to stop the development of early-stage fibrosis before the onset of cirrhosis [2].
Although the role of liver biopsy as a diagnostic test in chronic hepatitis B (CHB) has declined, it still has increasing importance in predicting treatment decisions. Currently, the major indication for liver biopsy in CHB is to evaluate the intensity of the disease, especially in respect to both necro-inflammation (grade) and fibrosis (stage) which is quite essential for prognosis and therapeutic management [3].
Liver biopsy is the gold standard for assessment of fibrosis in patients with HBV. However, it has some disadvantages, including inter-observer and intra-observer variability in biopsy interpretation and specimen variation [4]. A standard biopsy specimen represents only about 0.0002 % of the whole liver. It has been shown that two biopsy samples taken during the same procedure have significant influence on the diagnostic performance of interpretation in patients with chronic hepatitis C (CHC) or non-alcoholic steatohepatitis (NASH) [5, 6]. However, no study evaluating the sampling variability for liver biopsy in CHB is available in the literature. Therefore, we aimed to assess the influence of collecting two liver biopsy samples during the same procedure on staging and grading of CHB.
Patients and methods
Twenty-seven patients with CHB were enrolled consecutively into the study between June 2011 and April 2012. Laboratory and clinical data were obtained from our hospital's computerized patient registry database: HBV–DNA level, hepatitis B e-antigen (Hbe-Ag) seropositivity, alanine transaminotransferase (ALT), aspartate transaminotransferase (AST), gamma–glutamyl transpeptidase, alkaline phosphatase, bilirubin, international numeric ratio, white blood cell count, platelet count, hemoglobin. Patients co-infected with other viral hepatitis and HIV or liver transplantation, clinically overt cirrhosis, Wilson disease, hemochromatosis, alcohol abuse, and/or autoimmune or cholestatic liver diseases were excluded from the study.
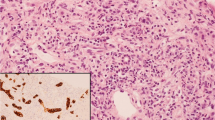
Liver biopsies were performed on treatment-naive CHB patients. Paired liver biopsy samples were obtained from the right and left hepatic lobes using ultrasound guidance with 17-gauge biopsy needles. Samples were fixed with 10-% formalin and embedded in paraffin. The tissue sections were processed with hematoxylin and eosin, Masson’s trichrome, and reticular fiber staining. An expert pathologist of our institution reviewed the biopsy samples. He was also blinded to the two separate biopsy specimens of the same patient to show discrepancy in staging of fibrosis between the two biopsy specimens, if present. The biopsy samples more than 18 mm long or including at least four portal tracts were accepted for pathological evaluation.
The Knodell scoring system, modified by Ishak, was used in evaluating the fibrosis staging and grading. According to the scoring system, the histological activity index (HAI) score was counted from 0 to 18 for minimal to maximal points (periportal or periseptal interface hepatitis, confluent necrosis, focal lytic necrosis, apoptosis and focal inflammation, portal inflammation), and the fibrosis score was counted from 0 to 6 for minimal to maximal points. Minimal/mild/moderate/severe HAI grading scores were defined 1–3/4–8/9–12/13–18, respectively. F0–F1 was termed “no/minimal fibrosis” and F2–F6 was termed ‘‘significant fibrosis’’.
The Statistical Package for Social Sciences (SPSS, Illinois, Chicago) 15.0 for windows was used to analyze the data. The values were reported as mean ± standard deviation (SD). For continuous variables, paired-samples tests were used to analyze the variance among groups, if appropriate. Categorical variables were compared with the Chi square test.
Results
Paired biopsy samples from 27 patients with CHB were evaluated. Median age of the patients was 43.51 ± 11.69. Fifteen patients were female, 12 patients were male. Demographic features and laboratory findings of patient and control groups are reported in Table 1.
All of the patients were HBs Ag positive, anti-HBc Ig G positive, anti-HBe positive and HBV DNA levels were higher than 2000 UI/ml. Serological tests for hepatitis D and hepatitis C were negative in all the patients.
Numbers of portal tract and biopsy size were equal in the two samples (right/left lobe portal tract: 7.92 ± 4.21/6.74 ± 3.73). HAI score in the right/left lobe was 4.85 ± 1.99/4.25 ± 1.85 and the difference was significant (p value = 0.04). 4/27 (14.8 %) patients had 1-point, 2/27 (7.4 %) had 2-point, and 3/27 (11.1 %) had 3-point differences in HAI score between the two samples of the same patient. On the other hand, fibrosis stages in the right/left lobe were 1.74 ± 1.12/1.81 ± 1.24 (p). Neither the difference in grading nor in fibrosis staging between the two samples was significant. 7/27 patients (25.9 %) had a 1-point difference and only 1 patient (3.7 %) had a 2-point difference in liver fibrosis stage between the two samples.
When we evaluated the pre-cirrhotic and cirrhotic patients, two patients had F3 fibrosis, which remained the same after the second examination. Three patients with F4 fibrosis had a one-point discrepancy in fibrosis score. On the other hand, 5/27 patients with either F1 or F2 had a 1-point difference. When we compared patients with F1–F2 fibrosis and patients with F3–F4 fibrosis, the difference in fibrosis score of the two samples was also not significant.
A significant HAI score (Knodell ≥ 8) rate was observed in right lobe biopsy samples (3.7 %, 1/27). On the other hand, no patient had a significant HAI score (Knodell ≥ 8) in the left-lobe biopsy samples. The rate of significant fibrosis stage (stage ≥ 2) was 66.7 % (18/27) in right-lobe biopsy samples; the same rate was observed (63.0 %, 17/27) in left-lobe biopsy samples, but the difference was not significant. The mean degree of steatosis was detected as 9.11 ± 16.07 (min: 0; max: 70). Portal tract numbers, stage and grade scores are given in Table 2.
Discussion
This study showed that the numbers of portal tracts and biopsy sizes were equal in right- and left-lobe samples. The right-lobe sample’s HAI score was higher from that of the left-lobe sample. However, the difference in terms of grading was not significant. Besides, we did find no significant difference in fibrosis staging between the two samples.
HBV infection is an important worldwide health problem, especially in developing countries. CHB is associated with a wide range of clinical conditions, from a healthy asymptomatic carrier status with a normal liver histology to severe and chronic liver diseases, including cirrhosis and hepatocellular carcinoma (HCC) [7]. There is a particular concern in the Asian region, where chronic HBV infection is common, with a chronic HBV carrier rate of approximately 10 %. About one-third of the CHB patients will die due to chronic liver disease [8]. The goal of treatment in patients with early stages is to stop the progression to cirrhosis; as such, liver biopsy is the first step of treatment.
Liver biopsy continues to have a main role as the ‘‘gold standard’’ in diagnosis and treatment of patients with CHB. In daily clinical practice, an important problem of liver biopsy is sampling variability. a liver biopsy sample is an only small amount of the liver, representing a 1:50,000 sample/whole organ ratio [9, 10]. Many studies have shown the clinical significance of sampling variability in chronic liver diseases [11–14]. In some studies, when paired samples were obtained from right and left lobes of the liver in patients with CHC, a difference of grades and/or fibrosis stages could be observed between the two samples in 20–30 % of patients [5, 15]. Similar differences were reported for non-alcoholic fatty liver disease where significant sampling variability was shown for diagnosis of NASH [16]. However, our study is the first to show liver biopsy sampling variability in CHB patients. In contrast to other research, we found no significant difference between two CHB samples in terms of grading and fibrosis staging.
According to pathological criteria, the optimal liver biopsy sample size is recommended to be at least 20 mm long, 1.4 mm wide or including 10 (at least 4–6) portal tracts [17–20]. In our study, numbers of portal tracts were appropriate to provide the basal criteria.
The most important limitation of our study is that only one pathologist evaluated the samples. The second limitation is the limited number of patients.
In conclusion, based on the findings of our study, we believe there is no need for a second biopsy in optimal sample collection conditions. This study showed that if the liver biopsy taken is the proper size, it is sufficient to predict treatment decisions in patients with hepatitis B. However, further studies with a larger number of patients are needed to compare the paired samples for grading and staging score in patients with CHB.
References
Lee WM. Hepatitis B virus infection. N Engl J Med 1997;337:1733–1745
Afdhal NH, Nunes D. Evaluation of liver fibrosis: a concise review. Am J Gastroenterol 2004;99:1160–1174
Rousselet MC, Michalak S, Dupre F, Croue A, Bedossa P, Saint-Andre JP, et al. Sources of variability in histological scoring of chronic viral hepatitis. Hepatology 2005;41:257–264
Cadranel JF, Rufat P, Degos F. Practices of liver biopsy in France: results of a prospective nationwide survey for the group of epidemiology of the French association for the study of the liver (AFEF). Hepatology 2000;32:477–481
Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 2003;38:1449–1457
Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, et al. LIDO Study Group. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 2005;128(7):1898–1906
Lai CL, Ratziu V, Yuen MF, Poynard T. Viral hepatitis B. Lancet 2003;362:2089–2094
de Franchis R, Hadengue A, Lau G, Lavanchy D, Lok A, McIntyre N, et al. EASL international consensus conference on hepatitis B. 13–14 September, 2002 Geneva, Switzerland. Consensus statement (long version). J Hepatol 2003;39:S3–S25
Bravo AA, Sheth SG, Chopra S. Liver biopsy. N Engl J Med 2001;344:495–500
Lee RG. General principles. In Lee RG, editor. Diagnostic Liver Pathology. St Louis: Mosby; 1994. p. 1–21
Maharaj B, Maharaj RJ, Leary WP, Cooppan RM, Naran AD, Pirie D, et al. Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Lancet 1986;1:523–525
Baunsgaard P, Sanchez GC, Lundborg CJ. The variation of pathological changes in the liver evaluated by double biopsies. Acta Pathol Microbiol Scand 1979;87:51–57
Abdi W, Millan JC, Mezey E. Sampling variability on percutaneous liver biopsy. Arch Intern Med 1979;139:667–669
Labayle D, Chaput JC, Albuisson F, Buffet C, Martin E, Etienne JP. Comparison of the histological lesions in tissue specimens taken from the right and left lobe of the liver in alcoholic liver disease. Gastroenterol Clin Biol 1979;3:235–240
Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 2002;97:2614–2618
Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD single topic conference. Hepatology 2003;37:1202–1219
Colloredo G, Guido M, Sonzogni A, Leandro G. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol 2003;39:239–244
Petz D, Klauck S, Roehl FW, Malfertheiner P, Roessner A, Röcken C. Feasibility of histological grading and staging of chronic viral hepatitis using specimens obtained by thin-needle biopsy. Virchows Arch 2003;442:238–244
Demetris AJ, Ruppert K. Pathologist’s perspective on liver needle biopsy size? J Hepatol 2003;39:275–277
Scheuer PJ. Liver biopsy size matters in chronic hepatitis: bigger is better. Hepatology 2003;38:1356–1358
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fuat Ekiz, İlhami Yuksel, Ata Turker Arikök, Baris Yilmaz, Akif Altinbas, Bora Aktas, Murat Deveci, Omer Basar, Sahin Coban, Osman Yuksel declare that they have no conflicts of interest.
Ethical standard
Our study was performed according to the guidelines of the Declaration of Helsinki, and the ethics review committee of our hospital approved it.
Informed consent
Informed consent to participate in the study was received from all patients.
Rights and permissions
About this article
Cite this article
Ekiz, F., Yuksel, İ., Arikök, A.T. et al. Will a second biopsy sample affect treatment decisions in patients with chronic hepatitis B?. Hepatol Int 10, 602–605 (2016). https://doi.org/10.1007/s12072-015-9666-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-015-9666-5