Abstract
Biphenotypic sinonasal sarcoma (BSNS) is a rare malignant tumor that affects the upper nasal cavity and ethmoid sinuses. It is more commonly found in middle-aged women and is characterized by the infiltration and hypercellular proliferation of spindle cells. These cells exhibit specific immunoreactivity. We add seven cases diagnosed as BSNS, to the handful of cases already available in the literature.BSNS is a malignant disease of the sinonasal tract that requires prompt and accurate diagnosis, followed by surgical resection and consideration of radiotherapy. Our analysis of seven cases supports previous research that confirms the aggressive nature of the disease but also shows that it is treatable with the right approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many phenotypes, presentations, and symptoms can be found in sinonasal tumors. And, due to this diversity in histology and proximity to vital structures such as the brain, orbit, base of the skull, and cranial nerves, they throw a diagnostic and therapeutic challenge to the diagnostician as well as the clinician.
About 1% of all head and neck cancers and 5–15% of all adult sarcomas are malignant spindle cell tumors of the head and neck [1].According to the 2017 World Health Organisation classification, there are eight main histologic categories of head and neck sarcomas, each of which has numerous variations.
Biphenotypic sinonasal sarcoma (BSNS) is a rare and slow-growing soft tissue sarcoma that has only been described in the last decade [1]. The tumor exhibits highly differentiated morphologic features and a high recurrence rate, but only locally without distant metastases. Immunohistochemical and molecular findings demonstrate the unique characteristics of this tumor, and it requires a thorough examination for proper diagnosis and treatment.
Patients typically present with vague, nonspecific symptoms related to tumor mass effect (e.g., nasal obstruction, congestion, and sinonasalpain) [2]The age of presentation ranges between 24 and 85 years with a female-to-male ratio of 2:1.
Studies in the last decade have attempted to characterize the clinical, morphologic, immunophenotypic features and genetic aberrations of BSNS.We hereby report a series of seven cases that presented between 2017 and 2022 in a tertiary care institute, along with a review of the literature on this entity.
Cases
Case 1
A 62-year-old female presented to the Otolaryngology outpatient department of this Institute with complaints of right nasal obstruction for the last 6 months. Her CT scan revealed a soft tissue polypoidal mass causing widening of the right nasal cavity, extending into the frontal and right anterior ethmoidal sinuses. This mass showed heterogenous enhancement and showed rarefaction of the underlying bone. A small biopsy was sent for histopathological examination, to plan the patient’s management course further. The small biopsy showed features of High-grade sarcoma, in which the tumor cells were positive for Vimentin on IHC and negative for CK and EMA.
The patient then underwent a Rhinectomy under GA, and the excised specimen was sent for Histopathological examination. Cut section of the gross specimen revealed a grey-white growth measuring 4 × 3 × 2 cm, microscopic examination of which showed a tumor composed of spindle cells arranged in fascicles. The individual cells showed moderate pleomorphism and occasional atypical mitosis. The tumor was seen infiltrating into the underlying bone around the septal cartilage. On IHC, these cells were strongly positive for Vimentin, S100, and focally positive for SMA, and negative for CK. Features were those of Biphasic Sinonasal sarcoma.
Case 2
A 67-year-old male, already diagnosed case of Squamous cell carcinoma of the buccal mucosa, post-RT/CT, presented with complaints of an ulceroproliferative growth on the left buccal mucosa extending up to the left vestibule, since the past 4 months. He had a chronic history of tobacco chewing. CECT revealed an ill-defined, heterogeneously enhancing soft tissue thickening in the left buccal mucosa, extending into the left gingivobuccal sulcus and left retromolar trigone, causing erosion of the underlying mandible.
The growth was excised and sent for histopathological examination. The biopsy showed a tumor composed of spindle cells, which showed mild to moderate pleomorphism, and atypical mitosis. The tumor cells on IHC were positive for SMA, S100, focally positive for Vimentin, and negative for CK, EMA, and CD34. Features were those of Biphenotypic Sarcoma.
Case 3
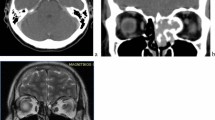
A 45-year-old male, with a long history of tobacco chewing, presented with a mass on the left lower gingivobuccal sulcus for the last 2 months, which bled on touch. CECT revealed an exophytic heterogeneously enhancing soft tissue lesion along the left lower buccal mucosa and gingivobuccal sulcus involving the retromolar trigone Fig. 1, abutting the alveolar process and the left masseter muscle. The mass was biopsied and sent for histopathological examination, which was diagnosed as BSNS, based on morphology and IHC.
Case 4
A 49-year-old male, smoker presented to the outpatient department of this Institute with complaints of an ulceroproliferative growth (UPG) on the lower gingivobuccal (GB) sulcus, which was associated with pain, anda burning sensation.Radiological investigations weren’t available.The growth was excised and sent for histopathological examination.Microscopically it revealed monotonous spindle cells. There was minimal atypia, focal necrosis and hemorrhage, and mitosis. On Immunohistochemistry, the spindle cells coexpressedsmooth muscle actin and S 100. Tumor cells were negative for CK, EMA, bcl2, and CD34. Based on the morphology and IHC a diagnosis of BSNS was made. Figure 2.
Case 5
A 56-year-old male, non-smoker presented with complaints of difficulty in swallowing and change in voice for the last 2 weeks along with complaints of a growth over the uvula associated with a foreign body sensation in the mouth. Radiologically it revealed a well-defined lobulated homogeneously enhancing soft tissue pedunculated mass lesion originating from uvula filling the oropharynx.Microscopically it revealed monotonous spindle cells. There was minimal atypia, focal necrosis and hemorrhage, and mitosis. On Immunohistochemistry, the spindle cells coexpressed smooth muscle actin and S 100.(Fig. 3) Based on the morphology and IHC a diagnosis of BSNS was made.
Case 6
A 51-year-old male, non-smoker presented to the Otolaryngology Outpatient department of this institute with complaints of a left neck swelling present for the last 6 months. Radiologically, the neck swelling revealed a soft tissue lesion in bilateral maxillary, ethmoidal, left frontal, and left sphenoidal sinuses.A small biopsy was sent from this mass for histopathological examination.Microscopically it revealed monotonous spindle cells. There was minimal atypia, focal necrosis and hemorrhage, and mitosis. On Immunohistochemistry, the spindle cells coexpressed smooth muscle actin and S 100. Based on the morphology and IHC a diagnosis of BSNS was made.
Case7
A 48-year-old-male, with a long history of tobacco chewing presented with an ulcero-proliferative growth over the hard palate over the last 2 months. A small biopsy from the growth was sent for histopathological examination. Microscopically, it revealed a relatively high-grade morphology with pleomorphic spindle cells showing nuclear atypia, and mitosis of 5–7/high power field. A differential diagnosis of leiomyosarcoma was considered, however, S100 was diffusely positive.After a careful review of the case based on clinico-radiological and histomorphological features and IHC, a diagnosis of BSNS was offered.
All the seven patients received post-op radiation therapy and were kept in close follow up. No recurrences were seen in all cases, clinically and on follow-up radiological imaging.
Discussion
BSNS is a recently described tumor that shows myogenic and neural differentiation, with only a hundred cases reported in the literature. The available data shows that these tumors tend to show a female preponderance, however, a multivariate analysis by Peng et al. shows that adult head and neck sarcomas tend to be more common in males. [3] They frequently occur in the fifth decade, with the mean age of presentation being 52.9 years(range 24–87). [4]
A third of patients had local recurrences during the first five years following surgery, despite the disease’s slow progression and lack of metastasis.The recurrence rate is between 40 and 50%, and the intervals between recurrences might be as short as one year or as long as nine years. Mortality from BSNS is extremely uncommon in the literature; only two cases of tumor-related death have been documented [4].
Tumors commonly involve the nasal cavity and ethmoid sinus. In some cases, tumor extension into the orbit, skull base involvement, and intracranial extension have also been reported.
In the seven cases that we report here, apart from the sex, the patient’s age, sites involved, clinical and radiological findings were consistent with the general demographic and localization characteristics of BSNS. There was no extra-sinonasal spread.
The primary histological characteristics of BSNS include benign sinonasal-type glands scattered and interspersed in spindle cell proliferation, an inadequate matrix organized in fascicles or a “herringbone” pattern, and a hemangiopericytoma-like vascular pattern.The “biphenotypic” characteristic of the tumor comesfrom the presence of both neural and myogenic markers in immunophenotypic studies. [2, 7]BSNS are characterized by S100 and SMA and/or muscle-specific actin (MSA) expression, as expressed by all the seven cases that we report here.
Rearrangements in the PAX3 gene, which is known to bea transcription factor that plays a critical role in neural andskeletal muscle differentiation, are responsible for the dual differentiation pattern [2].
In molecular analyses, Fluorescent in situ hybridization(FISH) studies, the PAX3-MAML3 fusion is present in79–96% of the cases and pathognomonic for BSNS. [4] It should also be noted that there are reports of patient groups in which PAX3 gene fusion was not detected [6]. This gene rearrangement can distinguish BSNS from its morphologic mimics with a high sensitivity of 100% [2, 6]. The PAX3 geneexpression could not be evaluated in our case as FISH cannot be performed in our hospital.
Since several spindle cell tumors occupy the nasal cavity and histopathologically show a fascicular arrangement, it becomes an important diagnostic challenge to identify and diagnose these tumors correctly, impacting the treatment modalities that the patient has to be offered by the clinician. Peripheral nerve sheath tumors, tumors with skeletal muscle and myoid differentiation, solitary fibrous tumors, and synovial sarcoma should be included in the differential diagnosis of BSNS. (Table 1)
BSNS is an important entity for pathologists to be familiar with because of the broad differential for head and neck spindle cell tumors and the indolent clinical behavior that distinguishes BSNS from common head and neck sarcomas. Pathologists as well as surgeons need to be aware of this entity to avoid misdiagnosis as a more aggressive disease entity.
Biphenotypic sinonasal sarcoma is a slow-growing tumor that can be removed through surgery since no cases of metastatic disease have been reported.The rates of recurrence following surgical excision and surgical excision combined with adjuvant radiation therapy are comparable; however, a determination of therapeutic superiority is hindered by the lack of follow-up data in reported cases, especially in instances when the surgical margins are positive. Therefore, to get the greatest possible treatment outcome, a multidisciplinary team must determine the course of treatment.
References
El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ (2017) WHO classification of Head and Neck tumours [Internet]. International Agency for Research on Cancer. (IARC WHO Classification of Tumours Series)
Kominsky E, Boyke AE, Madani D, Kamat A, Schiff BA, Agarwal V (2023) Biphenotypic Sinonasal Sarcoma: a Case Report and Review of Literature. Ear Nose Throat J 102(6):385–390
Peng KA, Grogan T, Wang MB (2014) Head and neck sarcomas: analysis of the SEER database, Otolaryngol. Head Neck Surg 151(4):627–633
Sudabatmaz EA, Abakay MA, Koçbıyık A, Sayın İ, Yazıcı ZM (2022) A rare sinonasal malignancy: biphenotypic sinonasal sarcoma. Turkish Archives Otorhinolaryngol 60(1):53
Anastasiadou S, Karkos P, Constantinidis J Biphenotypic Sinonasal Sarcoma with Orbital and Skull Base involvement report of 3 cases and systematic review of the literature. Indian J Otolaryngol Head Neck Surg 2023 Jun 22:1–1
Sethi S, Cody B, Farhat NA, Pool MD, Katabi N (2021) Biphenotypic sinonasal sarcoma: report of 3 cases with a review of literature. Hum Pathol (N Y) 24:200491
Chitguppi C, Koszewski I, Collura K, Curtis M, Nyquist G, Rabinowitz M et al (2019) Biphenotypic sinonasal sarcoma-casereport and review of clinicopathological features and diagnostic modalities. J NeurolSurg B Skull Base 80:51–58
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chaturvedi, A., Kumari, G., Dhankar, N. et al. Biphenotypic Sinonasal Sarcoma- A case Series with a Review of Literature. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04844-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-04844-z