Abstract
Aims Present study investigates the current trends in (Central) Auditory Processing Disorder [(C)APD] assessment and management practices among Audiologists practicing in Kerala, India. Materials and Methods The questionnaire for the survey was developed based on the Knowledge, Attitude, and Practices (KAP) model and underwent validation by experts in Audiology. Online survey was conducted to collect data from Audiologists practicing in Kerala, with a valid RCI-CRR number. Descriptive statistics were used to analyze the responses. Results The majority of participants held bachelor’s degrees and completed training modules on the assessment of (C)APD during their undergraduate studies. However, clinical exposure was very low. Even though 59.2% of participants reported that they were performing screening for (C)APD, the use of standardized screening tools was limited. Only 35% of participants reported that they were performing diagnostic evaluation. However, the rest of the participants used only speech-in-noise tests for (C)APD evaluation. The participants who performed management of (C)APD were even fewer, at only 13.4%. Lack of facilities, inadequate patient load, and lack of practical exposure were major obstacles to (C)APD assessment and management. The majority of participants strongly agreed that Audiologists are the most qualified persons to deal with (C)APD; however, the practice trends obtained from the study suggest that Audiologists have a really poor practice in this area. Conclusion The study highlights the need for standardized assessment tools, improved training opportunities, and increased awareness among Audiologists regarding (C)APD. Multidisciplinary collaboration and further research are essential for enhancing (C)APD assessment and management practices in Kerala.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
(Central) Auditory Processing Disorder [(C)APD] is a deficit in processing auditory stimuli in the auditory nervous system. It is not resulting from any higher-order language, cognitive, or learning difficulties. However, it coexists with a range of learning, language, and communication disorders [1]. Despite having normal audiograms, a notable percentage of children and young adults encounter such auditory processing challenges [2], warranting consideration as suspected (C)APD [3]. Assessing (C)APD remains challenging due to the absence of a gold standard diagnostic tool and the diverse presentation of symptoms [4]. Nevertheless, screening tools like the Screening Test for Auditory Processing (STAP) and the Screening Checklist for Auditory Processing (SCAP) show promise in identifying individuals at risk [5, 6]. Electrophysiological testing has also emerged as a valuable tool for early identification in children [7].
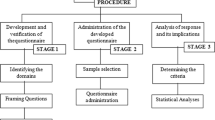
Management of (C)APD requires a multifaceted approach, including signal enhancement strategies, environmental modifications, and formal auditory training [8]. However, the lack of standardized practice protocols and therapy guidelines in India hindered effective intervention [9]. While many efforts have been made to address these gaps through systematic training programs, challenges are persisting, including limited awareness among healthcare professionals and linguistic diversity [10]. Further, it is important to explore Audiologists’ practice patterns, challenges, and knowledge regarding (C)APD assessment and management in the Indian context. Understanding these factors could help in the development of culture-specific guidelines, improving clinical outcomes, and enhancing advocacy efforts for individuals with (C)APD in India. Hence, the current study aims to fill this gap by investigating the knowledge, attitudes, and practices of Audiologists working in Kerala regarding the screening, assessment, and management of (C)APD.The objectives of this study include developing a questionnaire to assess the knowledge, attitude, and practices among Audiologists concerning the assessment and management of (C)APD and administering this questionnaire on Audiologists to gather relevant data.
Method
The online survey was conducted among Audiologists or Audiologists cum Speech-Language Pathologists practicing in Kerala state with a valid RCI-CRR number. Inclusion criteria comprised RCI registered Audiologists or Audiologists cum Speech-Language Pathologists working in Kerala, possessing a BASLP degree with or without MSc. Audiology or MASLP or higher qualification.
The survey questionnaire is developed based on the Knowledge, Attitude, and Practice (KAP) model [11]. The KAP surveys have been administered among the general public [12], persons directly related to any specific disorder [13] and healthcare professionals at various levels [14]. The questions for the survey were collected based on the thorough analysis of existing literature on (C)APD, and classified into for sections: experience and knowledge in (C)APD assessment, experience and knowledge about (C)APD management, opinions about current practices, and general opinions.
To ensure validity, the questionnaire underwent validation by five experts in Audiology, who assessed content, meaning, accuracy, context, and clarity. Their recommendations were incorporated, followed by field testing among a small sample (10 Audiologists) for cognitive debriefing and refinement. The final questionnaire was transformed into a Google form with six sections, where first two were informed consent and demographic details. Remaining four sections were questions of above-mentioned categories. The link for survey was disseminated via email and social media platforms to Audiologists in Kerala. Ethical approval from the Institutional Ethics Committee for the study was secured on November 10, 2021. The initial section of the Google form comprised an informed consent form, and respondents were allowed to proceed with the survey only upon reading and consenting to participate.
Descriptive statistics and generation graphics were made using Microsoft Excel. No statistical testing was performed.
Results
Out of 150 professionals surveyed across various regions of Kerala, 142 participants were eligible for analysis, with 21.13% (30) being males and 78.87% (112) females. Eight respondents were excluded due to not meeting the inclusion criteria. Participants’ ages ranged from 23 to 38 years, with a mean age of 26.13 years. Among them, 54.7% were undergraduates, and 44% held postgraduate degrees. In terms of employment, 45.3% worked in the private sector, 21.3% in academic institutions, 20% in multispecialty hospitals, 3.3% in government hospitals, 3.3% in ENT clinics/ENT hospitals, and 2% in hearing aid/cochlear manufacturing companies.
Screening for (C)APD
Approximately 59.2% of Audiologists indicated that they conduct (C)APD screening at their facilities, primarily employing informal procedures. Despite their familiarity with screening tools such as Screening Checklist for Auditory Processing (SCAP), Screening Checklist for Auditory Processing in Adults (SCAP-A), or Screening Test for Auditory Processing (STAP), majority of participants reported not using standardized tools for screening purposes (Fig. 1 upper panel).
Diagnostic Assessment of CAPD
A large portion (92 out of 142) reported not conducting diagnostic assessments for (C)APD. Among those who did, 50 out of 142 used only the Speech Perception in Noise Test for diagnosis. Electrophysiological tests were not commonly utilized, with 91.5% of professionals foregoing their use, while 8.5% employed the LLR in assessment. Various tests used by the participants for assessment of (C)APD is given in Fig. 1 (lower panel).
Various challenges were identified by Audiologists during (C)APD assessment (Fig. 2, upper panel). Lack of patient load (45.1%), facility limitations (33.8%), practical exposure (25.4%), and hands-on training (19%) were the notable concerns. A large number of participants (26.1%) reported that the assessment of CAPD is not part of their current job description.
Regarding comorbid conditions that contradict administration of CAPD assessment, Specific Language Disorder was cited as a contraindicating condition for (C)APD diagnosis by 66.9% of participants, followed by ADHD (54.7%), low IQ (39.4%), cognitive deficits (47.9%), speech delay (46.5%), poor vision (12%), language delay (48.6%), non-native speaker (17.4%), and bilingual speaker (34.5%).
In case of facility limitations, 54.9% of participants opted for completing basic Audiological assessments, screening for (C)APD, and making appropriate referrals, while 40.8% opted for completing basic Audiological assessments and making referrals. Only 2.1% indicated they would refer patients back to the professional who made the initial referral, while one participant mentioned counselling and sending patients’ home.
Regarding test materials, 56.7% utilized standardized materials available in English or Indian English, 39% tried to complete assessments using available materials, and 2.8% attempted to develop their own test materials for informal assessments.
Majority of the Audiologists, who are performing diagnostic evaluation follow ASHA framework (27.5%) followed by American Academy of Audiology Clinical Practice Guidelines of (C)APD (9%), Bellis/Ferre model (6.3%), Canadian Guidelines on Auditory Processing Disorders (2.8%), and British Society of Audiology Position Statement and Practice Guidance of (C)APD (1.4%).
Management of (C)APD
A large proportion of respondents i.e., 86.6% (123 of 142) reported that they are not performing the management of (C)APD. Numerous obstacles hinder Audiologists in effectively managing (C)APD. As depicted in Fig. 2 (lower panel), lack of patient load (68.9%), practical exposure (43.7%), academic training (25.4%), facility (38.7%), and cultural/linguistic issues (18.3%) are prominent factors restricting (C)APD rehabilitation efforts. However, professionals engaged in management make utilize wide variety of programmes and strategies, as shown in Fig. 3. Other programmes or strategies suggested by the participants includes training on sustained auditory attention, auditory memory enhancement, working memory enhancement, auditory closure, and auditory training using interactive device.
In instances of facility limitations, 87.3% of participants completed Audiological assessments and provided appropriate referrals for further (C)APD management. The management of (C)APD necessitates a multidisciplinary team approach, with 81% of Audiologists collaborating with Speech Language Pathologists, 76.8% with parents, and 70.4% with Educators/Special Educators.
Opinions and Suggestions from Participants
Most of the participants (78.2%) strongly agree with the statement that “Audiologists are the most qualified professionals to perform (C)APD assessment and management”. Most Audiologists agree that an Audiologist with a bachelor’s degree can handle the evaluation and management of (C)APD. The assertion that Audiologists should have MASLP/ MSc. Audiology/equivalent PG to perform assessment and management of (C)APD received varying feedback from Audiologists. Most of them recommended that Certificate courses/short-term training courses in addition to UG or PG are required to perform an accurate (C)APD assessment and management. Audiologists have a neutral opinion about RCI-recognized CREs and workshops to provide adequate hands-on experience on (C)APD rehabilitation. Most of them suggested that the ‘on-the-job training’ is sufficient for performing assessment and management of (C)APD.
In section 6 of the questionnaire, Audiologists were asked two open-ended questions. Regarding their opinion on the current assessment and management practices of (C)APD by Audiologists in Kerala. Their suggestions to improve audiological services for (C)APD in Kerala, as summarized in Table 1, emphasize the need for enhanced training during academic programs, especially its clinical aspects. The major themes derived from these suggestions are, 1. Sufficient Training clinical exposure during undergraduate (UG), postgraduate (PG), and internship periods. 2. Conducting regular CRE programmes and short-term courses that provide hands-on training and updated knowledge about developments in the field., 3. Formulating standardized protocols for assessment and management tailored to different patient populations, languages, and regions., 4. Importance of creating awareness and education among Teachers, Special Educators, Physicians, and Paediatricians about (C)APD., 5. Improving resources and facility especially in terms of software based assessment and management modules, as well as conversion of available tests into native language. Participants stressed the importance of evidence-based practices and the execution of standardized protocols among Audiologists in Kerala.
Discussion
(C)APD, a specialized area within Audiology, is progressively gaining attention worldwide, as evidenced by the increasing number of articles [15]. India’s expanding speech and hearing workforce has led to a rise in (C)APD-related services [16], supported by modules and training in undergraduate and postgraduate curricula and RCI-CRE programs [16]. However, practical exposure to (C)APD remains limited among Audiologists, with only 1 to 5 cases encountered during their academic training.
The survey conducted by Chermak et al. among USA-based Audiologists found that many Audiologists are not engaged in (C)APD assessment [17]. Similar to their findings, the current study sheds light on the fact that many audiologists in Kerala only perform screening procedures rather than diagnostic evaluations and (C)APD intervention. It was discovered in the current study that audiologists administer informal screening procedures for (C)APD before referring to diagnostic evaluation at their facility or to other professionals for further evaluation. Several questionnaires are available for screening for (C)APD in Indian scenarios, such as the Screening Checklist for Auditory Processing (SCAP), Screening Checklist for Auditory Processing inAdults (SCAP-A), and Screening Test for Auditory Processing (STAP).
However, the present study reveals that the use of such tools is very limited among Audiologists in Kerala. It indicates that there is an urgent requirement to make standardized screening tools available to Audiologists in Kerala. Both verbal and nonverbal assessment procedures are advised to provide a clearer picture of the auditory processing, and the potential site of dysfunction, according to the American Academy of Audiology (AAA, 2010) and ASHA (2005) documents. Even though these methods are accessible, most audiological assessment tools for (C)APD are not appropriate for Kerala’s linguistically and contextually diverse setting, making the assessment and diagnosis of (C)APD difficult. In the case of the unavailability of culturally validated screening and diagnostic tools, they must be developed and disseminated to practitioners since most of them are using informal screening procedures rather than formal screening test materials.
The complex nature of (C)APD underscores the importance of a multidisciplinary approach. To maximize the efficiency of treatment for (C)APD, it is crucial that other professionals who provide background information and refer people to an Audiologist should take part in interventions for (C)APD. They need to be aware of the criteria for diagnosis of (C)APD and the variety of clinical and related services available [15]. The present study suggests that most Audiologists collaborate with parents, Speech-Language Pathologists, and Educators/ Special Educators. Audiologists may also increase awareness and understanding of (C)APD among other professionals because these professionals are responsible for carrying out management, in case of audiologists are not performing the management for (C)APD. Audiologists can provide services and workshops to other related professionals. Through that, they get the opportunity for multidisciplinary discussion. In addition, language and cognitive tests conducted before or in conjunction with audiological testing may help identify whether auditory processing problems are due to language or cognitive issues [4]. It would be ideal for Audiologists to have basic knowledge of some cognitive tests and language evaluation tests. Otherwise, a proper referral should be made.
According to this study, many Audiologists in Kerala refer patients with auditory processing difficulties to other professionals after screening evaluation and are not willing to provide management because of several factors. A study conducted by Logue-Kennedy et al. in 2011 gives similar findings, more than half of the study sample did not offer interventions in the area of (C)APD and the minority indicate that their strategies only consisted of offering advice to the client, with no formal intervention protocol [18]. Audiologists in Kerala face several obstacles to (C)APD management, including facility, academic knowledge, practical experience, and cultural-linguistic factors. Regional conferences and online platforms may address these issues [15]. Additionally, the lack of native language speech tests poses challenges, underscoring the need for their development.
Limitations of the Study
The study’s sample size, comprising less than 10% of Kerala’s Audiologist population, may not fully represent the diverse landscape of Audiologists in the region. Additionally, most respondents had less than five years of experience, and a significant proportion worked in the private sector, suggesting a need for broader representation across different professional sectors in future studies. Hence, we suggest future research based on KAP-based surveys among Audiologists working across India with larger sample size.
Summary and Conclusion
The survey reveals that only a small number of Audiologists are involved in screening, assessment, and management of (C)APD compared to other areas in audiology. Challenges like low patient numbers, limited facilities, and insufficient training are hindering (C)APD assessment and management. While many Audiologists recognize the importance of a Audiologist’s role in (C)APD, their participation is restricted due to obstacles like lack of facilities, low practical exposure and inadequate patient volume etc. To improve the situation, suggestions include better clinical training in academic programs, regular programs for continuing education, standardized protocols, and increasing awareness among other professionals like educators and physicians about CAPD.
References
Musiek FE, Chermak GD (2013) Handbook of central auditory processing disorder volume 1: auditory neuroscience and diagnosis, 2nd ed, Plural Publishing, San Diego
Hind SE, Haines-Bazrafshan R, Benton CL et al (2011) Prevalence of clinical referrals having hearing thresholds within normal limits. Int J Audiol 50:708–716. https://doi.org/10.3109/14992027.2011.582049
Ferguson MA, Hall RL, Riley A, Moore DR (2011) Communication, listening, cognitive and speech perception skills in children with auditory processing disorder (APD) or specific language impairment (SLI). J Speech Lang Hear Res 54:211–227. https://doi.org/10.1044/1092-4388(2010/09-0167)
Moore DR, Campbell NG, Rosen S, et al (2018) Position Statement and Practice Guidance Auditory Processing Disorder (APD) British Society of Audiology 19pp.
Yathiraj A, Maggu AR (2014) Validation of the screening test for auditory processing (STAP) on school-aged children. Int J Pediatr Otorhinolaryngol 78:479–488. https://doi.org/10.1016/j.ijporl.2013.12.025
Yathiraj A, Maggu AR (2013) Comparison of a screening test and screening checklist for auditory processing disorders. Int J Pediatr Otorhinolaryngol 77:990–995. https://doi.org/10.1016/j.ijporl.2013.03.028
Liu P, Zhu H, Chen M, Hong Q, Chi X (2021) Electrophysiological screening for children with suspected auditory processing disorder: a systematic review. Front Neurol 12:692840. https://doi.org/10.3389/fneur.2021.692840
Bamiou DE, Campbell N, Sirimanna T (2006) Management of auditory processing disorders. Audiol Med 4:46–56. https://doi.org/10.1080/16513860600630498
Yathiraj A (2015) Perspective article management of auditory processing disorders: the Indian scenario. J All India Inst Speech Hear 34:8–16
Bantwal AR (2011) (Central) auditory processing disorders: issues and challenges in India. Perspect Glob Issues Commun Sci Relat Disord 1:55–63. https://doi.org/10.1044/gics1.2.55
World Health Organization (2008) Advocacy, communication and social mobilization for TB control: a guide to developing knowledge, attitude and practice surveys No. WHO/HTM/STB/2008.46
Ferdous MZ, Islam MS, Sikder MT et al (2020) Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an onlinebased cross-sectional study. PLoS ONE 15:e0239254. https://doi.org/10.1371/journal.pone.0239254
Magoo J, Shetty AK, Chandra P et al (2015) Knowledge, attitude and practice towards oral health care among parents of autism spectrum disorder children. J Adv Clin Res Insights 2:82–86
Devaraj NK (2019) Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breath Physiol Disord 24:1581–1590. https://doi.org/10.1007/s11325-020-02040-1
Musiek FE, Baran JA, James Bellis T, et al (2010) Clinical practice guidelines: diagnosis, treatment, and management of children and adults with central auditory processing disorder. American Academy of Audiology retrieved from https://www.audiology.org/education-and-events/continuing-education/
Shivashankar N (2015) Status of central auditory processing disorders in India retrieved from https://hearinghealthmatters.org/pathways-society/2015/status-of-central-auditory-processing-disorders-in-india/
Chermak GD, Traynham WA, Seikel JA, Musiek FE (1998) Professional education and assessment practices in central auditory processing. J Am Acad Audiol 9(6):452–465
Logue-Kennedy M, Lyons R, Carroll C et al (2011) Services for children with central auditory processing disorder in the republic of Ireland: current and future service provision. Am J Audiol 20:9–18. https://doi.org/10.1044/1059-0889(2011/10-0028)
Funding
No funding was received for completion of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Swetha, M., Ramiz Malik, M. & Mathews, M. Practice Trends in (C)APD Assessment and Management: A Survey of Audiologists in Kerala. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04838-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-04838-x