Abstract
Background: Patients with undifferentiated acute dizziness usually report with rapid onset of severe, often disabling illusion of movement with many other features. This accounts for roughly 50 to 100 million visits globally in emergencies annually. The causes may be numerous. Thus, the perplexed clinician needs to pursue advanced diagnostic imaging and unnecessary hospital admission in these patients. Aims and objectives: This study aims to assess the validity of HINTS Plus (head impulse test-nystagmus-test of skew + hearing assessment) test in diagnosing central causes of vertigo in patients with acute undifferentiated vertigo presenting within 72 h of onset of symptoms. The other objectives are to understand epidemiology and describe the assessment and management of these patients. Method: The data of 82 patients who visited the clinic within 72 h of the onset of symptoms as mentioned earlier during two years from August 2021 to 2023 at Ankush Hospital was stratified and analyzed. The outcome is reported here. Results: Among 82 patients, peripheral vestibular cause accounts for 84%. 12% were due to ischemic stroke and cardiovascular reasons. The sensitivity of HINTS Plus in isolating central acute vestibular vertigo was 100%, and the specificity was 95.6%. Conclusion: The risk for central and cerebrovascular causes of dizziness increases in the elderly with the presence of neurological signs and other comorbidities. The sensitivity and specificity of HINTS plus (4 Components) is very high in identifying central causes of undifferentiated acute vestibular in the first 72 h of onset of symptoms when undertaken by a trained clinician.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with undifferentiated acute vertigo usually report with rapid onset of severe, often disabling illusion of movement, nausea, vomiting, and head motion intolerance may be associated with gait unsteadiness and/or nystagmus [1]. This is also labeled as Acute vestibular syndrome (AVS) [2, 3]. A similar presentation is seen in vestibular neuritis and cerebellar/brainstem stroke [4].
Cerebellar/brainstem stroke is the most feared cause of vertigo which may lead to disability or death. In this condition patients may present with neurologic symptoms such as limb weakness, paresthesia, diplopia, or dysarthria, but some present without these features. So, the condition may resemble vestibular neuritis.
Because of this, there is.
-
1.
fear of missing a stroke and urgent need to intervene, so as not to miss the best time for treatment strategies [5].
-
2.
need to address cardiovascular risk factors to reduce chances of developing future complications [6].
-
3.
increase resource efficiency [7].
-
4.
and to avoid malpractice litigations [8].
As the evaluation of the dizzy patient can be overwhelming due to broad differential [9], the perplexed clinician needs to pursue advanced diagnostic imaging [CT (Computed Tomography) and MRI (Magnetic Resonance imaging)], sometimes unnecessary hospital admission in these patients.
However, many reports have suggested that CT and MRI suffer from a poor sensitivity for early stroke and the missed diagnosis rate is high [5, 10]. Reports have also shown that the “Head impulse test, Nystagmus, Test of skew (HINTs)” is more sensitive than the neuroimaging method in distinguishing stroke in predicting central causes in acute undifferentiated vertigo [7, 11].
This study aims to assess the validity of the HINTS Plus (head impulse test-nystagmus-test of skew + hearing assessment) test in diagnosing central causes of vertigo in patients with acute undifferentiated vertigo presenting within 72 h of onset of symptoms. The other objectives are to understand the epidemiology, describe the assessment and management of these patients as well as standardization and optimization of HINTS plus with the help of Video Oculography (VOG) and audiometry and to improve reproducibility and shorten the learning curve, with reliability and practicality.
Material and Methodology
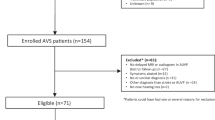
This study includes the patients visiting the clinic within 72 h of the onset of symptoms of undifferentiated acute dizziness/vertigo during two years from August 2021 to 2023. The data was stratified and analyzed. The outcome is reported here.
Inclusion criteria: undifferentiated acute vertigo i.e., acute onset of vertigo and dizziness as the main manifestation; with or without nausea, vomiting, head motion intolerance, gait unsteadiness, headache, limb numbness, speech abnormality, diplopia, facial weakness, eye movement disorders were taken into consideration, reported within 72 h of onset of symptoms and age ≥ 18 years.
Exclusion criteria: Obvious causes of dizziness, such as hypoglycemia, high-grade fever, influence of medications or alcohol usage, pregnant women, autoimmune or neoplastic disorders.
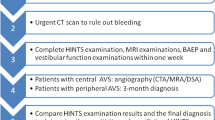
The workflow: Meticulous history and clinical data including age, gender, history of chronic diseases like hypertension, diabetes, heart disease, and alcohol intake was collected. Clinical examination and HINTS plus was done by a trained clinician with the help of video Oculography and hearing assessment with audiometry. Patients with transient vertigo and unidirectional nystagmus were segregated and treated for peripheral acute vestibular syndrome (AVS) with conservative management, maneuvers, and rehabilitation exercises and followed for one month to correct the initial diagnosis if required. Those patients with ongoing vertigo and /or uni/bidirectional nystagmus and the presence of other focal signs underwent HINTS plus examination. The presence of any of the positive HINTS plus test except the Head impulse test is considered a worrisome result. These patients with worrisome results are labeled with central AVS and subjected to neurological and cardiovascular evaluations with radiological investigations CT/MRI as per the specialist clinician’s requirement. otherwise, it is judged as a reassuring result as in peripheral AVS and treated for vestibular neuronitis. Patients who came out clear from neurological and cardiovascular assessment were then taken for Video nystagmography and treated accordingly (Chart 1). The data was then stratified and analyzed to describe the epidemiology, sensitivity, and specificity of HINTS plus.
Results
A total of 82 patients with undifferentiated acute dizziness were assessed from August 2021 to 2023. The age range of these patients is between 18 years to 82 years. 56 (68.2%) are female and 26 (31.7%) males.
In the spectrum of acute undifferentiated vertigo, peripheral vestibular cause accounts for 84%. 65% were diagnosed with Benign paroxysmal positional vertigo (BPPV), and 18% with Vestibular neuritis. In central vertigo, stroke accounts for 12%, Cardiovascular reasons for 1.2%, 3.6% due to Vestibular migraine (Chart 2a). Patients labeled with central causes of vertigo were above 36 years of age. 80% of them had comorbidities like hypertension, diabetes, or a previous history of stroke. Its incidence (Central causes of vertigo) was found to be higher in males 77% (10) than in females 23% (3), while for peripheral causes, there were more females 73% (38) than males 27% (14) (Chart 2b, c).
The sensitivity of HINTS Plus (head impulse-nystagmus-test of skew + hearing assessment) in isolating central acute vestibular vertigo, was 100%, and specificity was 94.5% (Table 1).
Discussion
There are numerous words to express the sensation of being dizzy. Probably we don’t have the right lexicon to describe it appropriately. Patients may use this word for vertigo, but may also use it to describe presyncope, imbalance, light-headedness, and other sensations. Thus, the distinction is of limited clinical utility [2, 3, 12]. Acute vestibular syndrome diagnosis requires the presence of persistent vertigo for more than 24 h, lasting for days to weeks [13].
Dizziness and vertigo account for about 2.6-4 million visits in emergency annually in the United States, roughly 50 to 100 million worldwide [2, 13]. 20% of them make their way to hospital admission [12, 14] out of these only 0.7 to 4% receive a diagnosis of ischemic stroke [15, 16]. A study conducted among the rural population in India reported an overall prevalence of dizziness of 0.71% [17]. No further reliable data is available for India and to date, no large population-based study has investigated the frequency of stroke among patients presenting in emergency with dizziness.
A common finding in several studies is that females suffer more from peripheral vertigo compared to males. Kurre and colleagues had 61.8% female patients [18] and Yetiser et al. observed 1.5-fold more female patients suffering from Benign paroxysmal positional vertigo (BPPV) [19]. In this study also there was an overall preponderance of female patients (68%) presenting with acute symptoms of vertigo and dizziness. More female patients (73%) suffered from peripheral causes of vertigo than men (Chart 2a). That was probably due to some association between comorbid anxiety and depression [20].
It’s interesting to note that central causes of vertigo were more common in male patients 77%. This has been observed in previous studies also [16]. Most of these patients also suffered from some other comorbidities like hypertension and diabetes. The proportion of cerebrovascular events in patients with dizziness symptoms varied in previous studies from 2 to 25% [16, 21]. In this study, 17% of patients were referred to specialists for central causes of vertigo (Chart 2b, c) and three of them came out to be clear of any serious cerebrovascular issues. Adjusting this number, 13% were truly suffering from stroke or cardiac complication. Most stroke patients with dizziness symptoms also had other neurologic features such as face/arm weakness, numbness, or speech/ language abnormalities to indicate a central lesion.
It’s worth mentioning that the cumulative incidence of stroke in patients visiting an emergency with symptoms of dizziness and vertigo and those who did not receive a stroke diagnosis is approximately 0.3% at 90 days [15] Lee et al. proposed that these patients had a higher risk for subsequent vascular events during the first year of their visit in emergency with symptoms of dizziness [6].
Cerebellar/brainstem stroke is the most feared cause of vertigo which may lead to increased disability or death. The fear of this disability and lack of overall diagnostic accuracy [16] for peripheral and central vestibular vertigo in acute circumstances, roughly 1 million with peripheral vestibular causes are over-tested [22], hundreds of millions of dollars are spent on brain imaging and hospital admissions trying to rule out dangerous central vestibular causes [21], still miss diagnosed [16] and undertreated [23]. Some patients can also present without neurological features which may resemble vestibular neuritis [24]. The evaluation of the dizzy patient can also be overwhelming due to broad differential and multisystem involvement. Moreover, patients often have difficulty in describing their symptoms with conflicting accounts being given at different times. Anxiety may significantly increase the risk of dramatic presentation and recurrences [9]. .
In different studies, CT and MRI were found to have low sensitivity in diagnosing early ischemic stroke with missed diagnosis rates ranging from 12 to 60% within 48 h [5, 13]. However, false negative stroke examination by MRI is relatively out-of-date due to the advancement in technologies [5]. Even if structural neuroimaging improves in the future, there will always be a place for physiological tests. As soon as the patient becomes symptomatic with acute vertigo, Oculomotor physiology changes instantaneously. Hence when correctly applied, the head impulse test has proven to be more accurate than diffusion-weighted MRI [7, 25].
Multiple studies and systematic reviews have shown sensitivity of HINTS ranging from 83 to 100% and Specificity from 44 to 96% within 48 h after onset of symptoms in identifying stroke [7, 13, 26]. Tao Qui and colleagues assessed the head impulse test, nystagmus, and test of skew individually. Their collective sensitivity was specificity of 89.8% and 84.2% respectively [5]. In a study by Edlow et al., it was suggested that only patients with persistent ongoing vertigo and spontaneous or gaze-evoked nystagmus undergo a head impulse test [27]. In this study the same was followed i.e., HINTS Plus (four components) examination with the help of Video-oculography (VOG) and audiometry. The sensitivity of HINTS plus for diagnosing central vestibular causes in acute undifferentiated vertigo turned out to be 100% and specificity 94.5% (Table 1). Video-oculography (VOG) devices record and measure key eye movements and can help in diagnosing, recording, training, and reproducing results. Although artifacts still require expert interpretation [2].
In some rare instances as Anterior inferior cerebellar artery strokes (i.e., labyrinthine infarction), rarely in basilar artery occlusion and Posterior inferior cerebellar artery stroke, there will be an abnormal HIT i.e., reassuring results mimicking vestibular neuritis. However, a large skew deviation and hearing loss are frequently present in these patients [7, 28]. Hyden et al. also advocated a collective approach in such patients unless proven otherwise [29].
There are a few limitations of HINTS plus examination. In case of head trauma, neck trauma, an unstable spine, or neck pain Head impulse test needs to be avoided. Certainly, all causes of vertigo cannot be diagnosed in this way. Most of the other rare causes of vertigo will also have some preexisting comorbidities or some features indicating that it’s not an isolated vertigo at the time of presentation.
Conclusion
The risk for central and cerebrovascular causes of dizziness, although low in undifferentiated acute vertigo, increases in the elderly with the presence of neurological signs and other comorbidities. The sensitivity and specificity of the HINTS plus (four components) test is very high in identifying central causes in undifferentiated acute vertigo compared to CT and MRI in the first 72 h of onset of symptoms when undertaken by a trained clinician. HINTS plus test-based workflow is evidence-based management, low-cost, and easy to carry out and learn. Improved technical equipment like Video oculography and audiometry, can effectively improve the diagnosis and significantly reduce the chance of a miss. The reproducibility of results is strong and the learning curve is short.
References
Hotson JR, Baloh RW (1998) Acute vestibular syndrome. N Engl J Med 339:680–685
Newman-Toker DE, Edlow JA (2015) TiTrATE: a novel, evidence-based approach to diagnosing acute dizziness and vertigo. Neurol Clin 33(3):577–599
Edlow JA, Gurley KL, Newman-Toker DE (2018) A New Diagnostic Approach to the adult patient with Acute Dizziness. J Emerg Med 54(4):469–483
Goldman B, Johns P (2020) Vertigo. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J (eds) Tintinalli’s Emergency Medicine: a Comprehensive Study Guide, 9th edn. McGraw Hill, New York, p 1145
Qiu T, Dai X, Xu X et al (2022) A prospective study on the application of HINTS in distinguishing the localization of acute vestibular syndrome. BMC Neurol 22:378. https://doi.org/10.1186/s12883-022-02904-x
Lee CC, Ho HC, Su YC, Chiu BC, Su YC, Lee YD, Chou P, Chien SH, Huang YS (2012) Increased risk of vascular events in emergency room patients discharged home with diagnosis of dizziness or vertigo: a 3-year follow-up study. PLoS ONE 7(4):e35923. https://doi.org/10.1371/journal.pone.0035923
Newman-Toker DE, Kerber KA, Hsieh YH et al (2013) HINTS outperforms ABCD2 to screen for stroke in acute continuous vertigo and dizziness. Acad Emerg Med 20(10):986–996
Ghaith S, Voleti SS, Bellolio F, Edlow JA, Lindor RA (2023) Dizziness as a missed symptom of central nervous system pathology: a review of malpractice cases. Acad Emerg Med 30(5):589–591. https://doi.org/10.1111/acem.14627
Chawla N, Olshaker JS (2006) Diagnosis and management of dizziness and vertigo. Med Clin North Am 90(2):291–304. https://doi.org/10.1016/j.mcna.2005.11.003
Newman-Toker DE (2016) Missed stroke in acute vertigo and dizziness: it is time for action, not debate. Ann Neurol 79(1):27–31
Carmona S et al (2016) The diagnostic accuracy of Truncal Ataxia and HINTS as Cardinal signs for Acute vestibular syndrome. Front Neurol 7:125
Smith DB (1990) Dizziness. A clinical perspective. Neurol Clin 8(2):199–207
Kattah JC et al (2009) HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 40(11):3504–3510
Crespi V (2004) Dizziness and vertigo: an epidemiological survey and patient management in the emergency room. Neurol Sci 25(Suppl 1):S24–S25. https://doi.org/10.1007/s10072-004-0212-9
Kerber KA (2020) Acute vestibular syndrome. Semin Neurol 40(1):59–66. https://doi.org/10.1055/s-0039-3402739
Kerber KA, Brown DL, Lisabeth LD, Smith MA, Morgenstern LB (2006) Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke 37(10):2484–2487
Abrol R, Nehru VI, Venkatramana Y (2001) Prevalence and etiology of vertigo in adult rural population. Indian J Otolaryngol Head Neck Surg 53(1):32–36. https://doi.org/10.1007/BF02910976
Kurre A, Straumann D, van Gool CJ, Gloor-Juzi T, Bastiaenen CH (2012) Gender differences in patients with dizziness and unsteadiness regarding self-perceived disability, anxiety, depression, and its associations. BMC Ear Nose Throat Disord 12:2. https://doi.org/10.1186/1472-6815-12-2
Yetiser S, Ince D (2015 Jan-Feb) Demographic analysis of benign paroxysmal positional vertigo as a common public health problem. Ann Med Health Sci Res 5(1):50–53. https://doi.org/10.4103/2141-9248.149788
Ferrari S, Monzani D, Baraldi S, Simoni E, Prati G, Forghieri M, Rigatelli M, Genovese E, Pingani L Vertigo in the pink: the impact of female gender on psychiatric-psychosomatic comorbidity in benign paroxysmal positional vertigo patients. Psychosom 2014 May-Jun ;55(3):280–288. https://doi.org/10.1016/j.psym.2013.02.005
Saber Tehrani AS, Coughlan D, Hsieh YH et al (2013) Rising annual costs of dizziness presentations to U.S. emergency departments. Acad Emerg Med 20(7):689–696
Newman-Toker DE, Camargo CA Jr, Hsieh YH, Pelletier AJ, Edlow JA (2009) Disconnect between charted vestibular diagnoses and emergency department management decisions: a cross-sectional analysis from a nationally representative sample. Acad Emerg Med 16(10):970–977
Kerber KA, Burke JF, Skolarus LE et al (2013) Use of BPPV processes in emergency department dizziness presentations: a population-based study. Otolaryngol Head Neck Surg 148(3):425–430
Lui F, Foris LA, Willner K et al Central Vertigo. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan https://www.ncbi.nlm.nih.gov/books/NBK441861/
Tarnutzer A (2023) Bedside Testing in Acute vestibular syndrome - HINTS Plus and Beyond –. Crit Rev https://doi.org/10.20944/preprints202306.1058.v1
Ohle R et al (2020) Can Emergency Physicians accurately rule out a Central cause of Vertigo using the HINTS examination? A systematic review and Meta-analysis. Acad Emerg Med 27(9):887–896
Edlow J, Newman-Toker D (2016) Using the physical examination to diagnose patients with acute dizziness and vertigo. J Emerg Med 50:617
Beyea JA, Agrawal SK, Parnes LS (2012) Recent advances in viral inner ear disorders. Curr Opin Otolaryngol Head Neck Surg 20(5):404–408
Hydén D, Akerlind B, Peebo M (2006) Inner ear and facial nerve complications of acute otitis media with focus on bacteriology and virology. Acta Otolaryngol 126(5):460–466
Author information
Authors and Affiliations
Contributions
None of the authors of this paper has a financial or personal relationship with other people or organizations that could inappropriately influence or bias the content of the paper. This research received no specific grant from any funding agency in the public, commercial, or not–for–profit sector. All authors have full access to the full data in the study and accept responsibility for submitting it for publication.
Corresponding author
Ethics declarations
Ethical Procedure
The research meets all applicable standards about the ethics of experimentation and research integrity, and the following is being certified/declared true.
The paper has been submitted with full responsibility, following due ethical procedure, fraud, plagiarism, or concerns about animal or human experimentation.
Competing Interests
No competing interests are at stake and there is No Conflict of Interest” with other people or organizations that could inappropriately influence or bias the content of the paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mittal, M. Diagnosing Emergencies in Undifferentiated Acute Vertigo. Indian J Otolaryngol Head Neck Surg 76, 2314–2319 (2024). https://doi.org/10.1007/s12070-024-04493-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04493-2