Abstract
Background: Neonatal oral cavity masses present complex diagnostic and management challenges, often involving respiratory distress. We present a case of a 1-day-old male neonate with an oral cavity mass and respiratory distress, whose antenatal scan revealed polyhydramnios and a nasopalatine cyst. Case Report: Clinical examination revealed a 5 * 5 cm cystic swelling arising from the right hard palate. CT scans confirmed an intraoral cystic lesion with a complete cleft palate and excluded oropharyngeal/neck extension. Aspiration of cystic fluid facilitated surgical excision, leading to a histopathological diagnosis of mature cystic teratoma. Primary closure of the soft palate defect was performed. Histopathological examination revealed it to be mature cystic teratoma. Conclusion: This case underscores the intricate interplay between antenatal imaging, clinical assessment, and surgical intervention in managing neonatal oral cavity masses. The successful excision and histopathological confirmation of a mature cystic teratoma highlights the significance of accurate diagnosis and timely intervention. The complexities surrounding neonatal oral cavity masses necessitate a comprehensive approach to optimize patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital anomalies involving the oral cavity in neonates can lead to significant respiratory distress and necessitate prompt evaluation and management [1, 2]. This case report presents the clinical course of a 1-day-old male neonate who exhibited a mass in the oral cavity and respiratory distress. The antenatal scan revealed polyhydramnios and a 4 * 4 cm nasopalatine cyst. Subsequent CT scans indicated an intraoral cystic lesion accompanied by a complete cleft palate.
Case Report
The neonate, male and aged 1 day, presented with respiratory distress and an observable mass in the oral cavity. Preceding birth, an antenatal scan identified polyhydramnios in the mother and a nasopalatine cyst measuring 4 * 4 cm in the fetus. A planned cesarean section was undertaken for the delivery of the child because of the same.
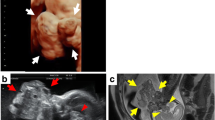
Upon clinical examination, a cystic swelling measuring 5 * 5 cm was observed on the right side of the hard palate, coinciding with the presence of a cleft palate. The tongue remained spared, albeit being pushed posteroinferiorly. (Fig. 1) Further diagnostic investigations through CT scans of the neonate on day 1 of birth revealed a well-defined, heterogeneous intraoral lesion arising from the basi-sphenoid region with minimal calcifications and no bony erosions. The lesion had no intracranial extension. Additionally, a complete cleft palate was identified. There was no involvement of cervical lymph nodes and great vessels. An MRI to look for intracranial extension was not feasible as the neonate needed urgent airway management.
1 day old male neonate presenting with a large oral cyst originating from the right side of the hard palate (a) along with the presence of an isolated complete cleft palate (b). Aspiration of the oral cyst led to the shrinkage of the cyst (c). Removal of the cyst from the attachments to the palate using a coblator wand (d)
With the patient under general anesthesia and oropharyngeal intubation, the ENT team initiated the procedure. (Fig. 2)
(a) Aspiration of 45 cc of fluid from the cyst. (b) The entire cyst along with the cyst wall was removed. This led to prolapse of the soft tissue surrounding the cyst and this defect was closed using absorbable sutures. (The photo shows the prolapsed healthy soft tissue and not the remnant of the cyst) (c) The excised sample sent for Histopathological study
Treatment
The initial step involved aspirating the cystic fluid utilizing an 18 G wide bore needle, resulting in the extraction of 45 cc of serous fluid. This aspiration led to cyst shrinkage, facilitating more surgical manoeuvrability. The subsequent excision of the cyst was conducted using a coblator wand (Procise Max Wand). The excised tissue (including the cyst wall) was sent for histopathological examination. Removal of the entire cyst led to prolapse of the soft tissue surrounding the excised cyst. This defect of soft palate was repaired through suturing using Vicryl 3 − 0 round body sutures. Following the procedure, the patient remained intubated and was relocated to the Neonatal Intensive Care Unit (NICU) for postoperative care.
Outcome and Follow-up
The specimen was processed thoroughly and urgently and the histopathological report revealed the mass to be a mature cystic teratoma. The patient was then referred to an oncology center for close long term follow up and review of the histopathological report.
Discussion
Teratomas of the oropharynx, commonly called as epignathus are a very rare occurrence and account for only 2% of all the subsites related to teratomas [3]. These are typically seen in midline or para-axial locations, often arising in the basisphenoid region as remnants of Rathke’s pouch. They are often associated with other congenital malformations with cleft palate being the most common occurrence as was seen in our case. This is attributable to failure of fusion of the secondary palate during the 8th week of gestation due to the development of oropharyngeal teratoma growth. This results in cleft palate.
It has been widely hypothesized that teratomas arise from the unchecked proliferation of pluripotent cells during the period of embryogenesis.
The antenatal scans hinting at polyhydramnios and nasopalatine cyst laid the foundation for further investigations in our patient. The presence of a nasopalatine cyst has been linked to oesophagal compression and thus reducing the absorption of amniotic fluid [4]. CT scan after birth delineated the extent of the cystic lesion, revealing the presence of a complete cleft palate while excluding neck involvement and intracranial extension.
The initial aspiration of cystic fluid not only contributed to the diagnosis postoperatively but also set the stage for subsequent surgery. Utilizing the coblator wand for excision proved to be an effective means of complete removal while minimizing tissue damage. It also aided in effective hemostasis during and after the procedure.
The histopathological examination unveiled the nature of the excised tissue as a mature cystic teratoma, characterized by mature neural tissue, adipose tissue, skeletal muscle, blood vessels, and nerve bundle fibres. Although rare, neonatal oral cavity teratomas underscore the necessity of accurate diagnosis and timely management. The case raises awareness about teratomas, which are true neoplasms composed of tissue derived from all three germinal layers. Although they are more common in females, neonatal teratomas are generally benign. Malignant transformation tends to occur more commonly in tumours diagnosed among older children. The determination of malignancy relies on the extent of tissue differentiation. However, malignancy is not solely contingent on the histological characteristics of the tumour but also considers the occurrence of synchronous or asynchronous metastases. Jordan et al. [5]. reported a case of neonatal neck teratoma that appeared benign upon histological analysis but was accompanied by synchronous liver metastases in the child. Airway obstruction and respiratory compromise are potential complications that highlight the urgency of management.
Teratomas are often associated with synchronous and metachronous lesions and thus require a long-term follow-up. Our case was followed up with a repeat MRI after one year to look for any local or distant seeding [6].
Conclusion
This case report emphasizes the complexity of neonatal congenital anomalies involving oral cavity masses and the consequential respiratory distress. A collaborative approach, involving antenatal scans, advanced imaging, surgical intervention, and histopathological assessment, culminated in the successful diagnosis and management of a mature cystic teratoma in a neonate. The teamwork between obstetricians, neonatologists, pediatric anaesthetists, ENT surgeons, and pathologists played an essential role in securing favourable patient outcomes.
The cornerstone of management for oropharyngeal teratomas lies in establishing and maintaining a secure airway. Early surgical intervention, aiming for complete mass excision, is crucial to prevent recurrence. Adjuvant chemotherapy and radiotherapy become necessary if histological analysis reveals malignant components. Repair of associated cleft palate can be deferred to a later age, usually around 1½ years. This case underscores the importance of a comprehensive and multidisciplinary approach in diagnosing and managing neonatal congenital anomalies, particularly those involving the oral cavity.
References
Patil S, Rao RS, Majumdar B, Jafer M, Maralingannavar M, Sukumaran A (2016) Oral lesions in neonates. Int J Clin Pediatr Dent 9(2):131–138
Shear M, Speight PM. Cysts of the Oral and Maxillofacial Regions [Internet]. Google Books. John Wiley & Sons; 2008 [cited 2023 Aug 10]. Available from: https://books.google.co.in/books?hl=en&lr=&id=Jgt7046OlUAC&oi=fnd&pg=PR5&ots=Kn7RJoZi1N&sig=EyBK48-_XChUF61y4jMC7MQBiyg&redir_esc=y#v=onepage&q&f=false
Azizkhan RG, Caty MG (1996) Teratomas in childhood. Current Opinion in Pediatrics [Internet]. Jun 1 [cited 2023 Aug 10];8(3):287. Available from: https://journals.lww.com/co-pediatrics/Abstract/1996/06000/Teratomas_in_childhood.18.aspx
Liechty KW, Crombleholme TM, Flake AW, Morgan MA, Kurth CDean, Hubbard AM et al (1997) Intrapartum airway management for giant fetal neck masses: the EXIT (ex utero intrapartum treatment) procedure. Am J Obstet Gynecol 177(4):870–874
Jordan RB, Gauderer MWL (1988) Cervical teratomas: an analysis. Literature review and proposed classification. J Pediatr Surg 23(6):583–591
Anderson PJ, David DJ Teratomas of the head and neck region. Journal of Cranio-Maxillofacial Surgery [Internet]. 2003 Dec 1 [cited 2023 Aug 10];31(6):369–77. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1010518203000672
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for this study was obtained from “Institutional Ethics Committee (IEC)-II Seth GSMedical College and KEM Hospital”. Approval number : IEC(II)/OUT/679/2020 (10th November 2020).
Consent to participate
Yes.
Consent to publish
Yes.
Competing Interests
There are no competing interests among the authors.
Compliance with Ethical Standards
Yes.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sahai, A., Narkhede, K., Shriwastav, P. et al. Mature Cystic Oral Teratoma in a Neonate- A Case Report. Indian J Otolaryngol Head Neck Surg 76, 1994–1997 (2024). https://doi.org/10.1007/s12070-023-04336-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04336-6