Abstract
Orbital abscesses are primarily seen in children as complication of ethmoid bacterial sinusitis. We report a case of invasive aspergillosis causing orbital abscess in an immunocompetent child which resolved with surgery followed by antifungal therapy. This case highlights need for histopathological, and microbiological examination, including fungal culture in such cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paediatric orbital abscesses are mostly seen as a complication of ethmoid sinus bacterial sinusitis. We report a case of invasive aspergillosis causing orbital abscess in an immunocompetent child. This case highlights need for histopathological and microbiological examination, including fungal smear and culture in such cases.
Case Presentation
A 10-year-old girl presented with swelling and drooping of right upper eyelid for three days with a constant, low-grade fever for a day. This was preceded by an upper respiratory infection, which was treated with antibiotics. She was an otherwise healthy child with no significant prior history.
On examination, the right eye showed tender periorbital oedema and erythema, with near-complete mechanical ptosis, chemosis and restriction of elevation, adduction and depression. However, corneal reflexes were intact and visual acuity was 6/9 (Snellen’s). Ophthalmological examination revealed right non-axial proptosis of 22 mm and hyperaemic discs. There was no facial anaesthesia or mucopurulent discharge on anterior rhinoscopy. The left eye examination and the rest of the ENT examination were unremarkable.
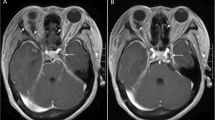
Blood investigations were normal except for a neutrophilic leucocytosis. Contrast-enhanced CT scan (CECT) of the nose, orbit and paranasal sinuses depicted right proptosis, periorbital and preseptal inflammatory changes and medial extraconal subperiosteal 35 × 9.5 × 23 mm collection, which displaced the medial rectus muscle, extended posteriorly to the orbital apex and abutted the optic nerve (Fig. 1). Fat stranding was present in the perineural area and the intraconal compartment with globe tenting. Right maxillary sinus, anterior and posterior ethmoid air cells showed soft-tissue opacification with focal dehiscence of lamina papyracea and infiltration of pterygopalatine and infratemporal fossae.
With a presumptive diagnosis of right, acute subperiosteal abscess, the patient was taken up for emergency surgery under general anaesthesia, where right middle meatal antrostomy, ethmoidectomy and sphenoidotomy were done, and mucopus was drained. Lamina papyracea and medial orbital floor were removed, periorbita incised, and the intra-orbital abscess was drained. Her postoperative period was uneventful, and she was discharged on the third postoperative day after pack removal.
Histopathological examination of the surgical specimen revealed fibro collagenous tissue, inflammatory changes and microabscesses, with short branched fungal hyphae, suggestive of Aspergillus species as highlighted by GMS (Grocott Methenamine Silver) staining (Fig. 2). Deeper sections and bones were free of fungus with no angioinvasion.
Intraoperative pus culture sent was positive for pan-sensitive Pseudomonas aeruginosa. She was treated with Ceftazidime and Amphotericin 50 mg intravenously daily for a week, followed by Voriconazole 200 mg tablets once daily for the next four weeks. The patient improved rapidly with complete resolution of periorbital swelling and full recovery of extraocular movements. Her liver function tests were monitored throughout her therapy. A repeat CT scan after three months depicted bulky extraocular muscles, complete clearance of abscess, with sinuses showing postoperative changes. The patient was kept under close follow-up for the next eighteen months and remains asymptomatic.
Discussion
Even though orbital complications of sinusitis are commoner in children, with 5–7% children with acute bacterial sinusitis developing them, underlying fungal aetiology in immunocompetent children is rare [1], with only four paediatric orbital aspergilloses reported. Hot, humid climate favours fungal growth resulting in more fungal spores circulating in the air exposing relatively younger patients to such an environment [2]. Initial fungal colonisation usually remains asymptomatic in healthy individuals but may progress to tissue invasion when defences are lowered. Direct extension via bony dehiscences, thrombophlebitis and septic emboli through the valveless system, immaturity of cell-mediated and humoral immune systems and defective phagocytosis may be the causes in apparently immunocompetent children. Our patient did not have any history to suggest immunodeficiency, and workup for immunodeficiency was negative. Though almost 90% of patients with orbital involvement have associated sinus disease, sino-nasal symptoms are rare at presentation, like in our case [3].
For any patient presenting with orbital symptoms like proptosis, restriction of eye movements or diminution of vision, imaging of choice is a contrast-enhanced CT scan of the orbit and paranasal sinuses. In orbital abscesses, CT reliably identifies peripheral enhancement, calcifications and retained secretions and debris [4]. Bone erosion is equivocal and may not be diagnostic for Aspergillosis. MRI is preferred for better soft tissue delineation.
Orbital abscess is a potentially fatal emergency, leading to rapid vision loss and life-threatening complications such as cavernous sinus thrombosis and requires immediate surgical intervention. Any orbital subperiosteal abscess requires close monitoring of vision and eye movements to prevent optic compression neuropathy. Oxford et al. have suggested medical management of medial orbital subperiosteal abscess in children when the patient has normal vision, pupil, and retina with no ophthalmoplegia, intraocular pressures (IOP) < 20 mm Hg, proptosis of 5 mm or less; and an abscess width of 4 mm or less [5]. Given restricted eye movements and impending visual complications, we decided to proceed with immediate surgical intervention. Along with abscess drainage to relieve the intraorbital tension, endoscopic sinus surgery needs to be done to address the source of infection and to obtain samples for biopsy and cultures. It is imperative to send pus and tissue samples for both bacterial and fungal cultures. When the underlying aetiology is a fungal infection, in addition to the above, surgical debridement reduces the tissues’ fungal load for increased antifungal penetration and aerates the anaerobic microenvironment [6]. Globe-conserving local debridement is the standard of care in cases of potentially salvageable vision. Surgery should be followed by culture-directed antibiotics or antifungal therapy, with a broad-spectrum antifungal like Amphotericin B or azoles such as voriconazole based on the fungal smear and culture report.
Conclusion
Though orbital aspergillosis is an unlikely cause of proptosis, ptosis, and fever in an otherwise healthy immunocompetent child, our case highlights the need for sending fungal smear and culture intraoperatively for all cases of acute sino-orbital infections. Absence of sinonasal symptoms does not rule out a primary focus of infection in the sinuses, which can be picked up only on scans. Combined medical-surgical therapy is the mainstay of treatment. When on antifungal therapy, patient needs to be closely monitored, and timely measures should be taken to keep the adverse effects of antifungals in check without compromising treatment efficacy.
References
Al-Madani MV, Khatatbeh AE, Rawashdeh RZ, Al-Khtoum NF, Shawagfeh NR (2013) The prevalence of orbital complications among children and adults with acute rhinosinusitis. Braz J Otorhinolaryngol 79(6):716–719
Pushker N, Meel R, Kashyap S, Bajaj MS, Sen S. Invasive aspergillosis of orbit in immunocompetent patients: treatment and outcome. Ophthalmology. ;118(9):1886–1891.
Hedges TR, Leung LS (2011) Para sellar and orbital apex syndrome caused by aspergillosis. Neurology. 1976;26(2):117–120.
Soon VTE (2011) Pediatric subperiosteal orbital abscess secondary to acute sinusitis: a 5-year review. Am J Otolaryngol 32(1):62–68
Oxford LE, McClay J (2006) Medical and surgical management of subperiosteal orbital abscess secondary to acute sinusitis in children. Int J Pediatr Otorhinolaryngol 70(11):1853–1861
Chorney SR, Buzi A, Rizzi MD (2021) The role of endoscopic sinus surgery in children undergoing external drainage of Non-Medial Subperiosteal Orbital Abscess. Am J Rhinol&Allergy 35(3):288–295
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest to disclose.
Informed Consent
Informed consent was obtained from the patient.
The authors declare that this manuscript is prepared and submitted only to the Indian Journal of Otolaryngology and Head & Neck Surgery and is not under consideration for publication elsewhere.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chowdhary, S., Jibi, A.M., Rose, W. et al. Aspergillosis Causing Orbital Subperiosteal Abscess in an Immunocompetent Child: A Rare Presentation. Indian J Otolaryngol Head Neck Surg 76, 1088–1091 (2024). https://doi.org/10.1007/s12070-023-04128-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04128-y