Abstract
It is uncommon for bony cervical spine lesions to cause dysphagia. Middle-aged female presented in the outpatient clinic with complaints of dysphagia of insidious onset. Patient’s medical history, clinical manifestation and imaging studies guided the diagnosis of spinal osteoid osteoma. The presentation and surgical management are discussed in this report.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma, first described in 1935, is a benign bone tumor of the growing skeleton [1]. Approximately 10% of these tumours occur in the spine, with cervical spine contributing to 26.8% [2]. The tumor develops from the posterior elements of the spine in majority of the cases and pain is the most commom presenting symptom. We report a case of an osteoid osteoma of C2 wherein dysphagia was the presenting symptom which makes the case even rarer.
Case Report
History
A 50 year-old female presented with a nine month history of dysphagia. The medical history and family history were not contributory. Dysphagia was progressive and was more to solid and semi-solid food than to liquids. She repeatedly consulted her family doctor but was not relieved.
Investigations
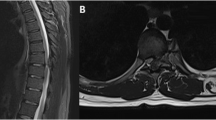
She was then referred to an otorhinolaryngologist who performed a video laryngoscopy (supplementary file) which revealed a swelling causing obstruction in the pharynx from behind. It was decided to further investigate the swelling via a computed tomography (CT), which showed a well defined curvilinear bony lesion measuring 28 × 12 × 5 mm (AP x CC x TR) situated anterior to C1-C2 vertebrae, more toward the right side (Fig. 1a, b). The lesion was seen to be causing mass effect on posterior aspect of oropharynx on the right side. These findings were suggestive of an osteoma. Subsequent magnetic resonance imaging (MRI) of cervical spine confirmed CT findings and the imaging features were considered typical for an osteoid osteoma.
Treatment
Surgery was undertaken after obtaining written informed consent with the intention of excising the lesion through an anterior approach. A plane was developed between the trachea and carotid artery to reach the paravertebral fascia where the lesion was identified and completely excised via drilling. The patient had an uneventful recovery with full range of neck motion. The histopathology report was compatible with the diagnosis. The nidus was well circumscribed and composed of haphazardly inter anastomosing fragments of osteoid tissue. The inter trabecular stroma was loose and fibrovascular. There were numerous scattered osteoclasts and osteoblasts surrounding the osteoid tissue. X-ray taken two months after surgery showed complete resection of the nidus with no signs of recurrence (Fig. 2).
Discussion
Osteoma per se isn’t a rare entity and is encountered frequently in orthopedic and neurosurgical practice but an osteoma at C2 causing dysphagia is rare. The presentation in this case was via a direct mechanical obstruction of esophagus by the expanding lesion. There are only eight cases of C2 osteoma in the literature, and data on C2 osteoma accompanied with dysphagia is scarce. These lesions typically express themselves through local mass effect on neighboring structures and / or cosmetic deformity due to their benign nature and slow growth rate. For such a lesion in cervical region, it can result in spinal cord compression, distorting of the vertebral blood supply, obstruction of the eustachian tube in the case of the upper cervical spine and rarely dysphagia [3].
Any anteriorly placed lesion of cervical spine which compresses the esophagus is bound to present as dysphagia. A systematic review has shown anterior osteophytic bridges connected to underlying pathologies like diffuse idiopathic skeletal hyperostosis (DISH) or ankylosing spondylosis almost exclusively produce dysphagia brought on by bone lesions of the cervical spine [4]. Other causes include protuberance of the anterior atlas, rheumatoid arthritis, ankylosing spondylitis, metastasis, and Forestier’s disease (ossification of the anterior longitudinal ligament [5]. The second most frequent symptom apart from dysphagia is swelling, which is attributed to increased vascular supply to the tumour brought on by prostaglandin production in the nidus.
Upper cervical spine tumors are rare but challenging due to its distinct morphology and proximity to vital structures. Careful dissection, isolation of the lesion and meticulous drilling of bone form the cornerstone of surgical treatment of these cases. Osteoid osteoma excision from the body of C2 through an anterior extraoral approach has been reported previously [6]. An anterior prevascular extraoral technique for the excision of C2 and C3 osteoma has also been described by Laus et al. [7]. Kratimenos and Crockard have also illustrated a far lateral approach to the foramen magnum and high cervical levels [8]. A simple anterior approach sufficed in our case as the lesion wasn’t compressing, encasing or in the vicinity of vertebral artery.
There is much controversy about the pathogenesis of osteoid osteoma. Some authors suggest it is a benign bone tumor, on the other hand, a few state it may represent an inflammatory process or unusual healing. The tumor’s histological resemblance to osteoblastoma and presence of atypical cellular and trabecular components lend credibility to the hypothesis that osteoid osteoma is a benign tumor originating from osteoblasts. Increased number of unmyelinated nerve fibers and blood vessels have been identified within the nidus [9, 10]. These nerve fibres may be responsible for the characteristic pain of this process by release of prostaglandins. Studies have shown that prostaglandin levels are 100 to 1000 times higher than the levels reported in normal bone, causing localised discomfort to the tumor location which typically worsens at night. Also, prostaglandins act on the bradykinin system, exacerbating the pain [9, 10]. Angiography has shown that the lesion is vascular in character. Early arterial phase imaging revealed a tiny feeding artery, and the nidus showed contrast filling.
In conclusion, skeletal benign neoplastic lesions are uncommon where dysphagia is the primary presentation and thus form a crucial yet rare differential diagnoses for pharyngeal dysphagia. Being forewarned is being forearmed.
References
Jaffe RL (1935). Osteiod osteoma: a benign osteoblastic tutor composed of osteoid and atypical bone. Arch Surg. 31:709.
Raskas DS, Graziano GP, Herzenberg JE, Heidelberger KP, Hensinger RN (1992). Osteoid osteoma and osteoblastoma of the spine. J. Spinal Disord. 5:204–211.
Wang W, Kong L, Dong R, Zhao H, Lu Y (2006). Osteoma in the upper cervical spine with spinal cord compression. Eur Spine J S616–20.
Ozgocmen S, Kiris A, Kocakoc E, Ardicoglu O (2002). Osteophyte- induced dysphagia: report of three cases. Joint Bone Spine 69:226–229.
Ilbay K, Evliyaoglu C, Etus V, Ozkarakas H, Ceylan S (2004). Abnormal bony protuberance of anterior atlas causing dysphagia. A rare congenital anomaly. Spinal Cord 42(2):129–131.
Molloy S, Saifuddin A, Allibone J, Taylor BA (2002). Excision of an osteoma from the body of the axis through an anterior approach. Eur Spine J 11:599–601.
Laus M, Pignatti G, Malaguti MC, Alfonso C, Zappoli FA, Giunti A (1993). Anterior extraoral surgery to the upper cervical spine. Chir Organi Mov 78:65–75.
Kratimenos GP, Crockard HA (1993). The far lateral approach for ventrally placed foramen magnum and upper cervical spine tumours. Br J Neurosurg 7:129–40.
Sherman MS, McFarland Jr G. Mechanism of pain in osteoid osteoma (1965). South Med J 58:163–6.
Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma (1993). Clinical, imaging, pathologic, and differential considerations. Skeletal Radiol 22(7):485–500.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to conception and design of the study. PP, AC and SP have been involved in data collection and data analysis. PP, AC, SG, SP, AL and VS have been involved in data interpretation, drafting the manuscript and revising it critically and have given final approval of the version to be published.
Corresponding author
Ethics declarations
Informed Consent
Written informed consent for publication of the clinical details and images was obtained from the patient.
Conflict of interest
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Punia, P., Chugh, A., Gotecha, S. et al. Unusual Presentation of Osteoid Osteoma of the Cervical Spine with Dysphagia: A Case Report. Indian J Otolaryngol Head Neck Surg 75, 2581–2584 (2023). https://doi.org/10.1007/s12070-023-03835-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03835-w