Abstract
To determine the prevalence of anatomical variations of nasal cavity and paranasal sinuses of patients with chronic rhinosinusitis (CRS) on CT scan imaging. To correlate the Anatomical variations with the extent of CRS. 100 patients attending the ENT outpatient department with clinically diagnosed CRS were selected for study based on inclusion and exclusion criteria. Patients were subjected to CT scan and diagnostic nasal endoscopy. The correlation of anatomical variation with severity of CRS based on radiological score and endoscopic score was observed. Deviated nasal septum was the most common anatomical variation observed in 71% cases. Followed by Agger nasi (68%), concha bullosa (55%), Onodi cell (25%), Haller cell (14%), frontal sinus hypoplasia (2%) and uncinate bulla (1%) respectively. Statistically significant relationship of radiological score with left side Bullous Concha Bullosa and highly statistically significant relationship with Haller Cell was observed. While statistically significant relationship between Deviated Nasal Septum on left side with endoscopic score was also observed. Correlation of anatomical variation with CRS concludes on the note that some variations cause impaired sinus drainage and ventilation leading to recurrent sinusitis. Also, incidence of these variations was comparable to other studies done in asymptomatic population therefore, simply detection of a solitary anatomical variant itself does not determine predisposition to disease or the pathogenesis of the CRS and that we should have a critical look out for these anatomical variations from point of view of surgical management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rhinosinusitis is defined by the American Academy of Otorhinolaryngology as—an inflammation of the mucosa of nose and paranasal sinuses. The mucosa throughout the nose and sinuses is continuous and thus inflammation of the nasal mucosa frequently involves the mucous membranes of the sinuses in diseases [1]. Rhinosinusitis can then be further defined as acute or chronic based on duration of symptoms: Acute rhinosinusitis when duration is less than 12 weeks and chronic sinusitis when duration is more than 12 weeks [2]. Diagnosis of Rhinosinusitis is made on clinical grounds that are based on the presence of characteristic symptoms, combined with objective evidence of mucosal inflammation on CT scan and diagnostic endoscopy [3].
Understanding the complex anatomy of Nose and Paranasal sinuses is crucial to know the pathophysiology, make a proper diagnosis and to decide the course of management amongst the patients of CRS. Studies about the relationships between anatomical variations of nose and paranasal sinuses and their possible consequences on nasal permeability and on CRS has been growing in recent years. In this present era of endoscopic sinus surgery and skull base surgery, a thorough knowledge of the precise anatomy and common anatomic variation of the nose and paranasal sinuses and their relationship with the neighboring structures is important for appropriate management of patients with Sino nasal diseases.
However, orientation to these paranasal sinuses remains a challenge among otolaryngologists owing to the anatomical variations and diversity of prevalence among different ethnicities [4].
CT imaging can assess both anatomical variations of the nasal cavity and paranasal sinus as well as extent of the disease. The main role of CT is to provide evidence and support in the diagnosis and management of chronic sinusitis and to define the anatomy of the sinuses prior to surgery. The Task Force on Rhinosinusitis recommends the Lund Mackay staging system to compare the severity of CRS with CT scan findings [5].
Diagnostic nasal endoscopy is a routine component of the clinical evaluation of every patient with evident or suspected disease of the nose and paranasal sinuses. The endoscope helps the examiner to recognize changes that may remain hidden on anterior rhinoscopy. It detects anatomical abnormalities like septal deviation and other inflammatory changes.
The combination of nasal endoscopy and CT scans in the evaluation of CRS allows for precise diagnosis and treatment.
Methods
A cross-sectional study was carried out from August 2018 to January 2021 on 100 patients of either sex, who presented to the OPD of ENT Hospital, Govt. Medical College Amritsar with symptoms pertaining to chronic rhinosinusitis and/nasal polyposis. The patients were selected at random based on a pre-defined inclusion and exclusion criteria. They were first examined clinically and then underwent CT of nose and PNS. This was followed by a diagnostic nasal endoscopy, and the results were correlated.
Inclusion criteria:
-
1.
All adult (≥ 18 years old) of either sex.
-
2.
Clinically diagnosed with CRS who have undergone CT scan.
-
3.
Patients with following clinical symptoms of more than 12 weeks:
-
Chronic nasal discharge.
-
Nasal obstruction.
-
Headache.
-
Postnasal drip.
-
Epistaxis.
-
Anosmia
-
Facial pain.
-
Patients with unilateral/bilateral nasal polyposis.
-
Exclusion criteria:
-
Patients who have undergone prior nasal surgery.
-
Patients diagnosed with malignancy in the paranasal sinus.
-
Patients with distorted nasal anatomy.
-
Craniofacial malformation.
-
Patients under 18 years.
-
Aggressive Fungal infections.
-
Patients with previous history of trauma.
Methodology:
(1) Clinical evaluation was based on-
• Clinical symptoms like:
-
I.
Nasal Obstruction
-
II.
Excessive sneezing
-
III.
Nasal Discharge
-
IV.
PND
-
V.
Sensation of smell
-
VI.
Facial Pain
• Anterior rhinoscopy findings:
-
I.
Condition of nasal mucosa
-
II.
Discharge
-
III.
Nature of discharge (if present)
-
IV.
Nasal Septum deviation
-
V.
Condition of turbinates
-
VI.
Other findings-Polyp
(2) Radiological evaluation:
In all patients of CRS/nasal polyposis, Non-contrast CT scan of Nose and paranasal sinuses was done with 3 mm cut sections and severity of CRS was evaluated based on Lund-Mackay score (0: no opacity, 1: partial opacity, 2: total opacity) The ten scores for the various sinuses and bilateral osteomeatal complexes were summed to give a bilateral total LMS that could range from 0 (complete lucency of all sinuses) to 24 (complete opacification of all sinuses).
On CT scan anatomical variations visualized were accessed and check list filled with regard to the plane and side, whether it was left or right.
(4) Diagnostic nasal endoscopic evaluation: After radiological evaluation all the patients were subjected to diagnostic nasal endoscopy.
Endoscopic staging as proposed by Lund-Kennedy to assess the following parameters was done:
-
Nasal mucosal edema (0: absent, 1: minimal, 2: gross).
-
Presence of secretion (0: absent, 1: thin, 2: purulent).
-
Presence of polyps (0: absent, 1: present in meatus, 2: present in nasal cavity but not obstructing airway, 3: present in nasal cavity with obstruction of airway).
Results
A total of 100 patients were included in the study. The most affected age group in our study was of 21–40 years with 74% cases and the mean age was 33.92 years. Male to female ratio of 1:1.56.
In our study, nasal obstruction was the most common complaint in 97% cases. Followed by nasal discharge (94%). Other symptoms were postnasal discharge (74%), headache (63%), excessive sneezing (44%), facial fullness (32%) and hyposmia (25%) Table 1.
In terms of prevalence, deviated nasal septum was the most common anatomical variation seen in 71%. Followed by Agger nasi (68%), concha bullosa (55%), Onodi cell (25%), Haller cell (14%), frontal sinus hypoplasia (2%) and uncinate bulla (1%) respectively. No cases of maxillary sinus hypoplasia and sphenoid sinus hypoplasia were seen during this study. Sphenoid sinus was pneumatized in all the cases with pre-sellar type pneumatization in 3% cases and sellar type in 97% cases Table 2.
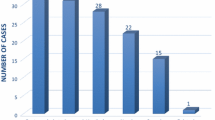
Regarding the CT findings for the sinuses and polyp, the Lund Mackay Radiological scoring was followed. In our study Frontal sinus was reported normal in 61% cases on left and 70% cases on right side, partially opacified in 38% on left side and 30% on right side and completely opacified in 1% on left side. Maxillary sinus was reported to be normal in 8% on left side and 21% on right side, partially opacified in 84% and 71% on left and right side respectively, and completely opacified in 8% each on left and right side. Anterior ethmoids were reported as normal in 45% and 47% on left and right side respectively, partially opacified in 53% and 52% on left and right side and completely opacified in 2% and 1% on left and right side respectively. Posterior ethmoids were normal in 68% on left and 65% on right side, partially opacified in 22% on left and 25% on right and completely opacified in 10% each on left and right side. Sphenoid sinus was reported to be normal in 68% on left side and 66% on right side respectively, partially opacified in 30% on left and 33% on right and completely opacified in 2% on left and 1% on right side. Osteomeatal complex was found to be normal in 84% cases on left and 83% cases on right side and occluded in 16% on left and 17% on right side. According to this Lund Mackay Radiological Score depicting the extent of disease patients were divided into three groups i.e. group I, group II and group III. 75% patients fall in group I i.e. patients having score from 0 to 8.24% of the patients were having score of 9–16 in group II and only 1 patient falls in group III having score between 17 and 24 (Fig. 3). Correlation between Various anatomical variations and Lund MacKay radiological score was observed. According to our study there was statistically significant (p < 0.05) relationship between left side Bullous Concha Bullosa with this Lund Mackay Radiology Score. And there was high statistically significant (p = 0.001) relationship present between Haller Cell and Lund Mackay Radiological score. However, according to our study no statistically significant (p > 0.05) relationship was found to be present between Lund Mackay Radiological score with any other variation Table 3.
Endoscopy grading of CRS was done based on Lund Kennedy Endoscopy score. No polyposis was seen in 92% cases on both sides. Grade 1 polyposis (polyp confined to middle meatus) was present in 4% cases on left side and in 1% cases on right side. Grade 2 polyposis (polyp beyond middle meatus but not completely obstructing the nose) was evident on left side in 1% cases and Grade 3 polyposis (polyp completely obstructing the nose) was found only in 2% cases on left side (Fig. 1). No oedema was present in 28% cases on left side and 31% cases on right side. Grade 1 (mild) oedema was present in 61% cases on left side and 57% cases on right side. Grade 2 (severe) oedema was present in 11% cases on left side and 12% cases on right side. There was no discharge in 5% cases on left side and 10% cases on right side. Clear and thin discharge (Grade 1) was present in 83% cases on left side and 84% cases on right side and thick and purulent (Grade 2) discharge was present in 12% and 6% cases on left and right side respectively. According to endoscopic grading division of patients into two groups was done i.e. Group I and Group II according on Lund Kennedy Endoscopic Score depending upon the endoscopic findings (Fig. 3). 97% patients fall under group I i.e., patients having score from 0 to 7 and 3% patients under group II i.e. patients having score from 7 to 14. According to our study Deviated Nasal Septum on left side had statistically significant relationship with Lund Kennedy Endoscopic Score i.e. (p < 0.05). There was no statistically significant (p > 0.05) relationship between other variations and Lund Kennedy Endoscopic Score Table 4.
Discussion
Chronic Rhinosinusitis (CRS) is one of the most prevalent chronic illness in India, affecting persons of all age groups and has also been reported worldwide with increasing incidence in the last few decades. However, its diagnosis and treatment is still a challenge to clinician. There are numerous studies regarding pathogenesis of CRS due to the anatomical variations. Some of the anatomic variants have been reported to be related with CRS, probably leading to inflammation by blocking drainage pathways of the sinuses and nasal cavity. The gold standard in the evaluation of these variations and its relationship with CRS is now the Computed tomography (CT) scanning of the paranasal sinuses and is thought to be an integral component in the diagnosis of CRS. Many attempts have been made to establish standardized staging systems of CT scan and diagnostic endoscopic evaluation to assess the severity for objective identification and quantification of CRS.
Our study included 100 patients from the OPD of ENT Department. The most affected age group in our study was of 21–40 years with 74% cases and the mean age was 33.92 years. In a study done by Rajeev et al. [6] in 2018 the mean age of presentation was 38.4 years.
On comparing clinical symptoms nasal obstruction was the most common complaint in 97% cases. Followed by nasal discharge (94%). Other symptoms were postnasal discharge (74%), headache (63%), excessive sneezing (44%), facial fullness (32%) and hyposmia (25%). Also, in a study done by Bakari et al. the main presenting symptoms were nasal blockage and rhinorrhea. In our study hyposmia was the least common symptom andwas present in 25% patients which according to a study by Bakari et al. [7] was present in 36% cases.
In terms of prevalence, deviated nasal septum was the most common anatomical variation seen in 71%. Followed by Agger nasi (68%), concha bullosa (55%), Onodi cell (25%), Haller cell (14%), Frontal sinus hypoplasia (2%) and Uncinate bulla (1%). No case of maxillary sinus hypoplasia and sphenoid sinus hypoplasia was seen during our study. Sphenoid sinus was pneumatized in all the cases with pre-sellar type pneumatization in 3% cases and sellar type in 97% cases. Similarly, the most common anatomical variant in a study done by Shrestha et al. [8] was DNS, occurring in 64.5% patients. This was also comparable to the absolute frequencies of DNS in other study done by Sharma et al. [9] 68%. The second most common variation in our study was Agger Nasi, seen in 68% patients. This was almost similar to study done by Shokri et al. [10] in 2019 in which prevalence of Agger Nasi was found to be 53.6%. Agger cells can obstruct the frontonasal outflow tract causing frontal sinusitis. The third most common variation in our study was concha bullosa, seen in 55% patients (Fig. 2). Presence of concha bullosa is believed to block the osteomeatal complex (OMC) and limits the exposure of surgical field. However, the correlation of concha bullosa and CRS continues to be debated. The literature has reported the prevalence of concha bullosa in a wide range; from 5 to 8% in a study by Kayalioglu et al. [11] to as high as 98.5% in a study by Bolger et al. [12]. This discrepancy in the incidence of concha bullosa not only occurs among the CRS patients but also in the normal population. This may be due to genetic difference among different races, and perhaps the definition for pneumatization may vary among different investigators. In our study, we found Onodi cell in 25% patients which was fourth most common variation in our study. Onodi cells are posterior ethmoid cells that extend to the sphenoid sinus, lying medial to the optic nerve. If Onodi cell is present, the surgeon should be extra careful during posterior ethmoidectomy because of neighboring optic nerve. In a similar study done by Shokri et al. [10] frequency of Onodi cell was found to be 37.2%. We observed Haller cell in 14% patients. In a study done by Shokri et al. [10] prevalence of Haller cell was 28.8%. In our study, frontal sinus hypoplasia was present in 2% cases which was similar to a comparative study done by Singh et al. [13] in which frontal sinus hypoplasia was seen in 3% cases. In our study frequency of presence of uncinate bulla was 1%. In a study done by Azila et al. [14] frequency of uncinate bulla was 3.3%. According to a study by Bolger et al. [12] it was found in 2.5% cases. In our study no cases of maxillary sinus hypoplasia and sphenoid sinus hypoplasia were seen. Maxillary sinus aplasia and hypoplasia are rare conditions which was present in 1.43% cases according to a study done by Bolger et al. [12]. In our study no conchal type sphenoid sinus pneumatization was seen, pre-sellar type pneumatization was seen in 3% cases and sellar type in 97% cases. According to a study done by Hiremath et al. in 2018 on assessment of variations in sphenoid sinus pneumatization in Indian population there were no patients with conchal type, 1.2% of patients werewith pre-sellar type, and 76.6% of patients with a complete sellar type of pneumatization [15] (Fig. 3).
Showing A Uncinate bulla (orange arrow) left side on coronal section, B Onodi cell (yellow arrow) on coronal section, C Concha Bullosa (blue arrow) (bullous type) on Sagittal section of CT nose and PNS, D Concha Bullosa (blue arrow) (bullous type) on coronal section of CT nose and PNS, E DNS with spur indenting inferior turbinate (white arrow) on left side on coronal section
A Depicts the division of patients into two groups i.e., group I and group II according on Lund Kennedy Endoscopic Score depending upon the endoscopic findings. B Depicts the division of patients into three groups i.e., group I, group II and group III according to Lund Mackay Radiological Score depending upon the CT Scan findings
In our study endoscopy grading of CRS was done based on Lund Kennedy Endoscopy score the results of which are tabulated below in Table 4. Results were similar to a study conducted by Deosthale NV to study the effectiveness of CT and nasal endoscopy, on clinical examination, congested nasal mucosa was seen in 45.08%, bilateral inferior turbinate hypertrophy in 48.36%, deviated nasal septum in 37.70%, edematous nasal mucosa in 31.14%, non-purulent nasal discharge in 25.40%, pale nasal mucosa and polyps were seen in 15.57% [16].
Correlation between Various anatomical variations and Lund Kennedy Endoscopic Score was observed and there was statistically significant relationship between Deviated Nasal Septum on left side with endoscopic score. Findings were similar to a study conducted by Fadda et al. [17] in which they observed statistically significant relationship between left nasal deviation with endoscopic score. Similar results were seen in study done by Rajeev et al. However, there was no statistically significant (p > 0.05) relationship between Deviated Nasal Septum on right side and Lund Kennedy Endoscopic Score [6]. This difference in results between left and right sided DNS may be due to left sided deviation being more common in our study and the smaller sample size. There was no statistically significant (p > 0.05) relationship between other variations and Lund Kennedy Endoscopic Score.
In our study Radiological scoring of CRS was done based on Lund MacKay radiological score the results of which are tabulated in Table 3. In a study done by Nabil et al. on CT reporting, maxillary sinus was found to be normal in 15% cases, partially opacified in 45% cases and completely opacified in 40% cases. Anterior ethmoids were normal in 15% cases, partially opacified in 35% cases and completely opacified in 50% cases. Posterior ethmoids were normal in 15% cases, partially opacified in 20% cases and completely opacified in 60% cases. The frontal sinus was normal in 40% cases, partially opacified in 30% cases and completely opacified in 30% cases. The sphenoid sinus was found to be normal in 35% cases, partially opacified in 35% cases and completely opacified in 30% cases [9].
On correlation of anatomical variations with radiology score it was observed that there was statistically significant relationship with left side Bullous Concha Bullosa and highly statistically significant relationship with presence of Haller Cell. Similar findings were seen in study conducted by Tiwari R and Goyal R where significant relationship was present between Concha Bullosa and Radiological score [18]. Rajeev et al. [6] observed highly significant relationship between Haller cell and Radiological score. However, according to our study no significant statistical (p > 0.05) relationship was found to be present between other anatomical variations and Lund Mackay Radiological score. In contrast to a study done by Hasan et al. [19] according to which the prevalence of septal deviation, was 72.7% in study group i.e. with sinusitis and 47.7% in control group i.e. without sinusitis which is statistically significant. These results differ from our study because in our study only the diseased patients were taken and there was no control group. It may also be due to the smaller sample size as compared to other study. Whether these were congenital or developmental, as commonly DNS is developmental these mild deviations were not causing obstruction significantly in our study but can definitely be blamed as one of the etiological factor in CRS.
Conclusion
Our study concludes that clinical examination gives a gross picture of the underlying disease which puts down the groundwork for subsequent management options. We also observed that CT proved to be of utmost importance in study of anatomy of the nasal cavity and paranasal sinuses and extent of disease. Nasal endoscopy is a valid and objective diagnostic tool in the work up of patients with CRS. In terms of correlation of these variation with CRS our study concludes that anatomical variations can cause impaired sinus drainage and ventilation leading to recurrent sinusitis. Considering the results obtained in our study, incidence of these variations was comparable to other studies done in asymptomatic population therefore, simply detection of a solitary anatomical variant itself does not determine predisposition to disease or the pathogenesis of the CRS and that we should have a critical look out for these anatomical variations from point of view of surgical management.
The limitations of the study:
-
1.
Asymptomatic cases was not taken into consideration to compare with the diseased group.
-
2.
Sample size used in our study was small.
-
3.
Patients with extensive disease were excluded, as it was not possible to visualize anatomical variations in such patients due to distorted anatomy.
Recommendation:
-
1.
Similar study may be carried out with larger study sample and more diverse population.
-
2.
Asymptomatic cases may be taken as control group.
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- CRS:
-
Chronic rhinosinusitis
- CT:
-
Computed tomography
- DNE:
-
Diagnostic nasal endoscopy
- LMS:
-
Lund MacKay score
- LKS:
-
Lund Kennedy score
References
Report of the Rhinosinusitis Task Force Committee Meeting (1997) Alexandria, Virginia. Otolaryngol Head Neck Surg 117:1–68
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I (2015) Clinical practice guideline (update): adult sinusitis. Otolaryngol Head and Neck Surg 152(Supp. 2):S1–S39
Steinke JW, Bradley D, Arango P, Crouse CD, Frierson H, Kountakis SE et al (2003) Cysteinyl leukotriene expression in chronic hyperplastic sinusitis-nasal polyposis: importance to eosinophilia and asthma. J Allergy Clin Immunol 111(2):342–349
Keast A, Sofie Y, Dawes P, Lyons B (2008) Anatomical variations of the paranasal sinuses in Polynesian and New Zealand European computerized tomography scans. Otolaryngol Head Neck Surg 139(2):216–21
Lund VJ, Mackay IS (1993) Staging in rhinosinusitis. Rhinology 107:183–184
Rajeev K, Ravishankara S, Chethana CS, Shenoy SB et al (2018) Anatomical variations of maxillary and ethmoid sinus in chronic rhinosinusitis. Int J Otorhinolaryngol Head Neck Surg. 4(4):1008–1012
Bakari A, Afolabi OA, Adoga AA, Kodiya AM, Ahmad BM (2010) Clinicopathological profile of sinonasal masses: an experience in national ear care center Kaduna, Nigeria. BMC Res Notes 3(1):186
Shrestha KK, Acharya K, Joshi RR, Maharjan S, Adhikari D (2019) Anatomical variations of the paranasal sinuses and the nasal cavity. Nepal Med Coll J 21(1):7–11
Sharma BN, Panta OB, Lohani B, Khanal U (2015) Computed tomography in the evaluation of pathological lesions of paranasal sinuses. J Nepal Health Res Counc 13:116–121
Shokri A, Faradmal MJ, Hekmat B (2019) Correlations between anatomical variations of the nasal cavity and ethmoidal sinuses on cone-beam computed tomography scans. Imaging Sci Dent 49(2):103–113
Kayalioglu G, Oyar O, Govsa F (2000) Nasal cavity and paranasal sinus bony variations: a computed tomographic study. Rhinology 38(3):108–113
Bolger WE, Parsons DS, Butzin CA (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 101(1):56–64
Singh S, Garg AK, Veereddy N (2019) A comparative study of anatomical variations in nose and paranasal sinuses to establish the etiological basis of chronic rhinosinusitis. MedPulse Int J ENT 9(1):26–32
Azila A, Irfan M, Rohaizan Y, Shamim AK (2011) The prevalence of anatomical variations in osteomeatal unit in patients with chronic rhinosinusitis. Med J Malays 66(3):191–194
Hiremath SB, Gautam AA, Keerthy Sheeja GB (2018) Assessment of variations in sphenoid sinus pneumatization in Indian population: a multidetector computed tomography study. Indian J Radiol Imaging 28(3):273
Deosthale NV, Khadakkar SP, Singh B, Harkare VV, Dhoke PR, Dhote KS (2014) Anatomical variations of nose and paranasal sinuses in chronic rhinosinusitis. People’s J Sci Res 7(2):1–7
Fadda GL, Rosso S, Aversa S, Petrelli A, Ondolo C, Succo G (2012) Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. ACTA Otorhinolaryngol Italica 32(4):244
Tiwari R, Goyal R (2015) Study of anatomical variations on CT in chronic sinusitis. Indian J Otolaryngol Head Neck Surg 67(1):18–20
Hasan OA, Hassan MA, Fawzy EK, Maarouf AM (2017) Anatomical variations of nasal structures in chronic rhinosinusitis as detected by computed tomography scan. Egypt J Hosp Med 68(3):1390–1394
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethics approval
Approved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhagat, R., Maan, A.S., Sharma, K.K. et al. Combined Radiological and Endoscopic Evaluation of Sino Nasal Anatomical Variations in Patients of Chronic Rhinosinusitis: A North Indian Study. Indian J Otolaryngol Head Neck Surg 75, 2155–2162 (2023). https://doi.org/10.1007/s12070-023-03814-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03814-1