Abstract
The most common cause of nasal obstruction is a deviated nasal septum. It causes breathing difficulties and may eventually also cause sinusitis, epistaxis, sleep disturbances and snoring. The traditional surgeries of the nasal septum improve the nasal airway but do not fulfil the essential criteria in most instances. Endoscopic septoplasty is a fast-developing concept and gaining popularity as it provides a direct targeted approach to the septal anatomic deformity allowing a minimally invasive procedure under excellent visualization. The aim of this study is to compare the post-operative morbidity among conventional and endoscopic septoplasty. The present prospective study was conducted on 50 patients having deviated nasal septum. Patients were randomly divided into two groups of 25 each. Out of 50 patients, in 25 patients (Group A) Conventional septoplasty was done, whereas in other 25 patients (Group B) endoscopic septoplasty was done. The patients were followed up post-operatively at 2 weeks, 4 weeks and 8 weeks. Study Design: comparative study. The mean of operating time (min) in Group A was 60.47 ± 8.16 which was significantly higher as compared to Group B (39.7 ± 6.73). (p value < .0001). The Mean of blood loss (mL) was significantly higher in Group A (88.67 ± 8.77) as compared to Group B. (54.6 ± 7.18). (p value < .0001). Post-operative NOSE score at one month was 7.33 ± 1.5 in group A which was significantly higher as compared to Group B (5 ± 1.41). (p value = 0.0007) whereas post-operative NOSE score at 3 months in Group A was 6.53 ± 1.25 which was significantly higher as compared to Group B (4.4 ± 1.78). Proportion of post-operative complications was comparable in Group A and Group B (No complication 80% vs. 92% respectively). According to the present study, both the conventional and endoscopic septoplasty procedures were effective in relieving nasal obstruction in the patients. Endoscopic septoplasty showed significantly better result than conventional septoplasty in terms of time taken for surgery, blood loss during the surgery, post-operative complications and in terms of quality of life as assessed by NOSE Score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The most common complaint in rhinologic practice is nasal obstruction, and the most common cause of nasal obstruction is a deviated nasal septum. It not only causes breathing difficulties but also results in improper aeration of paranasal sinuses predisposing to sinusitis and also resulting in drying of mucosa leading to crusting and epistaxis. It can also be accompanied with hypertrophic nasal turbinates causing sleep disturbances and snoring. It can also be implicated in headaches attributable to contact points with structure of lateral nasal wall [1]. The evaluation of a septal deviation causing nasal obstruction depends on physical examination and imaging [2]. Each surgical procedure has its limitations and cannot deal with all the variants of the deformities of nasal septum. An ideal surgical correction of the nasal septum should satisfy the following criteria [3]:should relieve the nasal obstruction
-
(b) should be conservative
-
(c) should not produce iatrogenic deformity
-
(d) should not compromise the osteo-meatal complex
-
(e) must have the scope for a revision surgery if required, later
The traditional surgeries of the nasal septum improve the nasal airway but do not fulfil the above-mentioned criteria in most instances. The reasons being poor visualization, relative inaccessibility, poor illumination, difficulty in evaluation of the exact pathology, need for nasal packing, unnecessary manipulation, resection and overexposure of the septum framework reducing the scope for a revision surgery if required later. Earlier sub-mucus resection of the septum was done which was a radical surgery and was associated with lot of complications. Now a days, septoplasty is the standard treatment offered for symptomatic deviated nasal septum which is conventionally performed under direct visualization using a headlight and a nasal speculum.
Endoscopic septoplasty is a fast-developing concept and gaining popularity as it provides a direct targeted approach to the septal anatomic deformity allowing a minimally invasive procedure under excellent visualization with limited septal mucosal flap dissection and removal of a small cartilaginous and/or bony deformity. More than one incision can be given to correct the deformities on the either side of the nasal septal mucosa. Better light illumination and magnification provided by the endoscope helps to increase the precision of the surgical procedure. Endoscope aids limited but sufficient exposure of septal pathology and there is no need for the disarticulation of ethmoido-chondral and vomero-chondral junctions [4].
Despite several benefits endoscopic septoplasty can be difficult because of frequent soiling of lens of the endoscope by blood and difficulty in finding enough space for endoscope in narrow septal mucosal tunnels [5]. Also complex deformities of the septum and anterior septal deviations were tedious to be managed by endoscopic septoplasty. The selection of best method for correction of deviated nasal septum is still controversial; therefore, the objective of our study was to compare the post-operative morbidity among conventional and endoscopic septoplasty using nose scale.
Methods
The study was conducted in the Tertiary Care Centre w.e.f November 2019 to October 2020 after taking approval of Institutional Ethical committee of GMC Jammu.
The patients attending the ENT Outpatient Department, with symptomatic deviated nasal septum in the age range of 17 to 60 years who were willing and were fit to undergo surgery were included in the study.
Exclusion Criteria included age less than 17 years, patients undergoing septoplasty along with other nasal pathology, patients not willing for surgery or not fit for surgery.
Informed consent was obtained.
Detailed history of the patient was taken.
Patients symptoms were assessed using NOSE scale [6] (Table 1).
Detailed evaluation of the patient including complete ear, nose and throat examination including Diagnostic Nasal Endoscopy was done to classify the deviation of nasal septum as anterior (localised to anterior quadrilateral cartilage), posterior (bony) or combined deviation.
Routine investigations of the patient were done.
Non contrast computed tomography of Nose and PNS was done for any concomitant disease.
Any other relevant investigation if and when required was done.
Patients were divided into two groups depending on the type of surgical procedure performed. Group A patients underwent Conventional septoplasty (n = 25) and group B patients underwent Endoscopic septoplasty (n = 25).
Surgical Procedures
-
(a) Conventional septoplasty
-
(b) Endoscopic septoplasty
Technique for Conventional Septoplasty [7]
The surgery was performed either under LA (Local anaesthesia) or GA (General anaesthesia). Bilateral nasal decongestion was done using 4% lignocaine with adrenaline 10 min prior to surgery. Under head light vision, after infiltration with 2% lignocaine with adrenaline (1:200,000) into the septum, a vertical hemi-transfixation incision was made 2–3 mm from the caudal end of septum on concave side along the entire height of septum. Mucoperichondrial and mucoperiosteal flap were raised; anterior and inferor tunnels were created and then united. The deviated part of the septum; bony as well as cartilaginous was removed. Incision was sutured with catgut (3–0) and nasal cavities packed with medicated nasal pack.
In case of caudal dislocation needing correction, a complete transfixation incision was made. Here the mucoperichondrial flaps were elevated on both sides of the caudal septum and the deviation was accordingly shortened in the most caudal aspect of caudal strut. The caudal strut was then secured to the columella (where a small tunnel was created by sharp dissection) with 4–0 vicryl sutures and the transfixation incision was closed meticulously.
Procedure for Endoscopic Septoplasty [4]
The procedure was done under GA or LA. The rigid endoscopes (0 degree and 30 degrees with 4 mm diameter) were used for the procedure. Xylocaine 2% with adrenaline infiltration were given on both sides just anterior to deviation. An incision caudal to the deviation on the convex side was made roughly parallel yet cephalic to the classically described hemi-trans fixation incision. Mucoperichondrial/ mucoperiosteal flap was raised and deviation whether, cartilaginous or combination was visualized. If the deviation was bony, the incision was made at the bony cartilaginous junction. Mucoperichondrial/mucoperiosteal flap on the opposite side was raised. The deviation was excised using Tru cut forceps/Luc’s forceps. For septal spurs, an ipsilateral incision was given parallel to the floor of the nose on the apex of the spur. An osteotome was then seated against the base of the spur and used to remove the bony protrusion. Additional remnants of spur were trimmed with cutting endoscopic forceps. Then flaps were restored to their native position. Nasal cavity was packed with small sized merocele packs.
Intraoperative parameters in both surgeries like; operative time taken, blood loss and problems encountered during the procedure were noted. Postoperatively, nasal packs were removed after 48–72 h and all the patients were followed up at 2 weeks, 4 weeks, and 8 weeks and complications if any like haematoma, perforation, synechiae and crusts were noted.
Post-operatively NOSE scale was evaluated at 1 and 3 months post-surgery.
Statistical Analysis
All the collected data was entered in the Microsoft excel sheet and then analysed using computer software Open Epi (version 3) for window. The qualitative data and quantitative data were reported as proportions and mean (± SD), respectively. t-test was used to test the association. A p-value less than 0.05 was considered as significant. All p-values were two tails.
Results
The study was conducted in the Department of Otorhinolaryngology & Head and Neck surgery, SMGS hospital GMC Jammu from November 2019 to October 2020. 25 patients of age > 17 years and < 60 years presenting with symptomatic deviated nasal septum were included in the study. Patients were randomly divided into two groups who underwent Conventional septoplasty (n = 25) and those who underwent Endoscopic septoplasty (n = 25). Group A (Conventional)—Out of 25 patients, 12 patients had anterior deviation, 9 patients had posterior deviation and 4 patients had combined anterior–posterior deviation.
Group B(Endoscopic)—Out of 25 patients, 15 patients had anterior deviation, 8 patients had posterior deviation and 2 patients had combined anteroposterior deviation.
The mean age of the patients was 25.4 + − 9.45 years with a range of 18–55 years and male to female ratio was 3:10.
The main presenting complaint was of nasal obstruction in 46 (92%) patients. 2(4%) patients presented with nasal obstruction along with nasal discharge and other 2(4%) presented with nasal discharge along with sneezing.
The mean of operating time(minutes) in Group A was 60.47 ± 8.16 which was significantly higher as compared to Group B (39.7 ± 6.73). (p value < 0.0001) (Table 2).
The Mean of blood loss (mL) was significantly higher in Group A (88.67 ± 8.77) as compared to Group B. (54.6 ± 7.18). (p value < 0.0001) (Table 3).
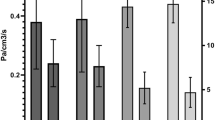
The mean pre-operative NOSE score in conventional septoplasty was 11.2 ± 2.24 and endoscopic septoplasty was 10.6 ± 1.71 with no significant difference between two groups. (p value = 0.48). Post-operative NOSE score at one month was 7.33 ± 1.5 in group A which was significantly higher as compared to Group B (5 ± 1.41). (p value = 0.0007) whereas post-operative NOSE score at 3 months in Group A was 6.53 ± 1.25 which was significantly higher as compared to Group B (4.4 ± 1.78). (p value = 0.001) (Table 4).
Proportion of post-operative complications at 1 month and 3 months was comparable in endoscopic septoplasty and conventional septoplasty and it was insignificant statistically. The incidence of post-operative complications at one month follow up was comparable in both groups. 20 (80%) subjects in group A and 23 (92%) subjects in group B developed no complication, 2 patient (8%) among group A subjects presented with epistaxis, 2 patients (8%) in group A and 2 patient (8%) in group B had residual septal deviation, synechiae was seen in 1 patient (4%) in group A. No patient in either group developed septal perforation, septal abscess/ haematoma or supra-tip depression. At two months follow up, the post-operative complications were almost similar to those at 1 month with no case of epistaxis, in addition to one case who developed post nasal drip in group B (Table 5).
Discussion
Deviated nasal septum is very common entity encountered in ENT practice but is mostly asymptomatic. In case of deviated nasal septum causing symptoms, septal surgery is the treatment of choice. In 1990, sub-mucus resection was the surgical procedure done for the correction of deviated nasal septum. Several modifications were done by Metzenbaum (1926) [8], Galloway [9], Cottle et al. [10] and septoplasty became the preferred surgery later. It is conventionally performed under direct visualization using a headlight and a nasal speculum. The drawbacks of relatively poor illumination and inaccessibility and no magnification calls for a larger incision and elevation of larger flaps often on both sides of the septum and hence resulting in higher chances of over-resection and over manipulation.
In 1978 there was advent of nasal endoscopic surgery, and in 1991, Lanza et al. [11] and Stammberger [12] described the application of endoscopic techniques for correction of septal deformities. Early rep orts of endoscopic septoplasty describe several advantages associated with the technique, including easy visualization of tissue planes and a better way to treat isolated septal spurs.
Age and Sex Distribution
In the present study of 25 subjects, majority of subjects were in the age group 19–31 years, with majority of conventional septoplasty (group A) subjects in the age group 18–31 years and endoscopic septoplasty (group B) subjects in age group 21–31 years. The mean age of the patients was 25.4±9.45 years with a range of 18–55 years. The findings of the present study were similar to the study conducted by Gupta [3] and Bajwa et al. [13] where the most common age group was third decade. Similar findings were seen in the studies conducted by Jain et al. [14] and Rao et al. [15].
In the present study, there were 19 (76%) males and 6 (24%) females with male-to-female ratio of 3:1.. Sathyaki et al. [16] conducted a study on 50 patients with 38 males (76%) and 12 females (24%), and the findings were also similar to the present study.
Presenting Complaints
Nasal obstruction was the main presenting complaint in all the 25 (100%) patients. It was the only presenting complaint in 23 (92%) patients, in 1 (4%) it was associated with nasal discharge (4%) and in the other 1 patient (4%) it was associated with sneezing. The findings of the present study were consistent with the studies conducted by Sathyaki et al. [16] and Suraneni et al. [17] where all the patients presented with chief complaint of nasal obstruction.
Operating Time and Intra-operative Blood Loss
In the present study, the mean operating time taken for patients in group A was 60.47 ± 8.16 min and Group B was 39.7 ± 6.73 min. Operating time (min) in Group A was higher as compared to group B. It was statistically significant (p value < 0.0001). The mean Intra operative blood loss in the group A patients was 88.67 ± 8.77 ml while in the group B it was 54.6 ± 7.18 ml. Thus, the blood loss in group A was significantly higher as compared to Group B (p value < 0.0001).
These findings were similar to the study conducted by Mandal and Jana [18] where the mean time taken for conventional septoplasty was higher and the difference was statistically significant. Intra-operative average blood loss (in mL) in conventional septoplasty subjects was also higher as compared to endoscopic septoplasty group.
Giles et al. [19] also reported in his study that endoscopic septoplasty took relatively shorter time as compared to traditional septoplasty in patients with limited deviation of nasal septum.
On contrary to findings of the present study, Singh et al. [7] reported that the mean time taken (in min) for conventional septoplasty was lesser as compared to endoscopic septoplasty. Intra-operative average blood loss (mL) in the conventional septoplasty subjects was also lesser than endoscopic septoplasty group.
NOSE Score Findings
In the present study, Mean Pre-operative NOSE Score in group A was 11.2 ± 2.24 and group B was 10.16 ± 1.71 with no significant difference between two groups. At month follow-up, mean post-operative NOSE Score in Group A was 7.33 ± 1.5 and in group B was 5 ± 1.41.The difference was statistically significant (p value = 0.0007). At 2 months follow-up, mean post-operative, NOSE score in Group A was 6.53 ± 1.25 and in Group B was 4.4 ± 1.78; which was significantly higher in Group A as compared to Group B (p value = 0.001), indicating that endoscopic septoplasty group had better relief of symptoms and functional outcome as compared to conventional septoplasty group.
These findings were similar to a study conducted by Singh et al. [7] where there was subjective improvement after surgery. The mean Pre-operative nose score in conventional septoplasty and endoscopic septoplasty group was 16.38 and 17 respectively, which declined post-operatively to 4.18 and 1.23 respectively. There was significant improvement in both the groups. Decline in mean NOSE score was significantly higher in endoscopic septoplasty group.
The findings of present study were similar to the study conducted by Sheriff et al. [20], who reported a significant decline in NOSE score post-operatively, from 10.7 ± 4 to 4.7 ± 4.3 in the endoscopic septoplasty group and, 10.5 ± 3.5 to 6.4 ± 2.8 in the conventional septoplasty group. Decline in mean NOSE score was comparatively higher in endoscopic septoplasty group as compared to the conventional septoplasty group, which was highly significant statistically.
On contrary to the present study, Paradis et al. [21] in their study on 63 patients reported that there was no significant statistical difference between the two groups. Although, both endoscopic and conventional septoplasty were found to be effective in improving the mean score of the patients.
Post-operative Complications
In the present study, the incidence of post-operative complications at one month follow up was comparable in both groups. 20 (80%) subjects in group A and 23 (92%) subjects in group B developed no complication, 2 patient (8%) among group A subjects presented with epistaxis, 2 patients (8%) in group A and 2 patient (8%) in group B had residual septal deviation, synechiae was seen in 1 patient (4%) in group A. No patient in either group developed septal perforation, septal abscess/ haematoma or supra-tip depression. At two months follow up, the post-operative complications were almost similar to those at 1 month with no case of epistaxis, in addition to one case who developed post nasal drip in group B.
In a study conducted by Bothra and Mathur [22] it was found that residual septal deviation was more in endoscopic septoplasty group (15%) as compared to the conventional septoplasty group (10%). In contrast to the present study, in this study there were more cases of synechiae in endoscopic septoplasty group (25%) as compared to conventional septoplasty group (5%).
On contrary to our findings, in a study conducted by Gulati et al. [4], it was found that cases of residual septal deformity were more in conventional septoplasty group (20%) as compared to endoscopic septoplasty group (8%), and in a study conducted by Mandal and Jana [18], there were 40% cases of residual septal deviation in conventional septoplasty group and 6.7% in endoscopic septoplasty group. Sathyaki et al. [16] conducted a study where there were no synechiae post-operatively in endoscopic septoplasty group and 16% patients had synechiae in conventional septoplasty group, and these findings are consistent with the present study.
Endoscopic technique is performed with minimal incision and better illumination leading to less operative time and blood loss. Also, although statistically insignificant, endoscopic septoplasty had fewer complications than conventional septoplasty in our study, which could be due to direct visualisation and minimal manipulation with the aid of endoscope.
Conclusion
According to the present study, both the conventional and endoscopic septoplasty procedures were effective in relieving nasal obstruction in the patients. Endoscopic septoplasty, however, had few drawbacks like frequent soiling of lens of the endoscope by blood during surgery and difficulty in correcting complex deformities. Anterior deviations could be corrected faster and with lesser difficulty by conventional septoplasty procedure while posterior deviations were dealt more precisely with endoscopic technique. Endoscopic septoplasty showed significantly better result than conventional septoplasty in terms of time taken for surgery, blood loss during the surgery, post-operative complications and quality of life as assessed by NOSE Score.
Availability of Data and Material
Available with corresponding author upon reasonable request.
References
Pannu KK, Chadha S, Kaur IP (2009) Evaluation of benefits of nacsal septal surgery on nasal symptoms and general health. Indian J Otolaryngol Head and Neck Surg 61(1):59–65
Dinis PB, Haider H (2002) Septoplasty-long term evaluation of results. Am J Otolaryngol 23(2):85–90
Gupta N (2005) Endoscopic septoplasty. Ind J Otolaryngol Head Neck Surg 57:240–243
Gulati SP, Wadhera R, Ahuja N, Garg A, Ghai A (2009) Comparative evaluation of endoscopic with conventional septoplasty. Indian J Otolaryngol Head Neck Surg 61:27–29
Doomra S, Singh M, Singh B, Kaushal A (2019) Evaluating surgical outcomes of conventional versus endoscopic septoplasty using subjective and objective methods. Niger J Clin Pract 22:1372–1377
Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT (2004) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130(2):157–163
Singh A, Bhat N, Bhandarkar P, Singh R (2018) A comparative study of conventional versus endoscopic septoplasty. Bengal J Otolaryngol Head Neck Surg 26(1):1–9
Metzenbaum M (1929) Replacement of the lower end of the dislocated septal cartilage versus sub-mucus resection of the dislocated end of the septal cartilage. Arch otolaryngol 9(3):282–296
Galloway T. (1946) The nasal septum. In: Mackay I (ed), Scott-Brown’s Otolaryngology, 6th edn, Buttterworth-Heinemann International edition, p 4/11/1/27
Cottle M, Fisher G, Gaynor I, Loring R (1958) The maxilla-premaxilla approach to extensive nasal septum surgery. Arch Otolaryngol 68:301
Lanza DC, Rosin DF, Kennedy DW (1993) Endoscopic septal spur resection. Am J Rhinol 7(5):213–216
Stammberger H (1991) Functional endoscopic sinus surgery. The Messerklinger Technique, Decker BC., Philadelphia, pp 430–434
Bajwa F, Ilyas M, Iftilhar M, Aamer MI (2018) A comparative study of Endoscopic Septoplasty versus Conventional Septoplasty. Pak Postgrad Med J 29(2):70–74
Jain L, Jain M, Chauha AN (2011) Conventional septoplasty versus endoscopic septoplasty. Peoples J Sci Res 4(2):24–28
Rao JJ, Kumar ECV, Babu KR, Chowdary VS, Singh J, Rangamani SV (2005) Classification of nasal septal deviation relation to sinonasal pathology. Indian J Otolaryngol Head Neck Surg 57(3):199–201
Sathyaki DC, Geetha C, Munishwara GB, Mohan M, Manjuanth K (2014) A comparative study of endoscopic septoplasty versus conventional septoplasty. Indian J Otolaryngol Head Neck Surg 66(2):155–161
Suraneni VR, Kudamala S, Srikanth K (2018) Conventional vs endoscopic septoplasty: our experience. Int J Oper Res Head Surg 4:403–408
Mandal S, Jana S (2020) A comparative study of endoscopic and conventional septoplasty. Int J Med Res Rev 8(1):1–6
Giles WC, Gross CW, Abram AC, Greene WM, Avner TG (1994) Endoscopic septoplasty. Laryngoscope 104(12):1507–1509
Guindi SS, Mostafa HS, Fawzy TO (2016) Endoscopic-assisted septoplasty versus traditional septoplasty: assessment by the NOSE scale. Egypt J Otolaryngol 32:26–31
Paradis JRB (2011) Open versus endoscopic septoplasty: a single-blinded, Randomized, controlled trial. J Otolaryngol Head Neck Surg 40(1):28–33
Bothra R, Mathur NN (2009) Comparative evaluation of conventional versus endoscopic septoplasty for limited septal deviation and spur. J Laryngol Otol 123:737–741
Acknowledgements
None.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Heemani Bhardwaj and Aditiya Saraf made contribution in data collection and design of manuscript. Gopika Kalsotra made contribution in interpretation of data. Parmod Kalsotra and Padam Singh made contribution in data analysis. All authors read and gave approval to the final version of submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
the authors declare they have no competing interests.
Ethics Approval and Consent to Participate
The study was conducted after approval by Institutional Ethics Committee of GMC Jammu. Written informed consent was taken from all subjects or their legal guardian in case of age of patient being less than 18 years. No animals were used in the study.
Consent for Publication
Written informed consent to publish patient’s clinical details was obtained from all subjects or their legal guardian in case of subject under 18 years.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhardwaj, H., Kalsotra, G., Kalsotra, P. et al. Surgical Outcomes of Endoscopic Versus Conventional Septoplasty. Indian J Otolaryngol Head Neck Surg 75, 1724–1730 (2023). https://doi.org/10.1007/s12070-023-03720-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03720-6