Abstract
Papillary thyroid carcinoma (PTC) is the most common differentiated thyroid neoplasm. Common sites of regional and distant metastasis includes lymph nodes, lungs and bone. 51 year old female patient who was a known case of PTC with a history of multiple surgeries, radioactive iodine therapy (RAI) and oral chemotherapy presented with a painful right parotid mass. PET scan demonstrated FDG avid lesions in the right parotid gland, cervical lymph nodes and other distant sites. Cytology report showed features of metastatic PTC. Patient underwent extended total parotidectomy with facial nerve resection, skin and masseter muscle resection and extended radical neck dissection. Final histopathology (HPE) report showed metastatic papillary carcinoma thyroid. Patient is currently on oral chemotherapy and on regular follow up. PTC rarely metastasizes to parotid gland and such cases have to be treated with surgery alone or with a combination of surgery and RAI based on tumour burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Majority of metastasis to the parotid gland are from cutaneous tumours of the scalp, face, external ear, eyelids, or nose. Metastasis from primary sites below the head and neck region are uncommon and usually derived from carcinomas of the lung, breast, kidney, colon, and prostate [1].
The incidence of papillary thyroid carcinoma (PTC) from 1975 to 2012 increased from 4.8 to 13.3 per 100,000 [2]. PTC is the most frequent type of thyroid carcinoma encountered. Lymph node (LN) metastasis occurs in up to 80% of PTC cases [3]. Distant metastasis, however, is uncommon and occurs at a rate of 2% to 10% [2]. Metastasis of PTC to parotid gland is very rare [4]. Mathew et al. identified only five such cases in their case report [5].
Case Report
51 year old hypertensive and hypothyroid female patient, who was a follow up case of metastatic recurrent PTC presented to us with a swelling over the right parotid region. She had undergone total thyroidectomy in 1992, which was followed by four consecutive surgeries for removal of neck mass (no detailed data was available with the patient) in 2006, 2007, 2012 and 2015. She had received high dose radioactive iodine therapy (RAI) for a total dose of 600 millicurie. She had also received oral chemotherapy (sorafenib) from December 2017 to June 2018. Fibreoptic laryngoscopy (FOL) done in 2018 showed right vocal cord palsy. In February 2021 she had an episode of bleeding from the thyroid bed for which she received Hemostatic Radiotherapy (RT). From February 2021 to May 2021 she was on lenvatinib for multiple distant metastasis.
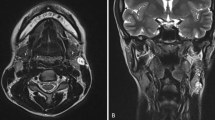
On clinical examination, she had a 6 × 8 cm mass over the right parotid region with ulceration of the overlying skin. Facial nerve function appears normal. Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) done in February 2022 showed FDG-avid lesion in right parotid measuring 6 × 4 cm along with a nodal mass involving levels Ia, Ib, parapharyngeal and supraclavicular nodes, right sided pleural effusion, diffuse pleural thickening and nodularity in the right hemithorax, multiple bilateral lung nodules, multiple mediastinal nodes and bone metastasis to bilateral iliac bone and femur (Fig. 1). Ultrasound (USG) guided fine needle aspiration cytology (FNAC) of the parotid mass showed features of metastatic PTC. Cytological examination of pleural fluid also indicated features of metastatic PTC. Pre operatively thyroglobulin level was detected to be > 5160. Although the patient had multiple distant metastasis, the decision to go ahead with surgery was taken in view of reducing the tumour load.
Maximum intensity projection (MIP) image (a), axial sections of CT and fused PET/CT (b–k) showing FDG avid lesion in right parotid measuring 6 × 4 cm along with nodal mass involving level Ia, Ib, parapharyngeal and supraclavicular nodes, right pleural effusion, diffuse pleural thickening and nodularity in right hemithorax, multiple bilateral lung nodules, multiple mediastinal nodes, bone metastasis to bilateral iliac bone and femur
The patient underwent extended total parotidectomy with removal of both the superficial and deep lobes of parotid gland along with the lower trunk of facial nerve. Extended radical neck dissection was done (level I-V, hypoglossal nerve sacrificed, external carotid artery ligated, sternocleidomastoid, internal jugular vein and spinal accessory nerve sacrificed, overlying skin removed). The post-operative defect (Fig. 2) was reconstructed using pectoralis major myocutaneous flap. The final specimen was sent for histopathological (HPE) examination.
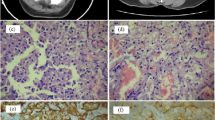
The final HPE report showed an irregular lesion measuring 9 × 6 × 4 cm almost replacing the entire parotid gland and morphology was consistent with metastatic PTC of tall cell variant, with lymphovascular invasion and perineural infiltration (Fig. 3a, b). All peripheral resected margins were free of tumour. 10/10 lymph nodes with metastatic papillary carcinoma having extracapsular extension was noted in the radical neck dissection specimen with the largest metastatic lymph node measuring 2.8 cm. Immunohistochemistry for thyroid transcription factor 1 (TTF1) and thyroglobulin (Tg) showed strong immunopositivity (Fig. 3c, d).
a Haematoxylin eosin stained ×40 shows a malignant papillary epithelial tumour with intranuclear grooves, morphologically suggestive of metastatic papillary carcinoma thyroid–tall cell variant. b Haematoxylin eosin stained ×200, shows high power tumour cell nuclei with nuclear clearing, nuclear overlapping with intranuclear inclusions. c ×100 tumour cells show diffuse strong nuclear positivity for TTF1. d ×40 tumour cells shows diffuse immunopositivity for thyroglobulin
FDG-PET scan done 2 months post operatively showed minimal diffuse FDG uptake in the right hemithorax. There was no RAI uptake noted in any of the other sites of distant metastasis which were present in PET scan probably because the tumour had undergone de differentiation. On 6 months follow up, patient was doing well and was on oral chemotherapy (lenvatinib) as advised by the specialists in medical oncology.
Discussion
PTC is the most common variant of well differentiated thyroid cancer (DTC) [6]. Distant metastasis occurs only in 4 to 8% of PTC. The most common sites for distant metastasis is lungs followed by bone and the less common sites include breast, adrenal, pituitary, kidney, orbit, brain, malar bone, and jaw bone [7]. Parotid as a site of distant metastasis is very rare for thyroid cancers. Occasionally, PTC with indolent behaviour has potential to transform into a poorly differentiated pattern, and the occurrence of parotid gland metastasis, in spite of its relative low occurrence, indicates that less differentiated tumours may spread to unusual regions [1].
Transformation to dedifferentiated form of papillary carcinoma occurs over time and is characterized by the following features—rapid growth, distant metastasis, tendency to recur and poor response to radioactive iodine therapy [8]. In the current case, this explains why the tumour did not show RAI uptake and was not responding to RAI therapy as it had already undergone dedifferentiation.
Tall cell variant has higher risk of locoregional and distant relapse with worse overall survival compared to the classical variant. Tall cell variant has shown to be an independent prognostic factor for disease-specific death [9]. Tall cell variant of PTC was detected in our case which is probably why the patient had multiple relapses and extensive locoregional and distant metastasis.
10-year disease-specific survival of classic PTC is 85–92% but with distant metastasis it reduces to 10–40% [10]. Poorly differentiated thyroid carcinoma has a 5-year overall survival of 65–85% [11].
Wu et al. found 3 cases (0.019%) of parotid metastasis in a review of 15,780 cases of thyroid carcinoma and in a systematic search of literature found that only 10 additional cases had been reported up to 2015. 8 of all 13 cases had papillary or follicular thyroid carcinoma with the remaining cases in patients with medullary thyroid carcinoma [12]. Less than 15 cases of parotid metastasis from thyroid cancer has been recorded in literature (Table 1) of which majority are from PTC.
Operable cases are best treated with surgery followed by RAI and add on chemotherapy or radiotherapy as required on a case to case basis. From the previous literature available, it is clearly demonstrated that majority of the patients with parotid metastasis were treated surgically and followed with RAI (Table 1).
Parotid gland metastasis in DTC is best treated with total thyroidectomy with central and/or bilateral lymph node dissection and parotid tumour resection [22].
This case report emphasizes on considering metastatic PTC as a differential diagnosis for parotid neoplasms. It is important to take careful history and proper clinical examination in such cases. Essential radiological imaging and FNAC are important tools in reaching the diagnosis [23].
Conclusion
Recurrent or metastatic papillary thyroid carcinoma should be considered as an important differential for parotid neoplasms of unknown primary. Metastasis to parotid gland from thyroid cancer, seems to be an indication of aggressive disease with high frequency of lung and bone metastasis with poor survival. In long standing cases, dedifferentiation is an important factor responsible for non-response to RAI. Reduction of tumour burden is the main treatment aim in such cases and the treatment modalities include surgery, RAI and chemotherapy based on multiple factors as discussed in the article.
Data Availability
Not applicable.
References
Kini H, Pai RR, Kalpana S (2003) Solitary parotid metastasis from columnar cell carcinoma of the thyroid: a diagnostic dilemma. Diagn Cytopathol 28:72–75
Cancer Stat Facts: Thyroid cancer. Accessed 20 Apr 2021. https://seer.cancer.gov/statfacts/html/thyro.html
Randolph GW, Duh QY, Heller KS et al (2012) For the American Thyroid Association Surgical Affairs Committee’s Taskforce on Thyroid Cancer Nodal Surgery RM; the prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid 22(11):1144–1152. https://doi.org/10.1089/thy.2012.0043
Kilic K, Sakat MS, Gozeler MS, Demirci E (2017) Parotid gland involvement as an initial presentation of papillary thyroid carcinoma. Int J Oral Maxillofac Surg 46(8):965–967. https://doi.org/10.1016/j.ijom.2017.04.002
Mathew PC, Balagopal PG, Thomas S, Sebastian P, Preethi TR (2007) Parotid metastasis from carcinoma of the thyroid. Int J Oral Maxillofac Surg 36:965–966
Shi X, Liu R, Basolo F, Giannini R, Shen X et al (2016) Differential clinicopathological risk and prognosis of major papillary thyroid cancer variants. J Clin Endocrinol Metab 101(1):264–274
Slim I, Mhiri A, Meddeb I, Goucha A, Gritli S, Ben Slimene MF (2012) Malar bone metastasis revealing a papillary thyroid carcinoma. Case Rep Otolaryngol 2012:795686
Chen H, Luo D, Zhang L, Lin X, Luo Q, Yi H, Wang J, Yan X, Li B, Chen Y, Liu X, Zhang H, Liu S, Qiu M, Yang D, Jiang N (2017) Restoration of p53 using the novel MDM2-p53 antagonist APG115 suppresses dedifferentiated papillary thyroid cancer cells. Oncotarget 8(26):43008–43022
Pagano L, Caputo M, Sama MT, Zavattaro M, Prodam F, Mauri MG, Pia F, Alonzo A, Valente G, Aimaretti G (2013) Unusual metastases from tall cell variant of papillary thyroid cancer. Head Neck 35:E381–E385
Papp S, Asa SL (2015) When thyroid carcinoma goes bad: a morphological and molecular analysis. Head Neck Pathol 9(1):16–23
Ibrahimpasic T, Ghossein R, Carlson DL, Nixon I, Palmer FL, Shaha AR, Patel SG, Tuttle RM, Shah JP, Ganly I (2014) Outcomes in patients with poorly differentiated thyroid carcinoma. J Clin Endocrinol Metab 99(4):1245–1252
Wu ZH, Ge MH, Cao J, Lan XB, Zhu XH, Huang YQ, Yu B (2017) Parotid metastases from thyroid carcinomas. Int J Clin Exp Pathol 10(10):10467–10474
Markitziu A, Fisher D, Marmary Y (1986) Thyroid papillary carcinoma presenting as jaw and parotid gland metastases. Int J Oral Maxillofac Surg 15(5):648–653. https://doi.org/10.1016/S0300-9785(86)80074-6
Malhotra G, Nair N, Awasare S, Baghel NS (2007) Metastatic parotid tumor: a rare presentation for papillary carcinoma of thyroid. Clin Nucl Med 32(6):488–490. https://doi.org/10.1097/RLU.0b013e31805379ce
Hafez MT, Refky B, AbdElwahab K, Arafa M, Abdou I, Elnahas W (2015) Axillary lymph nodes metastasis in a patient with recurrent papillary thyroid cancer: a case report. J Med Case Rep 9(1):1–3. https://doi.org/10.1186/s13256-015-0668-7
Farahmandfar F, Shakeri S, Askari E et al (2020) Parotid metastasis as the first presentation of papillary thyroid carcinoma. Iran J Nucl Med 28(2):42–45
Alzaraa A, Stone J, Williams G, Ahmed I, Quraishi M (2008) Direct spread of thyroid follicular carcinoma to the parotid gland and the internal jugular vein: a case report. J Med Case Rep 2:297
Pelosi S, Genden EM (2009) Medullary thyroid carcinoma metastatic to the parotid gland. Laryngoscope 119:253
Conway A, Wiernik A, Rawal A, Lam C, Mesa H (2012) Occult primary medullary thyroid carcinoma presenting with pituitary and parotid metastases: case report and review of the literature. Endocr pathol 23:115–122
Zikos P, Vafiadou M, Kechagias N, Vahtsevanos K, Mangoudi D (2013) Metastases to the parotid gland from a medullary thyroid carcinoma (case report). Oral Oncol 49:143
Garca-Arns JA, Maldonado C, Fernndez R, Gonzalo M (2014) Thyroid papillary microcarcinoma presenting as parotid metastasis: a case report. Endocr Abstr 35:331
Wexler JA (2011) Approach to the thyroid cancer patient with bone metastases. J Clin Endocrinol Metab 96:2296–2307
Liu CC, Jethwa AR, Khariwala SS, Johnson J, Shin JJ (2016) Sensitivity, specificity, and post test probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 154(1):9–23. https://doi.org/10.1177/0194599815607841
Acknowledgements
I would like to acknowledge the efforts of the department of robotics and surgical oncology, department of radiology and pathology of BLK-MAX Superspeciality hospital.
Funding
No source of funding for the study.
Author information
Authors and Affiliations
Contributions
Study Concepts: Surendra K Dabas, Nandini N Menon, Himanshu Shukla, Reetesh Ranjan; Study Design: Nandini N Menon, Sahibinder Singh Bhatti, Saurabh Arora; Data Acquisition: Nandini N Menon, Sahibinder Singh Bhatti, Saurabh Arora; Quality control of data: Nandini N Menon, Himanshu Shukla, Reetesh Ranjan; Manuscript preparation: All Authors; Manuscript editing: All Authors; Manuscript reviewing: All Authors.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest amongst the authors of the study.
Ethical Approval
The study is conducted abiding the ethical standards of the institution.
Informed Consent
A written and informed consent was taken for the procedure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dabas, S.K., Menon, N.N., Shukla, H. et al. Parotid Metastasis in a Case of Papillary Thyroid Carcinoma: Case Report and Review of Literature. Indian J Otolaryngol Head Neck Surg 75, 1123–1128 (2023). https://doi.org/10.1007/s12070-022-03425-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03425-2