Abstract
Tracheo-oesophageal fistula (TOF) is defined as a pathological connection between the trachea and the oesophagus, leading to a spillover of oral and gastric secretions into the respiratory tract causing aspiration. The cause of TOF may be congenital or acquired. In this case report, a 48 years old female with acquired TOF, has been reported. The patient was on ventilator support for COVID-associated pneumonia and its complication with endotracheal tube for 3 weeks and then tracheostomy was done. Post recovery after weaning from the ventilator, the patient was diagnosed with TOF by bronchoscopy and confirmed by CT and MRI. Surgical closure was performed: the oesophageal defect was sutured in 2 layers and Tracheal wall was isolated and a pedicled strap muscle flap sutured into the defect between the trachea and esophagus. The etiology of TOF may be due to traumatic intubation, cuff pressure, or inflammation. A better knowledge about the cause, site, and size of the TOF will help in prompt surgical procedure and recovery of the patient. This single staged surgical closure can be safely performed in the majority of patients with acquired TOF for optimal outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tracheo-oesophageal fistula (TOF) is defined as a pathological connection between the trachea and the oesophagus, leading to a spillover of oral and gastric secretions into the respiratory tract [1]. TOF is classified into two main categories: congenital and acquired. Acquired TOF mainly affects the adult population and is further divided into malignant and benign categories. In this case report, we are presenting an acquired benign TOF, in which we used an innovative single staged surgical procedure.
Case Report
A 48-year-old woman suffering from covid 19 pneumonia was admitted to a private hospital and treated conservatively with injection remdesivir and anticoagulants. As her hypoxia worsened, she was intubated and prone ventilated. She had also developed a cavity and consolidation in both lower lobes of the lungs. Ultrasound chest revealed loculated pleural effusion on the left side. She developed septic shock and had to remain in ICU for further treatment. A surgical tracheostomy was done 3 weeks later. However, her sensorium deteriorated and CT brain was found to show acute toxic leukoencephalopathy and EEG showed signs of diffuse cerebral dysfunction. The patient also developed acute kidney injury and was put on hemodialysis. The patient’s GCS continued to be low despite oxygen saturation, hemodynamics, and kidney functions recovering. After 3 weeks when GCS showed an improvement, oral feeding trials were done but the patient had repeated aspiration and vomiting. On bronchoscopy, a large trachea esophageal fistula was seen just above the tracheostomy cuff. Percutaneous endoscopic gastrostomy (PEG) feeding was started and the patient was discharged and referred to our ENT center.
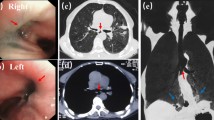
For further evaluation CT (Fig. 1) and MRI ((Fig. 2) neck were taken and it showed a large defect 1.5 * 1.5 cm in the left paramedian aspect of the trachea at the C7 & T1 level. A corresponding defect in the anterolateral wall of the esophagus was seen.
The patient was admitted to our center and planned for the transcervical repair of the TOF. After explaining the procedure an informed and written consent was obtained, the surgical procedure was planned under general anesthesia (GA).
Under GA, the patient was induced and an incision was made at the site of tracheostomy. The subplatysmal flap was elevated, strap muscles were identified and separated. Laryngotracheal framework isolated. Left side recurrent laryngeal nerve isolated carefully up to cricothyroid joint (Fig. 3). Then, the esophageal wall adjacent to the defect was marked with vicryl sutures with the aid of an endoscope (scope passed through stoma).
Dissection was taken gently into the tracheoesophageal groove and the tracheal defect isolated. Then, the fistula wall was excised, esophageal mucosa was repaired in two layers with continuous absorbable sutures (Fig. 4). The tracheal wall was isolated and a pedicled strap muscle flap sutured into the defect between the trachea and esophagus.
The postoperative period was uneventful and the patient was maintained on PEG feeds. Oral feeding was started on postoperative (POD) day 11 and decannulation was done on the next day on POD 12 (Fig. 5).
After ensuring adequate airway and vocal cord movement, PEG was also removed. The patient is on follow-up till date and doing well.
Discussion
Acquired TOF mainly affects the adult population is divided into malignant and benign categories [2]. The most common cancer associated with malignant TOF is oesophageal cancer, with > 10% of patients developing the condition during its clinical course [3].
Benign TOF occurs in the setting of prolonged mechanical ventilation via an endotracheal tube or tracheostomy tube, excessive cuff pressure of endotracheal tube or tracheostomy tube, blunt trauma to the chest or the neck, traumatic airway injury, granulomatous mediastinal infections [4]. Other aetiologies of TOF in the setting of mechanical ventilation are traumatic intubation and airway suctioning. Comorbidities such as diabetes, prior airway infections, use of steroids, and the presence of nasogastric tubes also increase the risk of TOF formation associated with endotracheal and tracheostomy tubes [5]. Cervicothoracic junction is the most common site of acquired TEF [1].
Acquired TEF should be suspected in ventilated patients in the presence of persistent air leak despite a hyperinflated cuff, abdominal bloating, contamination of the tracheobronchial tree with food particles, and digestive secretions, such as gastric juice and bile, recurrent chest infection, and repeated failures to wean. In patients breathing spontaneously, clinical symptoms and signs are the ONO sign (persistent cough that follows the act of deglutition in the absence of another swallowing disorder), repeated lower respiratory tract infection and lung infection, cough with expectoration of food particles. The onset of symptoms in benign cases is more variable, ranging from 5 to 15 days for traumatic causes to 21–30 days for iatrogenic cuff-related injuries [6].
The diagnosis of TOF is made by a combination of thoracic imaging studies and endoscopy (both flexible bronchoscopy and upper endoscopy if possible). An initial investigation of respiratory symptoms with a chest radiograph is reasonable. In addition to aspiration-related changes, the etiology of TOF may be apparent on initial radiographic evaluation such as a lung mass, the overinflated cuff of endotracheal/tracheostomy tube, widened mediastinum from granulomatous disease, or a pre-existing oesophageal stent. Although there are no formal guidelines, most experts agree that oesophagography and endoscopy are necessary to diagnose the disease and to perform pre-operative planning. Oesophagography is performed preferentially with barium. The contrast-enhanced oesophagogram demonstrates the defect in ~70% of patients with TOF [7]. Computed tomography (CT) scan of the chest can be performed to evaluate for signs of fistula, aerodigestive tract anatomy and mediastinal pathology. There are no available data assessing the sensitivity, specificity, negative or positive predictive value of CT scans in settings of known TOF. Once the thoracic imaging confirms the presence of TOF, the next step in evaluation is to assess the anatomy further via endoscopy and bronchoscopy. Endoscopic visualization allows for better localization, measurement, and characterization of the TOF [1].
After diagnosing the treatment options vary depending on the etiology. There are two clinical circumstances in which stents can be utilized: bridging benign TOF to definitive surgical therapy and palliating malignant TOF. In general, benign TOF is more amenable to definitive surgical intervention due to the transient nature of the injury and better nutritional status.
Alternative treatment modalities are fibrin glue injections, atrial closure devices and micromatrices. Fibrin glue injections have been used to treat small fistulae (< 5 mm). There are a few reports of bronchoscopic suturing techniques through tracheostomy sites [8], rigid bronchoscopy by using extracorporeal suturing techniques with a knot pusher or a Cor-Knot device [9]. In the report by Mozer et al. [10], the TOF of benign etiology was closed by suturing the fistula via a rigid oesophageal tube and securing it with a Cor-Knot device. They observed a full post-procedural closure of the fistula on the oesophagogram, and the patient was able to resume full oral intake at a 6-month follow-up.
A double patch technique, in which the esophageal wall was used as a protective patch repairing the defect on the trachea. Patient’s own viable esophageal tissue to repair the TEF rather than applying tracheal resection, to reduce the incidence of airway dehiscence after the repair in large TEFs. Thoracotomy is reserved for TEFs close to the carina.
The traditional approach uses a 2-layer longitudinal suture of the esophagus and segmental tracheal resection with end-to-end anastomosis for the trachea, as described by Grillo et al. [11] in 1976. This approach has been reported by other authors with small modifications [12]. As the general conditions and individual circumstances of these patients are often poor, an effective repair technique is critical.
In our approach, a simple and precise technique is followed to prevent complications and failure of closure.
Conclusion
The first step in diagnosing the TOF is understanding the pathophysiology of fistula formation between the airways and the oesophagus, and the associated conditions. The choice between definitive surgery, palliative stenting, use of a conservative approach will depend on the combination of patient’s condition and the underlying etiology of TOF. The single-stage repair offers patients the best chance of survival than multiple-staged surgical interventions. An innovative, individualized approach is frequently necessary for optimal outcomes.
References
Kim HS, Khemasuwan D, Diaz-Mendoza J et al (2020) Management of tracheo-oesophageal fistula in adults. Eur Respir Rev 29:200094. https://doi.org/10.1183/16000617.0094-2020]
Reed MF, Douglas JM (2003) Tracheoesophageal fistula. Chest Surg Clin N Am 13:271–289
Davydov M, Stilidi I, Bokhyan V et al (2001) Surgical treatment of esophageal carcinoma complicated by fistulas. Eur J Cardiothorac Surg 20:405–408
Santosham R (2018) Management of acquired benign tracheoesophageal fistulae. Thorac Surg Clin 28:385–392
Macchiarini P, Verhoye JP, Chapelier A et al (2000) Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fistulas. J Thorac Cardiovasc Surg 119:268–276
Diddee R, Shaw IH (2006) Acquired tracheo-oesophageal fistula in adults. Contin Educ Anaesth Crit Care Pain 6:105–108
Couraud L, Ballester MJ, Delaisement C (1996) Acquired tracheoesophageal fistula and its management. Semin ThoracCardiovasc Surg 8:392–399
Caronia FP, Reginelli A, Santini M et al (2017) Trans-tracheostomy repair of tracheoesophageal fistula under endoscopic view in a 75-year-old woman. J Thorac Dis 9:E176–E179
Galluccio G (2016) Endoscopic treatment of tracheo-oesophageal fistulae: an innovative procedure. Multimed Man Cardiothorac Surg 201:mmw015
Mozer AB, Michel E, Gillespie C et al (2019) Bronchoendoscopic repair of tracheoesophageal fistula. Am J Respir Crit Care Med 200:774–775
Grillo HC, Moncure AC, McEnany MT (1976) Repair of inflammatory tracheoesophageal fistula. Ann Thorac Surg 22:112–119
Marulli G, Loizzi M, Cardillo G et al (2013) Early and late outcome after surgical treatment of acquired nonmalignant tracheo-oesophageal fistulae. Eur J Cardiothorac Surg 43:e155–e161
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Committee Approval
Obtained.
Informed and Written Consent
Taken.
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Velusamy, A., Anand, A., Janarthanan, S. et al. An Innovative Single Staged Surgical Repair of Benign Tracheoesophageal Fistula – A Case Report. Indian J Otolaryngol Head Neck Surg 75, 2585–2590 (2023). https://doi.org/10.1007/s12070-022-03382-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03382-w