Abstract
Introduction
Identifying surgical candidacy for the management of laryngomalacia is a challenge.
Objective
To develop a simple scoring system for surgical candidacy in laryngomalacia.
Methods
Eighteen years retrospective observational study of children with laryngomalacia (LM) clinically categorized into mild, moderate and severe LM and were analyzed for surgical candidacy.
Results
There were 113 children (age ranging from 5 days to 14 months), 44% being mild, 30% moderate and 26% severe LM. None in mild, 32% in moderate, and all in severe LM had surgical intervention. Presence of stridor on feeding or crying and isolated type 1 or type 2 LM on laryngoscopy were significant indicators for conservative treatment (p-< 0.0001). Moderate failure to thrive, retraction at rest/sleep, with low oxygen saturation while feeding/at rest were significantly higher in both moderate and severe groups with laryngoscopic evidence of combined type 1 and 2 in moderate LM (p < 00,001). Aspiration pneumonia, hospitalization, pectus and mean pulmonary arterial pressure of more than 25 mmHg with laryngoscopic findings of all three combined types were significantly higher in severe LM (p < 0.0001).
A simple scoring system was then developed and it revealed that a score of 10 or more required surgical intervention.
Conclusion and clinical significance
A clinical scoring system is being reported for the first time in medical literature to identify ‘the difficult to treat’ subset within moderate laryngomalacia category simplifying decision making in its management for otolaryngologists and pediatricians as well as a referral criterion for pediatric otolaryngologists’ services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Laryngomalacia (LM), the most common laryngeal disease of infancy, is described as “inward collapse of supraglottic structures into glottic airway during the inspiratory phase of respiration” causing inspiratory stridor with an occurrence of 60–75% in all congenital laryngeal malformations [1]. Though, stridor is the most common symptom of laryngomalacia, other additional features associated with laryngomalacia like retractions (suprasternal/ substernal/ intercostal), feeding difficulties, regurgitation, choking, gastroesophageal reflux, cyanosis, failure to thrive, apnea and pulmonary hypertension have been described [2,3,4,5].
Clinical diagnosis of laryngomalacia is confirmed by flexible laryngoscopy. The most commonly followed classification for the anatomic variations of supraglottic structural collapse in LM was described by Olney et al. as type 1; prolapse of mucosa overlying the arytenoid cartilages; type 2, foreshortened aryepiglottic folds; and type 3, posterior displacement of the epiglottis [6].
The disease spectrum of LM ranges from mild to severe, based on associated feeding and obstructive symptoms. Though majority of infants with LM have mild disease with spontaneous recovery, approximately 20% will have failure to thrive, gastroesophageal reflux disease, aspiration pneumonia, hypoxemia, OSA, pulmonary hypertension or cor-pulmonale and surgery being required for the such cases [2, 7, 8].
Published data revealed that moderate LM is a therapeutic challenge for conservative or surgical intervention [2, 9, 10]. A landmark ‘laryngomalacia consensus recommendations’ was published by International Pediatric ORL Group (IPOG) regarding evaluation and treatment considerations, initial presentation and comprehensive care algorithm with symptomatic classification criteria and associated at risk co-morbidities [11].
In this article [11], laryngomalacia has been categorized as:
-
a.
Mild when only stridor with no symptoms or no radiographic evidence of simultaneous airway lesions (SAL).
-
b.
Moderate when associated cough, choking, regurgitation or feeding difficulty.
-
c.
Severe: evidence of apnea, cyanosis, failure to thrive, pulmonary hypertension and cor pulmonale.
As per their consensus statement, cases of moderate LM, also called “difficult to feed infant”, should be advised close follow up with specific medical protocol for decision making regarding conservative versus surgical treatment. One should bear in mind that aspiration, pooling of secretions, and decreased supraglottic sensation may be seen during endoscopy in uncontrolled laryngopharyngeal reflux and neurologic disease as well [11].
Our study was conducted in a tertiary care multi-specialty hospital with experience in upper airway disorders and LM since 2001. The objective was to develop a scoring system based on the clinical profile staging and management of infants/children diagnosed to have laryngomalacia for practicing otolaryngologist in decision-making in surgical management or referral for the same to specialist pediatric ENT care.
Methods
This retrospective observational study was approved by our Institutional Review Board and Ethical Committee (ECR/34/inst/KA/2013/RR-19). A retrospective chart review was performed and complete medical records including clinical profile, staging and management of infants and children who were diagnosed with laryngomalacia following flexible fiberoptic laryngoscopic examination in the department of Otolaryngology in our hospital between January 2001 to December 2019 was done. These patients were categorized into mild, moderate and severe based on their clinical presentation and treated conservatively or surgically with the then available recommendations [6, 7, 9]. Children with acquired laryngomalacia, that associated with congenital cardiac anomaly, neurological disorders or synchronous lesions of larynx were excluded from the study. The following parameters were reviewed:
-
Demographic data: patient’s age at presentation and gender.
-
Clinical presentation: presence of stridor, feeding difficulties, history of previous hospitalization due to aspiration pneumonia, presence of retractions, pectus excavatum and failure to thrive.
-
Investigation findings: In addition to complete blood count, blood sugars, serum creatinine, the following investigations findings were recorded and documented –
-
Pulse oximetry for saturation during awake / feeding / sleeping,
-
Transthoracic echocardiography for assessment of presence and severity of pulmonary hypertension (PH) from Tricuspid Regurgitant jet,
-
Flexible laryngoscopy findings to know the types of collapse as described by Olney et al. [6], recorded and documented.
-
-
Management approach followed either conservative or surgical.
-
Follow up period.
During this evaluation, short audio-visual clip of children had been recorded to document the stridor quality and chest retractions when possible. Clinical presentation was tabulated and analyzed for their significance in management protocol.
On the basis of clinical parameters, a simple scoring system was then developed. The scores were divided into 7 subsets, which includes inspiratory stridor, chest retractions, feeding difficulties with pulmonary infections, failure to thrive, oxygen desaturation, laryngoscopic findings and mean pulmonary arterial pressure on echocardiogram. Each subset was further scored from 0/1 to 3 according to the symptoms and signs. The scoring system was consolidated between the score of 1–21. (Appendix 1A).
Statistical Analysis
Data was expressed as percentage. Fischer’s exact test or Chi square test was used to analyze the significance of difference between frequency distribution of the data. P value < 0.05 was considered as statistically significant. SPSS© for windows™ Vs 17, IBM™ Corp NY and Microsoft excel™ 2016, Microsoft® Inc USA was used to perform the statistical analysis.
Results
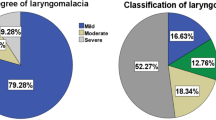
Total number of patients included in this study were 113. The summary of the clinical findings in these patients has been shown separately (Table 1). There were 50 (44%) infants in mild, 34 (30%) in moderate and 29 (26%) in severe clinical grading of LM. The age of presentation ranged from five days to 14 months. All (100%) infants in mild group (50) and in severe group (29) had conservative and surgical treatment respectively. In the moderate group, 68% (23/34) had conservative treatment and 32% (11/34) had surgical intervention. Thus 64.6% (73/113) cases in this study were treated conservatively with close monitoring, where usual symptoms disappeared at the average age of 8 months (range- 4–10 months). Remaining 35.4% (40/113) underwent suspension laryngoscopy with telescopic examination without muscle relaxant and supraglottoplasty was performed under general anesthesia. Average age at the time of surgical intervention was 3.5 months with a range of 17 days to 14 months. All children (whether conservative / surgical) were rigorously followed up till recovery and were eventually noted to have normal respiration and normal growth rate with respect to weight gain. Overall, the follow up period for all the cases was average of 7.3 months (range 3–12 months).
Isolated type 1 or 2 laryngoscopic findings (Olney’s classification) was noted in 43/113 (38%) patients, all of them having conservative treatment, which was statistically significant(p < 0.0001). Similarly, combined all three types found in 11.5% (13/113) and all had surgical intervention which was also statistically significant ((p < 0.0001). None of the cases had isolated type 3 or type 1 & 3 in our series.
The comparison of various parameters between subjects with different treatment has been tabulated separately (Table 2). Stridor at rest and feeding difficulty was found to be significantly less in mild LM (p < 0.0001) and indicators for conservative treatment being stridor only on feeding or crying and/or isolated type 1 or type 2 LM on laryngoscopy (p-< 0.0001).
Moderate failure to thrive, retraction while awake (at rest) and while in sleep as well as low oxygenation saturation while feeding and awake (at rest) was significantly higher in both moderate and severe LM, though laryngoscopy showed significantly more of combined type 1 and 2 in moderate LM (p < 00,001). Signs of aspiration pneumonia, hospitalization, pectus, mean pulmonary arterial (Pa) pressure of more than 25 mmHg on echocardiogram and laryngoscopic findings of all three combined were found to be significantly higher in severe LM (p < 0.0001). Odd’s ratio for pulmonary infections was significantly higher in severe LM when compared to moderate LM (75.2 versus 10.96) (Table 2).
The novel scoring system (Appendix 1A) was then implemented on all the 113 patients and analyzed with the treatment given. 76/113 had scores less than 10 ranging from 2 to 9. Among them, 94.7% (72/76) patients were treated conservatively. The four who had surgical intervention, none were clinically mild, three patients had score 9 one being clinically moderate, two were clinically severe) and one patient though had score 8 was clinically severe. 37/113 patients were having score 10 or more ranging from 10 to 16. All these patients were treated surgically except one, with score 10 who was clinically moderate and was followed up for 11 months.
Discussion
Laryngomalacia is traditionally considered as mild and self-limiting disease in majority of cases. However, LM can also be moderate or severe with significant disease in a group of patients, leading to life threatening complications without surgical intervention [2, 4, 5, 7,8,9, 11]. A case control study of 51 newly diagnosed moderate to severe congenital LM was done and the authors concluded that appropriately selected infants with moderate to severe LM can be managed with medical management and close observation [10]. Landry and Thompson had reported that about 40% of LM who present to the primary care physician may be mild and another 40% be moderate clinically [2]. Around 70% in each clinical group would resolve requiring conservative treatment only. Those with mild disease and baseline resting SAO2 of ≤ 96% are predicted to progress to the moderate disease category and an average resting SAO2 of ≤ 91% is also more likely to progress to severe disease requiring surgical intervention [12]. In our study of 113 infants with LM, 44% mild, 30% moderate and 26% had severe laryngomalacia.
Majority of moderate LM (68%) in our study had conservative treatment in spite of moderate failure to thrive, while about one third had surgical management. Our series also suggested that the severity of disease also manifests in myriad ways like presence of stridor while sleeping, development of pectus excavatum, feeding difficulties causing failure to thrive, recurrent aspiration pneumonia and raised pulmonary arterial pressure, similar in the previous published studies [13,14,15,16].
Similar to our study, it has been suggested by various authors that a subset of those in the moderate LM would require surgical intervention [2, 8,9,10,11]. The clinical challenge was to identify surgical candidates in moderate LM. Shah et al. suggested a severity score based on symptoms and concluded that cut off score 4 to decide for surgery but this paper has only taken clinical symptoms in to consideration [17]. Our scoring system derived from the clinical features and investigations into account to identify surgical candidacy. According to this, it is noted that a score more than 10 with moderate LM, was treated surgically. The algorithm for management of laryngomalacia has been suggested in Appendix 1B. This is being reported for the first time.
Limitations
Our study was a retrospective study. On the basis of previous operated cases, this scoring system has been proposed and the validation of this scoring system is needed on a multicentric prospective study approach. Prematurity and the birth weight were not included in analysis as the data was not available for all the patients. We excluded patients with other comorbidities. Though the gold standard of measuring pulmonary hypertension is right heart catheterization, due to the risks of invasive procedure and the very young age of our patients it was measured via transthoracic echocardiography.
Conclusion and Clinical Significance
Clinical staging of laryngomalacia (LM) still remains the cornerstone for therapeutic decision, indicating conservative medical management in mild LM and surgical management in severe LM as suggested by the ‘Laryngomalacia Consensus Recommendations’. Our novel scoring system when applied, a score of 10 or more identifies the one third of moderate laryngomalacia who require surgical intervention thus simplifying surgical candidacy for the attending pediatrician, otolaryngologist as well as pediatric otolaryngologists in management of laryngomalacia. This is a proposed clinical scoring system which needs to be validated with a multicentric prospective study.
References
Holinger LD (1980) Etiology of stridor in the neonate, infant and child. Ann Otol Rhinol Laryngol 89:397–400
Landry AM, Thompson DM (2012) Laryngomalacia: disease presentation, spectrum, and management. Int J Pediatr [Internet]. [cited 2020 Sep 17]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles
Hartl TT, Chadha NK (2012) A systematic review of laryngomalacia and acid reflux. Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 147:619–626
Thompson DM (2010) Laryngomalacia: factors that influence disease severity and outcomes of management. Curr Opin Otolaryngol Head Neck Surg 18:564–570
Unal E, Oran B, Baysal T, Baspinar O, Keser M, Karaarslan S et al (2006) Pulmonary arterial pressure in infants with laryngomalacia. Int J Pediatr Otorhinolaryngol 70:2067–2071
Olney DR, Greinwald JH, Smith RJ, Bauman NM (1999) Laryngomalacia and its treatment. Laryngoscope 109:1770–1775
Roger G, Denoyelle F, Triglia JM, Garabedian EN (1995) Severe laryngomalacia: surgical indications and results in 115 patients. Laryngoscope 105:1111–1117
Thorne MC, Garetz SL (2016) Laryngomalacia: review and summary of current clinical practice in 2015. Paediatr Respir Rev 17:3–8
Thompson DM (2007) Abnormal sensorimotor integrative function of the larynx in congenital laryngomalacia: a new theory of etiology. Laryngoscope 117:1–33
Faria J, Behar P (2014) Medical and surgical management of congenital laryngomalacia: a case-control study. Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 151:845–851
Carter J, Rahbar R, Brigger M, Chan K, Cheng A, Daniel SJ et al (2016) International Pediatric ORL Group (IPOG) laryngomalacia consensus recommendations. Int J Pediatr Otorhinolaryngol 86:256–261
Fearon B, Ellis D (1971) The management of long term airway problems in infants and children. Ann Otol Rhinol Laryngol 80:669–677
Richter GT, Wootten CT, Rutter MJ, Thompson DM (2009) Impact of supraglottoplasty on aspiration in severe laryngomalacia. Ann Otol Rhinol Laryngol 118:259–266
Ayari S, Aubertin G, Girschig H, Van Den Abbeele T, Mondain M (2012) Pathophysiology and diagnostic approach to laryngomalacia in infants. Eur Ann Otorhinolaryngol Head Neck Dis 129:257–263
Toynton SC, Saunders MW, Bailey CM (2001) Aryepiglottoplasty for laryngomalacia: 100 consecutive cases. J Laryngol Otol 115:35–38
Richter GT, Thompson DM (2008) The surgical management of laryngomalacia. Otolaryngol Clin North Am 41:837–864
Shah VS, Haupert M, Haddad G, Barazi R (2019) Laryngomalacia: the importance of disease severity. J Otolaryng Head Neck Surg 5:028
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study Concept & Design: Dr EVR, Dr DS, Dr MK, Dr GR. Analysis & Interpretation of Data: Dr DA, Dr DS, Dr EVR. Drafting of the Manuscript: Dr DS, Dr MK, Dr EVR, Dr DA. Critical revision of manuscript for important intellectual content: Dr MK, Dr EVR, Dr DA, Dr GR. Literature Research & analysis: Dr DS, Dr MK. Statistical Analysis: Dr DA, Dr DS. Study Supervision: Dr EVR, Dr MK, Dr GR.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare the following: Payment info: we declare that we have not received any financial support from any organization for this work submission. Financial relationships: we declare that we do not have any financial relationships with any organization who is interested in this work. Other relationships: we declare that there are no other relationships that could influenced the work we have published.
Human Subjects
Ethical committee approval for consent waiver was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1A
Raman's Scoring System for Surgical Candidacy of Laryngomalacia

Appendix 1B
Approach Algorythm for Mnagement of Laryngomalacia by Using Scoring System

Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shivnani, D., Raman, E.V., Kurien, M. et al. Surgical Candidacy for Management of Laryngomalacia: A Proposed Scoring System. Indian J Otolaryngol Head Neck Surg 75, 151–158 (2023). https://doi.org/10.1007/s12070-022-03307-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03307-7