Abstract
COVID 19 infections may be associated with a wide range of bacterial and fungal co-infections. Mucormycosis is a fungal infection primarily affecting immunocompromised individuals. We have observed sudden rise of mucormycosis cases in post COVID 19 patients. Here we have reported 100 cases of mucormycosis associated with COVID 19. To study epidemiology and clinical features of rhino orbital mucormycosis in post COVID 19 patients. To evaluate efficacy of medical as well as surgical treatment in such patients. This was an observational mixed (retrospective + prospective) study with a duration of 2 months. After noting demographic data, necessary radiological investigation was advised and representative tissue was sent for KOH and histopathological examination. Medical and surgical treatment was planned accordingly. Most patients (55%) presented with complaint of headache and facial pain. Hard palate involvement was observed in 45% patients. Unilateral presentation (68%) was more common. Only 25% patients who presented early had normal vision. We reported 22 patients with complete loss of vision. Eye movements were restricted in 58% patients. Diabetes mellitus is most common predisposing factor (65%). 9 patients required orbital exentration. Only 18% patients required Amphotericin for more than 14 days. Immune dysregulation caused by COVID 19 infection in addition to widespread use of steroids and broad-spectrum antibiotics may lead to the development mucormycosis. Diabetes Mellitus type II is another important risk factor and the presence of both have additional effect in causing mucormycosis. Headache and facial pain should be considered highly suspicious of mucormycosis. Early diagnosis with efficient treatment can improve prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 2019 novel coronavirus (2019-nCoV) or Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) first reported in Wuhan, Hubei province in China, quickly spread to other parts of the world forming a global pandemic [1]. It has shown a wide range of disease patterns, ranging from mild rhinitis to life-threatening pneumonia. A complex interplay of factors including pre-existing diseases, use of immunosuppressive therapy and systemic immune alterations of COVID-19 infection may lead to secondary infections. India has a high prevalence rate of Diabetes Mellitus type II (8.9% of adults, 77 million patients), which is a well-known risk factor [2]. Mucormycosis or Zygomycosis also called Phycomycosis is an aggressive, rapidly progressive and life-threatening fungal infection. A hallmark of mucormycosis infection is the presence of extensive angioinvasion with resultant vessel thrombosis and tissue necrosis [3]. Imaging techniques are not typically diagnostic. Even their cultures are not reliable. Only histological examination obtains a definitive diagnosis. Depending on the site of infection and underlying predisposing factors, mortality rates may vary from 10 to 100%. Early diagnosis and immediate intervention are crucial for such patients. Treatment includes control of the underlying disease, surgical debridement and systemic antifungal therapy. We have observed the sudden rise of mucormycosis cases in COVID-19 era. Very few articles are published on this subject. Being an apex institute of Gujarat, we are publishing this article with the aim of helping others in this field. Here we have reported 100 cases of mucormycosis in post Covid-19 patients.
Methods
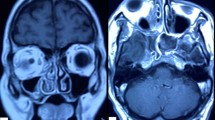
This was an observational mixed (retrospective + prospective) study of 100 patients with duration of 2 months. All the patients with rhino orbital mucormycosis admitted under ENT department of civil hospital, Ahmedabad during month of March and April 2021 were included in the study. Demographic data such as age, sex etc. were noted. Patients’ chief complaints were noted and thorough clinical examination was done. Sample collected from diseased tissue was sent for KOH and histopathological examination. Patients were advised necessary radiological investigation to know the anatomical variation and extent of the disease. Amphotericin B was started as soon as presence of mucormycosis was confirmed. Surgical debridement was planned after general anaesthesia check-up. Patients were evaluated post operatively by weekly nasal endoscopy with repeat biopsy. Once biopsy came negative for mucormycosis, patients were stepped down with syrup Posaconazole given with IV Amphotericin B. After 4 days, Amphotericin B was stopped and syrup Posaconazole was continued for 7 more days. All patients were kept on continuous surveillance by nasal endoscopy for 3 months.
Results
We found that most common age group was 51–60 years of age as shown in Table 1. Out of total patients, 64 were males and 36 were females (n = 100). It showed male to female ratio of 1.78/1. None of the patient was reported of age < 30 years. Mean age was 56 years.
Patient most commonly presented with complaint of headache and facial pain (55%) as shown in Fig. 1.
Out of 100 patients, hard palate involvement was observed in 45% patients.
Unilateral presentation was much more common as compared to bilateral. We had seen 68% patients with unilateral presentation and 32% patients with bilateral involvement.
We observed 25% patients with normal vision. 10% patients were able to appreciate finger counting for > 6 m. 17% patients were only able to appreciate hand movements. Even projection of light were absent in 22% patients. 42% patients were observed with normal eye movements while eye movements were restricted in 58% patients as shown in Fig. 2.
Diabetes Mellitus type II was found to be the most common etiological factor associated with mucormycosis as shown in Table 2. 80% patients had Diabetes Mellitus type II. Hypertension, ischemic heart disease and chronic kidney disease was reported in 33%, 9% and 5% patients respectively.
KOH culture of representative tissue revealed presence of fungi in 82% patients, while biopsy suggestive of mucormycosis was reported in all 100 (100%) patients.
Conventional Amphotericin B was required for 14 days in 62% patients. Liposomal Amphotericin B was needed in 20% patients for 14 days. 18% patients required Amphotericin for more than 14 days as shown in Fig. 3.
78% patients required endoscopic debridement via modified denker approach. Conservative endoscopic sinus surgery for the purpose of debridement was performed in about 22% patients. Total 9 patients required eye exentration for complete removal of the disease.
Out of 100 patients, 20 patients were lost to follow up. We reported 20 deaths in our study.
Discussion
None of the patient below 30 years of age has developed mucormycosis post Covid-19 infection. It can be attributed to their immunity and less incidence of comorbidity in young adults. Maximum no. of patients belong to age group of 51–60 years. It may be due to comorbidity associated with age. Mean age was 56 years with male to female ratio of 1.78/1. Similar results were reported by White et al. [4] in his study of 135 adults with median age 57 years and male to female ratio 2.2/1.
Most of the patients (55%) presented with the complaint of headache, facial pain and cheek swelling. Complaint of eye swelling and facial pain were reported by 15% patients. Nasal bleeding, facial numbness and eye swelling with diminution of vision were reported by 5%, 4% and 1% patient respectively. This being rare disease literature is not available for comparison.
Hard palate involvement was observed in 45% patients. Sharma et al. [5] reported palatal involvement in 39% patients in his study of 23 patients with post COVID 19 mucormycosis.
Only 25% patients who presented early had normal vision. Vision gradually deteriorate with the advancement of the disease. In the extreme scenario patients cannot even appreciate projection of light. We reported 22% patients with such an advanced stage who had complete loss of vision. Eye movement was not affected in 42% patients, while eye movements were restricted due to rhino orbital mucormycosis in 58% patients. Unilateral presentation was much more common as compared to bilateral.
Diabetes mellitus type II is most common predisposing factor accounting for 80% cases. Similarly Yohai et al. [6] and Ferry et al. [7] have found diabetes mellitus type II to be the most common predisposing factor. Hypertension and Ischemic heart disease were found in 33% and 9% patients respectively. Immunosuppression due to underlying disease is mainly responsible for secondary infections. Biopsy proved to be gold standard for diagnosis of mucormycosis.
Amphotericin B is the gold standard in the treatment of mucormycosis. The survival rate of patients dramatically has increased to the 60% after the introduction of Amphotericin B [8]. Liposomal amphotericin B is the first choice of treatment in patients with intracranial extension as it crosses the blood–brain barrier more effectively. Most of the patients respond well with Amphotericin B either conventional or liposomal, depending upon the renal status of the patient. Only 5% patients required Amphotericin for more than 14 days who had presented with more advanced disease.
Debridement of necrotic tissue as well as removal of fungal debris is crucial in the treatment of mucormycosis. All patients in our study underwent surgical debridement. Surgery alone has been reported not to be curative, but an aggressive surgical approach has been shown to improve survival [9]. Most of the patients (78%) required medial maxiilectomy via modified denker approach for complete endoscopic removal of the disease. This is attributed to the aggressive and more fulminating nature of the disease. 9 patients with extensive orbital invasion and total loss of vision required orbital exentration. 22% patients were managed via more conservative approached and did not need extensive surgical intervention.
In our study we chose Posaconazole as maintenance antifungal therapy after completion of amphotericin B treatment.
20% patients with more advanced disease could not be revived. Patients who presented at an early stage of disease has shown promising results in terms of survival. Surgery and Injectable Amphotericin B can significantly improve prognosis. Control of underlying disease, systemic antifungal medication and surgical debridement proved to be the mainstay of mucormycosis treatment.
Conclusion
Immune dysregulation caused by COVID 19 infection in addition to widespread use of steroids and broad-spectrum antibiotics may lead to the development mucormycosis. Diabetes Mellitus type II is another important risk factor and the presence of both have additional effect in causing mucormycosis. Thus possibility of invasive secondary fungal infections should always be kept in mind for post COVID-19 patients especially with pre-existing comordity. Headache and facial pain should be considered highly suspicious of mucormycosis. Early diagnosis can significantly improve prognosis. Control of underlying disease, systemic antifungal medication and surgical debridement proved to be the mainstay of mucormycosis treatment.
References
Farnoosh G, Alishiri G, Hossseini Z Sr et al (2020) Understanding the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease (COVID-19) based on available evidence—a narrative review. J Mil Med 22(1):1–11
International Diabetes Federation (2021) IDF sea members http://idf.org/our-network/regions-members/south-east-asia/members/94-india.html. Accessed 27 June 2021
Bouchara J, Oumeziane N, Lissitzky J et al (1996) Attachment of spores of the human pathogenic fungus Rhizopus oryzae to extracellular matrix components. Eur J Cell Biol 70(1):76–83
Pl W, Dhillon R, Cordey A et al (2020) A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa1298
Sharma S, Grover M, Bhargava S et al (2021) Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol 135(5):442–447. https://doi.org/10.1017/S0022215121000992
Yohai R, Bullock J, Aziz A, Markert R (1994) Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol 39(1):3–22
Ferry A, Abedi S (1983) Diagnosis and managementof rhino orbito-cerebral mucormycosis (phycomycosis)—a report of 16 personally observed cases. Ophthalmology 90:1096–1104
Furco A, Mouchet B, Carbonnelle M et al (2001) Pulmonary mucormycosis: benefit of aerosol amphotericin B. Rev Mal Respir 18(3):309–313
Goldstein E, Spelberg B, Walsh T et al (2009) Recent advances in the management of mucormycosis: from bench to bedside. Clin Infect Dis 48:1743–1751
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the Human Research Ethical Committee (HREC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Desai, E.J., Pandya, A., Upadhya, I. et al. Epidemiology, Clinical Features and Management of Rhino Orbital Mucormycosis in Post COVID 19 Patients. Indian J Otolaryngol Head Neck Surg 74, 103–107 (2022). https://doi.org/10.1007/s12070-021-02807-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02807-2