Abstract
To develop an accurate protocol for measuring the Cochlear Duct Length (CDL) by using Multi Detector Computerized Tomography (MDCT) imaging of the temporal bones and thereby make the appropriate choice of electrode for cochlear implantation. 79 MED-EL® Cochlear implantees were divided into three cohorts in chronological order of their implantation. CDL was calculated from MDCT images and correlated with the CDL calculated using the existing Jolly’s formula. Results of the CDL measured by unfurling the cochlea correlated well with the existing formula. In addition to CDL measurement, measuring diameter of each turn, especially the apical turn, helped in choosing the appropriate electrode for complete cochlear coverage. Having dedicated radiographers and neuro-radiologists can avoid inter-observer variations in CDL measurements. Measuring the CDL and the diameter of each turn helps in choosing an appropriate electrode thus minimizing intra-operative difficulties and achieving complete safe insertion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The length of the Organ of Corti (OC) is the distance from its basal to its apical end as measured along the curves of the cochlear spiral. Direct measurement of this dimension of the OC is difficult because of its location within dense bone, and its delicate structure and shape. Hardy et al., in their exclusive study concluded that the Cochlear Duct Length (CDL) varies from 25 to 36 mm with an average of 32 mm [1]. Most of these studies on CDL were done on Caucasian skulls which are larger and highly variant from Indian skulls. In one study by Grover M et al., the average CDL in Indian population was found to be in the range from 28 to 34.3 mm [2].
With advancements in technology and focus on electrode design, a variety of cochlear implant electrodes with varying lengths are available, which can be chosen according to the length of the recipient cochlea. This creates a need to develop an accurate pre-operative technique to determine the length of the cochlea and to choose the appropriate electrode for that patient.
Length of the electrode and hence depth of insertion are important for optimal stimulation of the cochlear neural structures. Basilar membrane is of different thickness and also responds to different auditory inputs in a unique way, with higher frequencies at the basal region and lower frequencies towards its apex [3,4,5]. A long electrode with deep insertion can cause trauma to the delicate cochlear structures, while a shorter electrode will not stimulate all ganglion cells and may lead to poorer performance [6,7,8,9]. Hence, matching the electrode length to the CDL is very important for optimum results [10].
As the concept of preservation of membranous and bony structures within the cochlea has grown in its emphasis, a detailed account of structural variations within the cochlea may provide insights both for the design of electrode arrays and for the surgical strategy [11]. Thus, choosing an appropriate length of electrode becomes important so as to minimize the damage to cochlea and to stimulate it adequately [12].
In our experience of Cochlear Implantation (CI) surgeries at Apollo Hospitals, Bangalore, India, since the year 2006, more than 500 surgeries have been performed. During the early growing years of our CI program, there was no specific radiological protocol in place for CDL measurement. Varying lengths of the cochlear duct (with structurally normal cochlea) ranging from 22 to 30 mm were reported and the lengths did not always correlate with the intra-operative findings. Some of these patients received MED-EL® 31.5 mm standard electrodes that were completely inserted into the cochleae without any resistance. This wide disparity between the reported CDL and the intra-operative observations prompted us to analyze the cause for it. We discovered that several radiographers and radiologists were performing the High Resolution Computerized Tomography (HRCT) of the temporal bones with 3-D reconstruction of the cochleae and analyzing the data, which lead to substantial inter-observer variations in the CDL measurements. In the learning years, Multi-Planar Reconstruction (MPR) and unfurling of the cochleae was performed subjectively by the radiologists and often, apical turn was not included in the measurements. Also, in the initial years of the program, there were no formulae to measure the lengths. Hence, in the current study, certain radiological protocols were laid and results compared with the CDL calculated using the existing Jolly’s formula [13, 14].
CDL can be evaluated by the following methods [15]. 1. Direct method where the length is measured directly from the histologic sections under microscope using a micrometer. This method is also called as surface specimen technique used first by Retzius [1, 16,17,18]. 2. Indirect method is the 2-D reconstruction of the cochlea which was used by Guild in 1921 [1, 16,17,18]. This method uses landmarks from the histologic sections of the cochlea. 3. The 3-D reconstruction method, developed and used by Takagi and Sandol in 1989 and Sato et al. in 1991 [19, 20]. 4. Modeling of the cochlea using a mathematical spiral function. In the current study, we used the 3-D reconstruction method.
Methods
79 MED-EL® cochlear implantees were enrolled for this study. The patients are divided into three cohorts on the basis of chronological order of their implantation performed during the years 2006 to 2015. Three types of CDL values are discussed here. 1. CDL-Old: Pre-operative CDL in the first cohort. 2. MPR-CDL: CDL calculated from the MPR images by unfurling the cochlea. 3. CDL-Cal: CDL calculated using the Jolly’s formula.
Unfurled Cochlea–Mid-Ductal Measurement
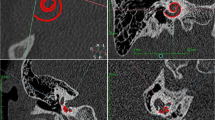
HRCT of the temporal bone was performed using Multi Detector Computerized Tomography (MDCT) (Toshiba Aquillion 64™). Reconstruction of the cochlea was done using curved MPR with slice thickness of 1 mm and mini IP Window width of 4500 and window level of 450 in pre-operative CT and 12,000 for post-operative CT. Unfurling of the cochlea was performed by manually placing the reference points along the outer bony wall margin of cochlea from the round window membrane. Length of the straightened/unfurled cochlea is measured in mid-ductal plane (MPR-CDL) (Fig. 1).
Hardy’s ‘A’ Measurement
A line drawn from the mid-point of the long diameter of the round window through the central axis of the cochlea to the polar-opposite, distant point of the first turn, was measured and was named Hardy’s ‘A’ (Fig. 2). For width measurement of each turn, a line was drawn orthogonal to the line used for the length measurement that subtended the maximal dimension of that turn of the cochlea [14].
‘A’ thus measured was used to calculate complete length of the cochlea using formula given by Alexiades et al. which is 2.5 TL (Turn Length) i = 4.16xA-2.7 [13]. The 2.5TLi thus measured is compared with the MPR-CDL values and based on them, the choice of electrode was made.
Cohort 1
25 MED-EL® implantees who underwent HRCT Temporal bones for various reasons after their cochlear implant surgery were included. All patients had a pre-operative HRCT temporal bone using the same machine and had no cochlear abnormality. CI was performed by the same surgeon; insertion was achieved via round window or extended round window approach. MPR-CDL and CDL-Cal were calculated from the post-operative CT. CDL estimated pre-operatively (CDL-Old) was compared with MPR-CDL and CDL-Cal. As seen in Table 1, the average CDL-old reported pre-operatively was less than MPR-CDL and CDL-Cal. In all the patients, MED-EL® standard electrode with a length of 31.5 mm was used. Electrode insertion was complete and smooth in most of the cases, except a few where complete insertion was not achieved and one or two electrodes were outside the round window. The point to ponder was, with the CDL reported less than 31.5 mm, a complete insertion of 31.5 mm electrode cannot be possible. Literature review on CDL measurements helped in identifying one study by Alexiades et al., 2015 who measured CDL using the formula (2.5 TLi). The same formula (Jolly’s formula) had been used to validate the CDL measurement in the current study. Discussions with radiologists led to a few changes in the CDL measuring protocols. To our satisfaction, the MPR-CDL correlated well with the CDL-Cal. It was also seen that the patients in whom complete insertion was not achieved actually had smaller lengths.
Cohort 2
For the next cohort of 30 patients, CDL was calculated from the MPR of HRCT images acquired from the scans done pre-operatively. These values were compared with the values calculated using the formula. Prospectively, all the remedial measures were applied and electrodes chosen accordingly. However, some difficulty was perceived in achieving complete insertion in two cases (out of 26 Standard 31.5 mm electrodes), in spite of correct CDL measurement and verification with CDL-Cal. It was noted that the diameter of the lumen of the apical turn was less than 0.5 mm in these two patients. The tip dimension of the standard 31.5 mm MED-EL® electrode is 0.5 mm. So, in addition to the CDL measurements, diameters of each turn [basal (Dia-bas), middle (Dia-mid) and apical (Dia-api)] were measured (Fig. 3) and based on these dimensions, electrodes were chosen for complete cochlear coverage (Standard or Flex portfolios).
Cohort 3
For the next cohort of 24 patients, electrode choice was based on both the CDL measurements and diameter measurements.
Results
Data thus obtained was subjected to descriptive and inferential statistical analysis. Results on continuous measurements are presented on Mean ± SD (Min–Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. Pearson correlation between study variables is performed to find the degree of relationship, Pearson correlation co-efficient ranging between -1 to 1, -1 being the perfect negative correlation, 0 is no correlation and 1 means perfect positive correlation.
Significant figures.
+ Suggestive significance (P value: 0.05 < P < 0.10).
* Moderately significant (P value: 0.01 < P ≤ 0.05).
** Strongly significant (P value: P ≤ 0.01).
Statistical software: The Statistical software namely SPSS 18.0, and R environment ver.3.2.2 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs and tables. Study design: A correlation study.
Cohort 1
In the cohort 1, 22 (88%) patients had the value of ‘A’ between 8.5 and 9.5. Only 3 (12%) had A value less than 8.5. 10 (40%) patients had a pre-operatively calculated CDL-old between 21 and 25 mm, 11 (44%) patients had a CDL-old of 26 mm to 30 mm and 4 (16%) patients had a CDL-old of more than 30 mm (Fig. 4). MPR-CDL was found to be between 30 and 35 mm in 20 (80%) patients, less than 30 mm in 1 (4%) patient and more than 35 mm in 4 (16%) patients whereas the CDL-Cal were less than 32 mm in 3 (12%), between 32 and 36 mm in 18 (72%) and more than 36 mm in 4 (16%) patients (Fig. 5). The mean value of ‘A’ in cohort 1 was found to be 8.94 with a standard deviation of 0.46 and the mean CDL-old, MPR-CDL and CDL-Cal were 26.70 mm, 33.60 mm and 34.49 mm respectively (Table 1).
Cohort 2
In the cohort 2, MPR-CDL was found to be between 30 and 35 mm in 21 (70%) patients, less than 30 mm in no patient and more than 35 mm in 9 (30%) patients whereas the CDL-Cal was less than 32 mm in 1 (3.3%), between 32 and 36 mm in 27 (90%) and more than 36 mm in 2 (6.7%) patients (Fig. 5). The mean value of ‘A’ in Cohort 2 was found to be 9.01 with a standard deviation of 0.28 and the mean MPR-CDL and CDL-Cal were 34.21 mm and 34.75 mm respectively (Table 1).
Cohort 3
MPR-CDL was noted to be between 30 and 35 mm in 10 (41.7%) patients and more than 35 mm in 14 (58.3%) patients whereas the CDL-Cal were between 32 and 36 mm in 19 (79.2%) and more than 36 mm in 5 (20.8%) patients (Fig. 5). In the cohort 3, the MPR-CDL values ranged between 31.9 mm and 36.6 mm (Table 1). The values obtained by using the Jolly’s formula (CDL-Cal) were close to the MPR-CDL. They ranged from 32.6 to 36.8 mm with the mean being 35.20 ± 1.07 mm. Average diameters of the three turns, basal, middle and apical were 1.89 ± 0.15 mm, 1.48 ± 0.25 mm and 0.78 ± 0.23 mm respectively (Table 1). The average CDL-Cal was close to the average MPR-CDL obtained by radiologically measuring unfurled cochlea. As the average diameter of the apical turn was 0.78 mm, for cochleae with apical diameter less than 0.5 mm, a Flex28 electrode was used and for cochleae with larger apical diameters, a standard electrode was used.
As seen in Table 2 and Figs. 6 and 7, the Pearson co-efficient (r value) was computed to assess the relationship between the variables MPR-Cal and CDL-Cal in all the cohorts and between MPR-CDL and CDL-Old in the first cohort. All the r values were closer to + 1 and the p value is less than 0.001 which shows significant positive correlation. However, correlation between MPR-Cal and CDL-old in the first cohort is positive but not statistically significant (p value: 0.32).
Discussion
With the advances in cochlear implant surgery and the gaining emphasis on the concept of “soft surgery”, it is important to select the correct size of the electrode array with the best possible compromise between complete cochlear coverage and non-traumatic insertion for the preservation of residual hearing [21]. There has been growing evidence that ‘one size fits all’ theory for electrode array does not achieve optimal hearing outcomes [22].
Accurate measurement of the length of the cochlea is essential to select the appropriate electrode, predict the proper insertion depth for each individual, and for the planning of surgical techniques prior to the surgery.
Evolution of the CDL measurements began from direct methods from histological sections used by Hardy et al., in 1938 to measurements from 3-Dimensional reconstruction of the cochlea using sections from the CT imaging and calculation of the CDL using spiral coefficients [15]. The linear equation developed by Alexiades et al., popularly known as Jolly’s formula has been the standardized measurement protocol being used by most surgeons [13].
During the early stages of our cochlear implant program, there were no standardized protocols in place for the measurement of cochlear sizes. CDL measures provided pre-operatively in the first cohort were not standardized and were given by many radiologists. Advances in imaging technology with HRCT and 3-dimensional reconstructions detect and quantify variations in cochlear anatomy with utmost reliability. With the advancement of these imaging techniques and beginning of the MPR, we began to measure the CDL using the sliced images from HRCT of the temporal bones by taking reference points along the outer wall of the cochlea and unfurling the cochlear spiral. Similar method has been explained by Weurfel et al., who measured CDL from the cone beam computed tomography of temporal bones [23]. They measured the CDL with a starting point at the distal bony rim of the round window and then a 3D curve was set up from the outer edge of the bony cochlea until helicotrema. Uncoiled spiral of the cochlea from the MPR was utilized to calculate the length of the cochlea.
With the advent of a standardized formula to measure the length from a given ‘A’ value, the estimation of the CDL has been systematic all across the world. The same formula has been utilized in our study, to correlate the measurements obtained from the MPR.
Recent advancements in cochlear duct measurements involve proposals of automated method for the measurement of ‘A’ value which is applicable in the Jolly’s formula. Automated ‘A’ and CDL measurements are proposed to be more reproducible (OTOPLAN) and less-time consuming compared to the manual measurements [24,25,26]. However, in our study, ‘A’ value was calculated manually.
In the first cohort, the pre-operatively calculated CDL (CDL-old) was less than 30 mm in 84% of the patients whereas the CDL calculated using MPR on HRCT was found to be less than 30 mm in only one patient. Using the Jolly’s form ula and Hardy’s ‘A’, the CDL was found to be less than 32 mm in 3 (12%) patients. All these patients were implanted with a standard 31.5 mm electrode successfully and without any difficulty. Hence, it was inferred that the older method of calculating the CDL was not accurate.
In the second cohort, the CDL was calculated pre-operatively using both MPR and the formula. 87% (26) of the patients had MPR-CDL and CDL-Cal of more than 33 mm and thus underwent implantation with the standard electrode. Among the 26, in two patients complete insertion up to the marker ring was not achieved and resistance was perceived towards the end of insertion. Retrospectively, it was found that in these patients the diameter of the apical turn of the cochlea was less than 0.5 mm, hence the perceived difficulty. Since the tip of the MED-EL® Standard electrode is 0.5 mm in greatest diameter, apical turn dimensions of less than 0.5 mm would face difficulty in accommodating a 0.5 mm electrode. In such cases a choice of a thinner electrode (Flex 28) should be made.
Importance of deep electrode insertion and apical stimulation has been discussed by Hochmair et al. [6]. They concluded that excitable neural structures exist in the apical region of the cochlea allowing for significant degree of speech perception and discrimination with deep electrode insertions. However, there have been no studies that discuss the measurement of diameter of the apex and its importance in electrode insertions.
In the third cohort, two patients (8%) had CDL less than 33 mm and one patient (4%) had apical turn diameter of 0.5 mm, thus a choice of a thinner electrode (Flex 28) was made in these patients, while others received standard 31.5 mm electrodes. All the patients had complete, smooth electrode insertions.
Based on the ‘A’ value obtained from the radiological imaging, MED-EL® offers various types of electrode array designs for both round window approach and cochleostomy approaches (Fig. 8) [26]. In our study, selection of the electrode array was based on both the apical diameter and the CDL calculated from the Hardy ‘A’ using the Jolly’s formula. Our current recommendation as shown in Table 3, matches well with the company’s recent electrode recommendations based on the Hardy’s ‘A’.
Conclusion
Cochlear size varies in every individual. Accurate measurement of the CDL using an appropriate method is essential to choose a suitable electrode for cochlear implantation. Dedicated radiographers and radiologists are required to perform the unfurling of the cochlea by placing reference points along the outer wall of cochlear duct and taking mid-ductal measurements. This prevents inter-observer variability in measuring cochlear duct lengths. In our study, CDL measured by unfurling the cochlear spiral correlated well with the values from the formula. Choice of an appropriate electrode can be based on the estimated pre-operative CDL values calculated either by unfurling method or by using the formula. In addition, measurement of the diameter of each turn, apical in particular, helps in picking an electrode which is expected to allow for smooth and complete surgical insertion. For cochleae with lesser apical diameter, a shorter flexible electrode with a narrow apical diameter (MED-EL® Flex28) can be chosen, whereas for larger apical diameters, a standard electrode can be preferred. Our recommendations for electrode choice are displayed in Table 3.
These above said protocols are being followed in our institute and appropriate length of electrode is chosen based on pre-operative radiological inputs. The intra-operative findings have been correlating excellently with the radiological measurements given pre-operatively. However, the current study only discusses the decisions made with respect to MED-EL® electrodes while the recipients of cochlear implants made by other companies were excluded from the study.
References
Hardy M (1938) The length of the organ of Corti in man. Am J Anat 62(2):291–311
Grover M, Sharma S, Singh SN, Kataria T, Lakhawat RS, Sharma MP (2018) Measuring cochlear Duct length in Asian population: worth giving a thought! Eur Arch Otorhinolaryngol 275(3):725–728
Roy AT, Penninger RT, Pearl MS, Wuerfel W, Jiradejvong P, Carver C et al (2016) Deeper cochlear implant electrode insertion angle improves detection of musical sound quality deterioration related to bass frequency removal. Otol Neurotol 37(2):146–151
O’Connell BP, Cakir A, Hunter JB, Francis DO, Noble JH, Labadie RF et al (2016) Electrode location and angular insertion depth are predictors of audiologic outcomes in cochlear implantation. Otol Neurotol 37(8):1016–1023
Venail F, Mathiolon C, Menjot de Champfleur S, Piron JP, Sicard M, Villemus F et al (2015) Effects of electrode array length on frequency-place mismatch and speech perception with cochlear implants. Audiol Neurotol 20(2):102–11
Hochmair I, Arnold W, Nopp P, Jolly C, Roland P, Müller J (2003) Deep electrode insertion in cochlear implants: apical morphology, electrodes and speech perception results. Acta Otolaryngol 123(5):612–617
Mistrík P, Jolly C (2016) Optimal electrode length to match patient specific cochlear anatomy. Eur Ann Otorhinolaryngol Head Neck Dis 133:S68-71
Kennedy DW (1987) Multichannel intracochlear electrodes: mechanism of insertion trauma. Laryngoscope 97(1):42–49
Landsberger DM, Mertens G, Punte AK, Van De Heyning P (2014) Perceptual changes in place of stimulation with long cochlear implant electrode arrays. J Acoust Soc Am 135(2):75–81
Gstoettner W, Plenk H, Franz P, Hamzavi J, Baumgartner W, Czerny C et al (1997) Cochlear Implant deep electrode insertion: extent of insertional trauma. Acta Otolaryngol 117(2):274–277
Miranda PC, Sampaio ALL, Lopes RAF, Ramos Venosa A, de Oliveira CACP (2014) Hearing preservation in cochlear implant surgery. Int J Otolaryngol 2014:1–6
Helbig S, Baumann U, Hey C, Helbig M (2011) Hearing preservation after complete cochlear coverage in cochlear implantation with the free-fitting FLEXSOFT electrode carrier. Otol Neurotol 32(6):973–979
Alexiades G, Dhanasingh A, Jolly C (2015) Method to estimate the complete and two-turn cochlear Duct length. Otol Neurotol 36(5):904–907
Escudé B, James C, Deguine O, Cochard N, Eter E, Fraysse B (2006) The size of the cochlea and predictions of insertion depth angles for cochlear implant electrodes. Audiol Neurotol 11(1):27–33
Koch RW, Ladak HM, Elfarnawany M, Agrawal SK (2017) Measuring cochlear Duct length–a historical analysis of methods and results. J Otolaryngol Head Neck Surg 46(1):19
Schuknecht HF (1953) Techniques for study of cochlear function and pathology in experimental animals: development of the anatomical frequency scale for the cat. Arch Otolaryngol Head Neck Surg 58(4):377–397
Walby AP (1985) Scala tympani measurement. Ann Otol Rhinol Laryngol 94(4 Pt 1):393–397
Pollak A, Felix H, Schrott A (1987) Methodological aspects of quantitative study of spiral ganglion cells. Acta Otolaryngol 104(sup436):37–42
Takagi A, Sando I (1989) Computer-aided three-dimensional reconstruction: a method of measuring temporal bone structures including the length of the cochlea. Ann Otol Rhinol Laryngol 98(7):515–522
Sato H, Sando I, Takahashi H (1991) Sexual dimorphism and development of the human cochlea: computer 3-D measurement. SOTO 111(3):1037–1040
Stakhovskaya O, Sridhar D, Bonham BH, Leake PA (2007) Frequency map for the human cochlear spiral ganglion: implications for cochlear implants. JARO 8(2):220–233
Schurzig D, Timm ME, Batsoulis C, Salcher R, Sieber D, Jolly C et al (2018) A novel method for clinical cochlear Duct length estimation toward patient-specific cochlear implant selection. OTO Open 2(4):2473974X1880023
Würfel W, Lanfermann H, Lenarz T, Majdani O (2014) Cochlear length determination using cone beam computed tomography in a clinical setting. Hear Res 316:65–72. https://doi.org/10.1016/j.heares.2014.07.013 (Epub 2014 Aug 11 PMID: 25124151)
Iyaniwura JE, Elfarnawany M, Riyahi-Alam S, Sharma M, Kassam Z, Bureau Y, Parnes LS, Ladak HM, Agrawal SK (2017) Intra-and Interobserver variability of cochlear length measurements in clinical CT. Otol Neurotol 38(6):828–832. https://doi.org/10.1097/MAO.0000000000001411 (PMID: 28383464)
Rivas A, Cakir A, Hunter JB, Labadie RF, Zuniga MG, Wanna GB, Dawant BM, Noble JH (2017) Automatic cochlear Duct length estimation for selection of cochlear implant electrode arrays. Otol Neurotol 38(3):339–346. https://doi.org/10.1097/MAO.0000000000001329 (PMID:28146009;PMCID:PMC5335919)
Khurayzi T, Almuhawas F, Sanosi A (2020) Direct measurement of cochlear parameters for automatic calculation of the cochlear duct length. Annals of Saudi Medicine 40(3):212–218. https://doi.org/10.5144/0256-4947.2020.218
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutt, S.N., Gaur, S.K., Vadlamani, S. et al. Evolving a Radiological Protocol for Cochlear Duct Length Measurement: Three Audit Cycles. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 3998–4006 (2022). https://doi.org/10.1007/s12070-021-02774-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02774-8