Abstract
Chronic Otitis Media is the most common cause of hearing impairment with ear discharge with which patients report to any otologist. The aim of management in such cases is to provide a safe ear and restore the hearing by Tympanoplasty. Many materials have been used for ossicular reconstruction, including both biological and synthetic materials. Minimally destroyed ossicle can be utilized for Ossiculoplasty while in case of complete destruction of ossicles, synthetic materials may be used such as teflon, titanium, hydroxyapatite etc. To evaluate the outcome of Ossiculoplasty using autograft versus synthetic graft. A prospective study done using non-probability convenience method of sampling involving a group of 50 patients were subjected to Tympanoplasty with Ossiculoplasty. Intra operative decision was taken on the type of graft to be used for Ossiculoplasty and the patients were divided into two equal groups, A (autograft) and B (synthetic graft) of 25 each. The patients were thereafter evaluated post surgery at periodic intervals of 3, 6 and 12 months. The improvement in hearing following surgery was significant (AB gap < 20 dB) in the range of 72% in Group A to 84% in Group B of patients 12 months after surgery. Also there was a 37% change in AC in Group A as compared to 40% in Group B, demonstrating marginally better improvement in hearing with synthetic graft as compared to autograft. The patients have significant improvement in hearing thresholds after ossiculoplasty with both autograft and synthetic graft. Teflon is an excellent alternative for ossiculoplasty when autologous incus is not available for use due to disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
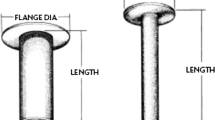
Chronic Otitis media (COM) is a chronic inflammatory disease that affects the middle ear and the mastoid leading to partial or complete loss of tympanic membrane (TM) and ossicles, which manifests as conductive hearing loss [1]. Cholesteatoma and chronic otomastoiditis are common causes of erosion of the ossicles mostly affecting incudostapedial joint with loss of the lenticular process or complete loss of some portion of the distal incus. However the entire long process of the incus along with the stapes superstructure can also be eroded in some cases of extensive cholesteatoma [2]. Surgical removal of the affected ossicles during cholesteatoma removal also causes ossicular discontinuity. In most instances this involves the entire incus and the head of the malleus [2]. Tympanoplasty is a surgical procedure which eradicates disease from the middle ear along with reconstruction of the hearing with or without repair of the TM. Ossiculoplasty is the operation to restore the hearing mechanism by ossicular chain reconstruction. To enhance binaural input to auditory centers, the hearing thresholds of the diseased ear should be within 15 dB after surgery. Various options for ossicular reconstruction are there and surgeon must choose his prosthesis based on the best chance of hearing restoration and the lowest chance of complications. There are many factors which affect the outcome of surgery such as the type of material used for ossiculoplasty, eustachian tube function, extent of disease and the degree of hearing loss. Amongst these, material used for tympanoplasty is an important factor in determining the long term hearing results. There are many types of materials including biological and synthetic which have been used for ossicular reconstruction. Biologic materials include ossicles, cortical bone and cartilage and synthetic materials include gold, titanium, Teflon, hydroxyapatite, ceramics and plastipore. Incus body is the most commonly used autograft material which is often reshaped to fit between the handle of malleus and the stapes. Sometimes malleus head may be used when incus is not available [3]. Autograft ossicle is inexpensive, safe and helps in primary reconstruction in all patients undergoing chronic ear surgery. Autograft materials are sometimes not available for reconstruction as an ossicle may have microscopic squamous epithelium infiltration and may lead to recividism. Also operative time is long to obtain and shape the autologous graft to appropriate size, resorption may occur with cartilage, and possible fixation to the adjacent walls of the tympanic membrane and middle ear. Because of these disadvantages of autograft materials, synthetic materials were introduced in ossicular reconstruction. Studies have shown improved hearing post ossiculoplasty using bone and cartilage graft [4] and extrusion rate in these studies were very low. There are also studies demonstrating the difficulties in terms of it being a technically challenging procedure requiring long intra-operative time for harvesting, fashioning and reconstructing the graft. There are other studies using synthetic grafts for ossiculoplasty and having advantage of being a technically straight forward procedure, readily available and having no risk of leaving behind any residual disease [5]. There still exists a considerable difference of opinion in using either type of graft in terms of selection of graft material, graft remodeling intra-operatively, extrusion rates and post operative hearing outcome. So this study was done to comprehensively evaluate the outcome of ossiculoplasty using autograft versus synthetic graft.
Materials and Methods
This was a prospective study done using non-probability convenience method of sampling carried out in a tertiary care hospital over a period of 2 years and included 50 patients. The study was approved by the Institutional Ethical Committee. The patients were categorized into 02 groups. Patients in Group A (25 patients) underwent ossicular reconstruction using sculptured autograft ossicle (malleus or incus) and Group B (25 patients) underwent ossicular reconstruction using synthetic graft (Teflon). Senior surgeon operated in all the cases. The decision to use autograft or synthetic was taken intraoperatively. If the ossicle was found to be minimally destroyed, it was refashioned and used for ossiculoplasty. If ossicles were completely destroyed, then synthetic graft (Teflon) was used for reconstruction.
Inclusion Criteria
-
1.
Patients with symptoms of Chronic Otitis Media, Cholesteatoma patients with Austin Type A defects.
-
2.
Hearing loss of more than 30 decibels air bone gap.
-
3.
Patient with no active discharge for more than 3 weeks.
-
4.
Patients in the age group 15–45 years.
Exclusion Criteria
-
1.
Patient with an acute exacerbation of Chronic Otitis Media.
-
2.
Patients with sensorineural hearing loss.
-
3.
Patients with bilateral Chronic Otitis Media where the ear to be operated is the only hearing ear.
-
4.
Extensive cholesteatoma patients with Austin Type B, C, D.
Research Design

where S-1, subjective and objective evaluation done prior to surgery; T-1, subjective and objective evaluation at 3 months after surgery; T-2, subjective and objective evaluation at 6 months after surgery; T-3, subjective and objective evaluation at 1 year after surgery.
All the patients were subjected to history, otological examination, examination under microscope and pure tone audiometry. Following this, the patients were taken up for Tympanoplasty with Ossiculoplasty. Post aural approach was used in majority especially for perforations located in the anterior quadrant of the tympanic membrane. Few patients underwent the surgery by the end aural approach. If the ossicle was found to be minimally destroyed, it was refashioned and used for Ossiculoplasty. If ossicles were completely destroyed, then an synthetic graft (Teflon) was used for reconstruction. To prevent extrusion of graft, a thin slice of cartilage with perichondrium intact on one side was placed medial to Temporalis graft. The post operative assessments of the patients were done at 3, 6 months and 1 year after the surgery. The post-operative assessment included the evaluation of the symptoms on the basis of improvement in hearing using PTA.
Statistical Analysis
Comparison of the hearing results between the two groups were done using following tests:
-
Symptomatic improvement in hearing after surgery using t-test.
-
The Average hearing threshold (air conduction) pre-operative and post-operative at 3, 6 months and one year was analyzed.
-
ABG in PTA after surgery was done using the t-test.
SPSS 10.0 was used to perform the statistical tests. P value < 0.001 was considered significant.
Results
The age of patients in this study varied between 15 and 45 years. The mean age in Group A was 31.24 years (SD 8.98) and in Group B was 30.84 years (SD 8.75). In both groups majority of patients were males (Group A-56%, Group B- 52%). The predominantly affected ear was the right side in both the groups (Group A-60%, Group B-64%). Average Pure Tone hearing threshold (AC) and Air–Bone gap (A-B gap) were recorded pre-operatively and post-operatively in both the groups by taking an average of 500 Hz, 1 and 2 kHz. This was taken as baseline for recording quantitative improvement in hearing post-operatively. Post-operative PTA was done after 3/6/12 months. In Group A, hearing loss was the symptom in all the 25 patients and after ossiculoplasty using autograft (Ossicle), improvement was seen in 80% at the end of 3 months of surgery. This improvement was enhanced further after 6 months with 88% of the patients experiencing a better or same hearing as compared to that prior to surgery. In Group B, hearing loss was the symptom in all 25 patients and after ossiculoplasty using synthetic graft (Teflon), the improvement was seen in 84% at the end of 3 months of surgery. This improvement was enhanced further after 6 months with 96% of the patients experiencing a better or same hearing as compared to that prior to surgery. In the 50 patients with hearing loss studied, it was found that the average pre-operative air conduction (AC) was 42.2 dB (SD 11.46) and 43 dB (10.41) in Group A and B respectively (Fig. 1). Upon comparing the improvement in AC during the post operative period in Group A, it was found that there was a 29.3% change, from 42.2 to 29.8 dB at the end of 3 months (T1). The same change in Group B was 30.7% (43–29.8 dB) demonstrating a marginally better improvement in hearing using allograft as compared to autograft. After 6 and 12 months post operative follow-up, it was found that AC improved by 37% in Group A and by 40% in Group B again demonstrating an even better outcome using teflon (Table 1). Pre-operatively in Group A, 36% of patients had an AB gap between 10 and 20 dB, 40% between 21 and 30 dB and 24% had > 30 dB. Similarly in Group B, 24% of patients had an AB gap between 10 and 20 dB, 60% between 21 and 30 dB and 16% had > 30 dB (Table 2). Post operatively at 3 months, Group A showed an improved AB gap in 100% patients (64% in 10–20 dB range and 36% in 21–30 dB range). Similarly Group B also showed 100% improvement. (80% in 10–20 dB range and 20% in 21–30 dB range) (Table 3). Post operatively at 6 and at 12 months, Group A showed an improved AB gap in 100% patients (72% in 10–20 dB range and 28% in 21–30 dB range). Similarly Group B showed a 100% improvement too (84% in 10–20 dB range and 16% in 21–30 dB range). It was seen that the improvement in AB gap was more in the Group B with the synthetic graft as compared to Group A with the autograft (Table 4).
In our study, no cases of graft extrusion or displacement were encountered. The AB gap closure was faster and better with synthetic graft, though P-value was not significant. Use of synthetic graft saved time and provided maximum surgical ease, though equally good results are achieved with both autograft and synthetic graft.
Discussion
COM is the most common cause of hearing impairment with ear discharge with which patients report to any otologist. The aim of management in such cases is to provide a safe and dry ear and restore the hearing, by Tympanoplasty which may be combined with ossiculoplasty. Tympanoplasty involves removal of disease from the middle ear and reconstructs the tympanic membrane and ossicular chain. The goal is a stable, reliable connection between the tympanic membrane and the stapes and to achieve good hearing result. The are various studies done previously to evaluate the results of ossciuloplasty, but the outcomes are quite variable and surgeons are still not clear with the type of surgery, type of graft most suitable for poor and low socioeconomic population. In this study with 50 patients (25 per Group A and B) were enrolled who underwent tympanoplasty with ossiculoplasty for COM. The mean age was 31.24 years in Group A and 30.84 years in Group B. Age does not alter the success rates of Ossiculoplasty in our study and it was also concluded in the study done by Fukuchi et al. [6]. The common symptoms in patients who presented with COM, as seen in this study in Group A were hearing loss (100%) and ear discharge (92%). Other less common symptoms were earache (32%), tinnitus (16%) and giddiness or vertigo (4%). In Group B, the main symptoms were hearing loss (100%) and ear discharge (88%). Other less common symptoms were earache (20%), tinnitus (12%) and giddiness or vertigo (8%). Ear discharge was present in all patients, followed by decrease hearing (84%) in this study. After ossiculoplasty using autograft (Ossicle), hearing improvement was seen in 80% at the end of 3 months of surgery which enhanced further to 8% at the end of 6 months. In Group B, hearing loss was the symptom in all 25 patients. After Ossiculoplasty using Teflon, the improvement was seen in 84% at the end of 3 months of surgery which enhanced further to 96% at the end of 6 months. Robert C O’reilly et al. in their study [7] showed that with the use of autograft incus he had achieved a mean postoperative AB gap of 18.6 dB. The study by K. Ojala [8] attained a mean AB gap of 25.8 dB. Our study achieved a mean post operative AB gap of 15.8 dB using autograft ossicle and 14.2 dB using teflon, Teflon. Iurato [4] reviewed the literature at length to investigate hearing results from ossicular reconstruction in Austin-Kartush type A patients. Success was 84 vs. 82% for incus interposition vs allograft at one year of follow-up. Hillman [9] published a retrospective review of 84 patients undergoing tympanoplasty with the Plastipore prosthesis and 53 with the titanium. The air-bonbe gap was less than 20 dB in 60% of patients in the Plastipore group while in the titanium group, 45.3% of the patients achieved a 20 dB or less air–bone gap. In another study by Emir [10], autologous incus had 58% success rate and plastipore had 56% success rate with 9.3% implant extrusion. House JW in his retrospective study of ossicular reconstruction with Hydroxyapatite and Plastipore TORP (560 patients) and PORP (650 patients) achieved AB gap within 10 dB in 68% patients with PORP and 58% patients with TORP. The extrusion rate in his study was 4% and statistically less when it was combined with cartilage reconstruction [11]. Success in ossiculoplasty depends on the skills of the operating surgeon and case selection [12]. The results of ossiculoplasty are improving with less complications and no cases of graft extrusion [13, 14]. In our study also there were no cases of graft extrusion the improvement in hearing outcome (Group A-72%, Group B-84%) at end of 6/12 months was significant and consistent with other studies (ranging between 56 and 84%) [12,13,14,15]. It was further observed that the air conduction and Air Bone gap closure was marginally better with the Teflon than with the ossicle. The sample size in our study was small and follow up period was less. Further prospective long term RCTs with large sample size are required to assess the ossiculoplasty outcomes to choose an ideal ossicular prosthesis.
Conclusion
Both autograft (Incus) and synthetic graft (Teflon) provide significant improvement in hearing outcomes. Teflon is an excellent alternative for ossiculoplasty when autologous incus is not available for use due to disease.
Abbreviations
- COM:
-
Chronic otitis media
- ABG:
-
Air bone gap
- TM:
-
Tympanic membrane
- SD:
-
Standard deviation
- dB:
-
Decibels
- PTA:
-
Pure tone audiometry
References
Bluestone CD, Gates GA, Klein JO et al (2002) Panel reports: 1. Definitions, terminology, and classification of otitis media. Ann Otol Rhinol Laryngol 111:8–18
Charles W et al (2010) Cummings otolaryngology head and neck surgery, 4th edn, Elsevier Mosby, New York
O’Reilly R (2005) Ossiculoplasty using incus interposition: hearing results and analysis of the middle ear risk index. Otol Neurotol 26:853–858
Iurato S (2001) Hearing results of ossiculoplasty in Austin-Kartush group A patients. Otol Neurotol 22(2):140–144
Gardner EK (2004) Results with titanium ossicular reconstruction prostheses. Laryngoscope 114(1):65–70
Fukuchi I, Cerchiari DP, Garcia E, Rezende CE, Rapoport PB (2006) Tympanoplasty: surgical results and a comparison of the factors that may interfere in their success. Braz J Otorhinolaryngol 72(2):267–271
Smyth G (1971) Long term results of middle ear reconstructive surgery. J Laryngol Otol 85(12):1227–1230
Ojala K, Sorri M, Vainio-Mattila J, Sipila P (1983) Late results of tympanoplasty using ossicle or cortical bone. J Laryngol Otol 97:19–25
Hillman TA (2003) Ossicular chain reconstruction: titanium versus plastipore. Laryngoscope 113(10):1731–1735
Emir H (2008) Ossiculoplasty with intact stapes: analysis of hearing results according to the middle ear risk. Acta Otolaryngol 31:1–7
House JW (2001) Extrusion rates and hearing results in ossicular reconstruction. Otolaryngol Head Neck Surg 125(3):135–141
Albu S, Babighian G, Trabalzini F (1998) Prognostic factors in tympanoplasty. Am J Otol 19:136–140
Laha P, Prasad B (2013) A study of Ossiculoplasty in chronic otitis media using different types of prosthesis. Bengal J Otolaryngol Head Neck Surg 21(2):13–15
Lieder A, Issing W (2014) Hearing benefit in allograft tympanoplasty using tutoplast processed malleus. Int J Otolaryngol 2014:931308
Kumar S, Yadav K, Ojha T, Sharma A, Singhal A, Gakhar S (2018) To evaluate and compare the result of ossiculoplasty using different types of graft materials and prosthesis in cases of ossicular discontinuity in chronic suppurative otitis media cases. Indian J Otolaryngol Head Neck Surg 70(1):15–21
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Ethical Approval
Study approved by Ethical Committee of the Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, K., Nagamani, Y.S., Kour, A. et al. A Comparative Prospective Study to Evaluate Outcomes of Ossiculoplasty using Autograft Versus Synthetic Graft. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 511–516 (2022). https://doi.org/10.1007/s12070-020-02360-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02360-4