Abstract
To assess the parameters’ setting of the microscope during parotidectomy and the impact of microscopic parotidectomy on facial nerve functional status. A prospective study was conducted on 28 patients in a tertiary care center, who underwent microscopic parotidectomy. Microscope’s settings’ like magnification, focal length, diameter of the visualized field, and clock position were recorded. Facial nerve functional status was also recorded. All surgeries were performed by right-handed surgeons using Leica F 20 M525 microscope. Clock position of microscope for right parotidectomy ranged between 7 and 10 o clock and for left, it ranged between 7 and 12 o clock. Magnification ranged between 1.3 × and 3.2 ×; magnifications of 1.3 × and 1.8 × were preferred from incision to separation of parotid from sternocleidomastoid muscle, 1.8 × and 2 × for dissection of the facial nerve trunk, and 2 × and 3.2 × for individual branches of the facial nerve. Focal length ranged between 251 and 410 mm and the diameter of the visualized field ranged between 7 and 14.7 cm. Out of 24 cases of benign lesions, 2 (8.3%) developed facial paresis which resolved in 3 months. Two out of four cases of malignancy developed permanent palsy as nerve branches were sacrificed to achieve tumor clearance. Using a microscope for parotidectomy is advantageous for facial nerve dissection, reducing chances of facial paralysis. The microscope was also found to be useful for teaching. The use of appropriate microscopic parameters avoids the glitch of transition from open to microscopic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of salivary gland neoplasms originate from parotid [1]. Complete tumor removal with preservation of all facial nerve branches is the primary goal of surgery for parotid neoplasms. Temporary and permanent facial nerve paralysis have been reported following parotidectomies and are considered the most troublesome complications for surgeons as well as patients. The reported incidence of temporary facial paresis is 25 and 60% while permanent facial palsy is 2–6% [2,3,4,5,6]. Malignant parotid neoplasms are usually associated with a higher rate of postoperative facial palsy [1]. Accurate identification of facial nerve trunk and careful tracing of its branches is the key to preserving facial nerve function.
Antegrade and retrograde facial nerve dissection, as well as nerve monitor, have been advocated as ways to identify facial nerve during parotidectomy. Significance of using facial nerve monitor for facial nerve identification and preservation is still debatable as some studies quote in favor of its positive role while others could not find any role [7, 8].
Parotidectomy has conventionally been an open surgery performed without the use of magnification [2, 3, 9]. Few studies mention about the use of the microscope in parotidectomy but do not mention about surgical settings of the same [1, 5, 10, 11].
In the present study, authors report their experience of performing parotidectomy under microscopic vision focusing on surgical settings of the microscope and its outcomes primarily in relation to the facial nerve.
Materials and Methods
A prospective study was conducted involving 28 patients who underwent microscopic parotidectomy in our department in a tertiary care hospital between August 2018 and February 2020. The preoperative evaluation involved a detailed medical history, clinical examination (including facial nerve functional status), fine needle aspiration cytology (FNAC) and contrast-enhanced magnetic resonance imaging (CEMRI) in all patients. The patient underwent superficial or total parotidectomy depending on the extent of lesion and cytology. All surgeries were performed by surgeons with at least 5 years of experience in the parotid, microscopic ear, and laryngeal surgery. All surgeons were right-handed.
The patient was positioned in 15 degrees reverse Trendelenburg. A head ring was placed and extension was provided at shoulders using a sandbag. Surgery was performed using a Leica F 20 M525 microscope. The monitor of the microscope was positioned to help assistant surgeons to visualize surgery. All surgeries were performed with surgeons in a standing position (Fig. 1). Headend and foot end were considered as 12’O clock and 6′ O clock positions respectively. The mid-point between eyepieces of the microscope was considered as the clock position of the microscope. Magnification and focal length as displayed on the microscopic system, which gave the optimum vision to the operating surgeon at each step, were recorded. The diameter of microscopic light in the surgical field was recorded by an assistant surgeon using a sterile surgical scale which corresponded with the visualized field in the microscope. The specific steps at which recordings of prior mentioned parameters were done included skin incision, flap elevation, separation of parotid from the anterior border of sternocleidomastoid & cartilaginous external auditory canal, delineation of the posterior belly of digastric, identification of the main trunk of facial nerve and tracing of individual branches of the facial nerve.
The use of monopolar cautery was restricted to surgical steps till the exposure of the tragal pointer; after which, bipolar cautery with fine tip was used (Electronic supplementary file 1, which demonstrates dissection of nerve branches using bipolar cautery). Cautery use was avoided during flap elevation in the submandibular region to prevent injury to the marginal mandibular branch.
All branches of the facial nerve were checked for their functional status in the immediate post-operative period as soon as the patient was conscious enough to respond and on the first postoperative day (Electronic supplementary file 2, which demonstrates facial nerve functional status in immediate post-operative period). The presence of abnormal functional status of the facial nerve on the first post-operative day was considered as paresis which was graded as per the House-Brackmann scale [12]. All patients with paresis were re-assessed for its status at 3 weeks, 6 weeks, 3 months until the complete resolution or latest till 9 months whichever was earlier.
Results
The mean age of patients was 40.1 years and male to female ratio was 1.54:1. The type of parotidectomy performed and their number along with corresponding histology have been mentioned in Table 1. Pleomorphic adenoma was the most common pathology followed by Warthin’s tumor and mucoepidermoid carcinoma. Right parotidectomy was performed in 13 (46.4%) patients while left in 15 (53.6%) patients.
For the right parotidectomy, the microscope was positioned on the left side and the surgeon stood on the right side (Fig. 1); the preferred direction of instrumentation during facial nerve dissection was from below upwards. For the left parotidectomy, the microscope was positioned on the right side, the surgeon stood on the head end of the table during facial nerve trunk dissection and the preferred direction of instrumentation during dissection was from above downwards. Table 2 mentions the surgeon’s position and the microscope’s parameters. A lower magnification allowed a wider field to operate on and vice versa; hence magnification changed as per the area of dissection. Higher magnification was preferred for dissection of the facial nerve and its branches. During the identification of the main trunk of the facial nerve, the tragal pointer and posterior belly of digastric were kept in the field of vision which was achievable even with a high magnification of 3.2 × but was used only (in 4 cases) when the trunk was not identifiable with a lower magnification.
Table 3 mentions the status of facial nerve function in the postoperative period and on follow up. The mean follow-up was 12.17 ± 3.42 months. The maximum follow-up period was 18 months and a minimum of 6 months.
Discussion
Had the facial nerve not been crossing through the parotid gland, parotidectomy would never have been a charming as well as a challenging surgery. Time and again, there have been modifications to the surgical concepts of parotidectomy with almost all having the common goal of facial nerve preservation [2, 13]. Surgical technique, use of accessory equipment, tumor pathology, and its extension appear to be the determining factors for the post-operative functional status of the facial nerve [10, 11, 13].
The gold standard method of treatment of parotid gland tumors is superficial parotidectomy and/or total conservative parotidectomy [14,15,16]. Literature also advocates the role of limited parotidectomy or focused extracapsular tumor dissection for a benign parotid lesion to minimize facial nerve complications [13, 17, 18]. Witt et al. and Colella et al. in their studies mention a higher rate of tumor recurrence after extracapsular dissection compared to superficial parotidectomy while Albergotti et al. do not mention a difference in this aspect [4, 19, 20]. Superficial parotidectomy is also advantageous in terms of reduced chances of residual metachronous Warthin’s tumor and avoidance of parotid asymmetry [1]. In this study, superficial parotidectomy was done for all lesions of the superficial lobe to minimize the risk of recurrence.
The use of microscope and nerve monitor as accessories to help identify and protect the facial nerve has been mentioned in studies showing a variable incidence of temporary and permanent facial paralysis signifying uncommon conclusions (Table 4). Microsurgical dissection of the facial nerve was first mentioned by Nicoli et al. [21]. Their study mentioned no cases of permanent facial palsy. The study by Carta F et al. mentions microscope assisted parotidectomy with simultaneous use of facial nerve monitor resulting in 2.7% incidence of permanent facial palsy in parotid lesion not involving the nerve and zero incidences of facial palsy in benign extra-facial parotid lesions [1]. Factors such as the use of electrocautery, use of muscle relaxants during anesthesia, and neurological disorders may affect responses of nerve monitor resulting in the unreliability of facial nerve identification; while, a microscope is independent of these factors [7]. We used a microscope as the sole equipment for identification of facial nerve and its branches which produced comparative results for benign lesions of the parotid. As there were only 4 malignant parotid lesions in this study, the results of malignant lesions are not comparable.
The transition from a non-aided vision to an aided vision for a surgeon is a learning curve. Proper microscope positioning, appropriate magnification, and focal length adjustment as per the corresponding area of surgical dissection help a surgeon to quickly and comfortably adjust to this transition. These also help in maintaining proper ergonomics during surgery and hence avoiding the possible musculoskeletal problems in the future. For right-sided lesions, microscope position adjustment needed during various steps ranged between 7′O and 10’O clock. For left-sided lesions, the same ranged between 5’O clock and 12’O clock (Table 2). 12’O clock is the preferred position to identify facial nerve trunk on the left side for a right-handed surgeon and hence range of movement on the left side is more. In our study, all surgeons were right-handed. For a left-handed surgeon, the microscopic positions should possibly reverse. All procedures performed in the study were with the same microscope and hence a change of microscope may change its adjustment parameters within a minimal range of our experienced settings.
While using a microscope, the surgeon needs to adjust to the magnified focused view of one region with a simultaneous blurring of the surrounding surgical field, handling of instruments, and restricted assistance of the assistant surgeon. Surgeons in our study had the experience of performing microscopic ear, laryngeal, and thyroid surgeries, hence using the microscope in parotidectomy was not uncomfortable.
A centrifugal approach of facial nerve dissection was followed in all cases, aiming at identification of facial nerve trunk first followed by tracing its branches. The facial nerve trunk and its branches were located accurately using the microscope in all cases. Though the surgeons never attempted to identify the peripheral branches initially, in 6 cases peripheral branches (4 marginal mandibular nerve and 2 lower buccal nerve branch) could be identified using the microscope after flap elevation. Hence it also explains a possible better peripheral nerve branch delineation as compared to unaided vision while a retrograde approach of nerve dissection is followed during parotidectomy. Nicoli et al. [21] mention retrograde dissection using marginal mandibular nerve as an initial landmark in all their cases of microscope assisted parotidectomy.
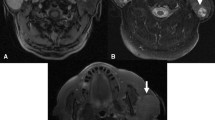
The branching pattern of the facial nerve is quite variable which can be confirmed only intra-operatively [22, 23]. Variation in branching pattern and the number of communicating branches mandates a cautious dissection of all individual branches to preserve the facial nerve function in toto (Fig. 2) (also watch Electronic supplementary file 3, which demonstrates facial nerve branching pattern in one of the cases). A magnified vision with microscopic assistance helped in the identification of nerve and its branches including minute communicating ones which were not appreciable with naked eyes, as well as their differentiation from fibrous strands eliminating the dilemma of dissecting tissue immediately superficial to the nerve. It also helped in avoiding unnecessary traction of nerve branches which may result in temporary paresis. The microscope also aided in good visualization and hence preservation of perineural vascularity of facial nerve branches, damage to which may affect nerve function. Good visualization of vessels running through parotid helped achieve good hemostasis while simultaneously avoiding inadvertent cauterization of parotid tissue; even minimum bleeding looks magnified under the microscope and may pose trouble to the surgeon.
Duration of resolution of temporary facial paralysis post-parotidectomy varies between 20 days to 18 months [1, 2, 11]. In the study by Nicoli et al. [21], all cases of temporary facial paralysis resolved within 3 months, while the study by Eviston et al. [2] mentions a maximum duration of 18 months for resolution of temporary facial paralysis. With a preserved anatomy of the facial nerve, it’s deficit should resolve within 12 weeks beyond which chances of resolution are less [1, 24]. In this study, out of 4 cases with temporary paresis, 1 resolved in 3 weeks, 2 in 3 months, and 1 in 6 months (Table 3). The variable duration of transient paralysis may be explained by variations in the degree of nerve stretch during surgery, degree of injury to neural vascularity which runs close to the nerve, and presence of communicating nerve branches.
A microscope with an attached monitor is an excellent teaching tool for parotid surgery. As the area of dissection is narrow particularly during delineation of facial nerve trunk and its branches, an unaided demonstration restricts the number of residents who can be taught as well as may require halting the surgery for the same. Using a microscope helps teach multiple residents at the same time with optimum visualization of all structures, this is very important to quicken their learning curve. The average surgical duration in the study was less compared to other studies (Table 4).
The only disadvantage of using a microscope is the equipment cost. However, microscope being essential surgical equipment in otolaryngology practice does not add much to the overall expenditure and carries an advantage over nerve monitor in this aspect. Reduced surgical complications related to the facial nerve with the use of microscope outweigh the cost factor in our opinion.
The lacuna of our study is a small sample size which has resulted in a very small number of patients with malignant parotid lesions. Hence, our results can’t be extrapolated to the malignant category.
Conclusion
Authors recommend the use of a microscope in all parotidectomies as it was associated with reduced incidences of both, temporary and permanent facial paresis in this study. Proper settings of microscope’s parameters as experienced by us are advocated to skip the initial hurdle in the shift from open to microscopic approach. The microscope also serves as a good teaching tool.
Data Availability
Yes.
References
Carta F, Chuchueva N, Gerosa C, Sionis S, Caria RA, Puxeddu R (2017) Parotid tumours: clinical and oncologic outcomes after microscope-assisted parotidectomy with intraoperative nerve monitoring. Acta Otorhinolaryngol Ital 37(5):375–386
Eviston TJ, Yabe TE, Gupta R, Ebrahimi A, Clark JR (2016) Parotidectomy: surgery in evolution. ANZ J Surg 86(3):193–199
Mehle ME, Kraus DH, Wood BG et al (1993) Facial nerve morbidity following parotid surgery for benign disease: the Cleveland Clinic Foundation experience. Laryngoscope 103:386–388
Witt RL, Rejto L (2009) Pleomorphic adenoma: extracapsular dissection versus partial superficial parotidectomy with facial nerve dissection. Del Med J 81:119–125
Guntinas-Lichius O, Klussmann JP, Wittekindt C, Stennert E (2006) Parotidectomy for benign parotid disease at university teaching hospital: outcome of 963 operations. Laryngoscope 116:534–540
Koch M, Zenk J, Iro H (2010) Long-term results of morbidity after parotid gland surgery in benign disease. Laryngoscope 120:724–730
Meier JD, Wenig BL, Manders EC, Nenonene EK (2006) Continuous intraoperative facial nerve monitoring in predicting postoperative injury during parotidectomy. Laryngoscope 116:1569–1572
Makejev M, Venail F, Cartier C, Garrel R, Crampette L, Guerrier B (2005) Continuous facial nerve monitoring during pleomorphic adenoma recurrence surgery. Laryngoscope 115:1310–1314
Marshall AH, Quraishi SM, Bradley PJ (2003) Patients’ perspectives on the short- and long-term outcomes following surgery for benign parotid neoplasms. J Laryngol Otol 117:624–629
Grosheva M, Klussmann JP, Grimminger C et al (2009) Electromyographic facial nerve monitoring during parotidectomy for benign lesions does not improve the outcome of postoperative facial nerve function: a prospective two-center trial. Laryngoscope 119(12):2299–2305
Savvas E, Hillmann S, Weiss D, Koopmann M, Rudack C, Alberty J (2016) Association between facial nerve monitoring with postoperative facial paralysis in parotidectomy. JAMA Otolaryngol Head Neck Surg 142(9):828–833
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93:146–147
Mantsopoulos K, Koch M, Klintworth N, Zenk J, Iro H (2015) Evolution and changing trends in surgery for benign parotid tumors. Laryngoscope 125(1):122–127
Woods JE (1985) Parotidectomy versus limited resection for benign parotid masses. Am J Surg 149:749–750
Alajmo E, Polli G, De Meester W (1989) Total parotidectomy–a routine treatment for parotid gland swellings? J Laryngol Otol 103:181–186
Valentini V, Fabiani F, Perugini M et al (2001) Surgical techniques in the treatment of pleomorphic adenoma of the parotid gland: our experience and review of literature. J Craniofac Surg 12:565–568
O’Brien CJ (2003) Current management of benign parotid tumors? The role of limited superficial parotidectomy. Head Neck 25:946–952
McGurk M, Thomas BL, Renehan AG (2003) Extracapsular dissection for clinically benign parotid lumps: reduced morbidity without oncological compromise. Br J Cancer 89:1610–1613
Colella G, Cannavale R, Chiodini P (2015) Meta-analysis of surgical approaches to the treatment of parotid pleomorphic adenomas and recurrence rates. J Craniomaxillofac Surg 43:738–745
Albergotti WG, Nguyen SA, Zenk J et al (2012) Extracapsular dissection for benign parotid tumors: a meta-analysis. Laryngoscope 122:1954–1960
Nicoli F, D’Ambrosia C, Lazzeri D et al (2017) Microsurgical dissection of facial nerve in parotidectomy: a discussion of techniques and long-term results. Gland Surg 6(4):308–314
Kopuz C, Turgut S, Yavuz S, Ilgi S (1994) Distribution of facial nerve in parotid gland: analysis of 50 cases. Okajimas Folia Anat Jpn 70(6):295–299
Gataa IS, Faris BJ (2016) Patterns and surgical significance of facial nerve branching within the parotid gland in 43 cases. Oral Maxillofac Surg 20(2):161–165
Dulguerov P, Marchal F, Lehmann W (1999) Postparotidectomy facial nerve paralysis: possible etiologic factors and results with routine facial nerve monitoring. Laryngoscope 109:754–762
Funding
None.
Author information
Authors and Affiliations
Contributions
AB: Conceptualization, Methodology, Original draft preparation. RS: Data collection, Methodology. MM: Methodology, Review, Editing. MP: Methodology, Review. AKT: Draft revision, study design. AK: Draft revision, study design. SV: Supervision, Review. AS: Original draft preparation
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical Statement
All of the procedures performed in this study were in accordance with the ethical standards of our institution and with the Helsinki Declaration of 1975, as revised in 2008. The protocol for the investigation has been approved by the Institutional Review Board and written informed consent was obtained from each participant or each participant’s guardian.
Code Availability
Not applicable.
Ethics Approval
This retrospective review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Study has been approved by Institutional review board (letter no. 3017396/2020/05/03/2020).
Consent to Participate
:Informed consent was obtained from all individual participants/legal guardians included in the study.
Consent for Publication
:Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM_1 Dissection of facial nerve branch using bipolar cautery (MP4 30927 kb)
ESM_2 Facial nerve functional assessment in immediate post-operative period (MP4 9726 kb)
ESM_3 Facial nerve branching pattern as visualized under the microscope (MP4 63455 kb)
Rights and permissions
About this article
Cite this article
Bhardwaj, A., Sood, R., Malhotra, M. et al. Microscopic Parotidectomy: A Prospective Study. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2273–2280 (2022). https://doi.org/10.1007/s12070-020-02106-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02106-2