Abstract
Despite minimally invasive neck dissection (MIND) being popular technique, there is a paucity of literature emphasizing its safety and efficacy. In this meta-analysis, we compared the efficacy and safety of MIND over CND techniques in treating oral/head and neck cancer. We systematically searched PubMed, MEDLINE, Embase, from database inception to January, 2019 for the relevant studies comparing MIND and CND. Two independent reviewers performed quality check and data were extracted for primary outcomes to assess length of hospital stay, duration of surgery, intraoperative blood loss and retrieved lymph nodes. Drainage volume and duration, length of incision, satisfaction of scar and safety were the secondary outcomes. We analyzed the outcomes using standard mean differences (SMDs) and the relative risk that were pooled using random effect meta-analysis. Out of 144 studies, 17 met the final inclusion criteria. MIND technique has shown better overall efficacy with outcomes compared to CND except with duration of surgery (SMD 1.82, 95% CI 0.47–3.17). Lesser hospital stay, better nodal yield and less intra-operative blood loss was observed with MIND over CND. Duration and volume of wound drainage was comparably less in MIND with smaller length of incision. Postoperative complications were less and tolerable with MIND approach with superior cosmetic outcomes. MIND via endoscopic or robotic approach is safe and efficacious with equitable oncological outcomes in terms of lymph nodes yield compared to CND, but it requires longer surgery duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, Minimally Invasive Neck Dissection (MIND) performed endoscopically or robotically for treating head and neck cancer have made a remarkable progress not only with better oncological outcomes, but also functional outcomes, lesser morbidity and improved quality of life [1,2,3]. Considering minimally invasive surgery for head and neck cancer could be challenging due to complex anatomy, narrow working space and close proximity of vital structures. After the advancement in endoscopic techniques and FDA approval of da Vinci system for head and neck cancer surgery in 2009, the advantages of this minimally invasive approaches have been utilized. Conventional Neck Dissection (CND), which includes Radical Neck Dissection (RND), Modified radical Neck Dissection (MND) or Selective Neck Dissection (SND) is still being the standard and integral part of oral, head and neck cancer treatment which involves resection of draining group of lymph nodes. However, CND being safe and have lower risk of regional recurrence, it is associated with significant post-operative morbidities and shoulder dysfunction. MIND procedure has advantages with respect to efficacy, safety and cosmetic benefits [4, 5].
MIND, along with patient desire for aesthetically acceptable scar and surgeon concern for better functional and cosmetic results without compromising on oncological effectiveness compared to CND, minimally invasive techniques have several advantages to patients as well as surgeons. Which includes smaller incisions, lesser risk of infection, decreased pain and hospital stay with better scar satisfaction to patients. Whereas, the robotic instruments enhanced the dexterity and degree of freedom for the surgeon to operate along with three-dimensional visualization [6].
As the main purpose of these minimally invasive techniques is to hide the scar of head and neck surgery, several remote access approaches were considered which includes transoral, transaxillary, modified facelift, retro auricular or past auricular facelift approach [7].
Despite the increased adoption of this technique, there is a paucity of literature and studies available are mostly confined to South Korea. Considering the popularity of MIND technique, it is imperative to assess its efficacy compared to CND. In this study, we systematically reviewed the relevant studies which preferred MIND and CND techniques for oral/head and neck cancer and performed meta-analysis among the comparative studies between MIND and CND techniques and synthesize data in terms of safety and efficacy.
Materials and Methods
This systematic review and meta-analysis (PROSPERO ID: CRD42019124586) conformed to the “Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)” guidelines (Fig. 1).
Study Design and Participants
A comprehensive scientific literature searched using PubMed, EMBASE and Cochrane library databases were conducted for articles published till January 2019 using following search strings: (oral cancer AND neck dissection) AND (“minimally invasive” OR “minimally invasive neck dissection” OR “robotic neck dissection” OR “endoscopic assisted neck dissection.”
The initial screening of the articles was performed based on the title and abstract, followed by full-text examination of initially included article to assess the relevance according to the defined inclusion/exclusion criteria. Two reviewers independently carried out article screening process, discrepancy and disagreements were resolved by third party. Prospective and retrospective studies comparing minimally invasive neck dissection techniques (robot or endoscopic assisted) with conventional neck dissection and also single arm prospective/retrospective studies where the patients were administered the novel techniques were included. Articles published in English-only were included in the study. Other study designs (case reports, reviews, meta-analysis, etc.), studies with insufficient statistical data and repeated studies that contained the same patient cohorts were excluded.
Data Extraction and Quality Assessment
Two independent reviewers extracted data from included studies regarding author, year of publication, study design, study population (total as well as group-wise), demographics of the study population, oncological outcomes in terms of efficacy and safety to standardized MS Office Excel based data extraction sheets. The primary outcome of interest in this study were length of hospital stay, duration of surgery, intraoperative blood loss and retrieved lymph nodes. Secondary outcomes were drainage volume and duration, length of incision, satisfaction of scar and safety analysis, in terms of adverse events (AEs).
The methodological quality of the eligible studies was determined by Methodological Index for Non-Randomized Studies (MINORS) [8] criteria and publication bias in this meta-analysis was evaluated using funnel plots for duration of surgery, intraoperative blood loss and hospital stay. Authors of the study were contacted to resolve any discrepancy or unclear data reported.
Statistical Analysis
Statistical analysis for meta-analysis was done by using ‘R’ software. Descriptive statistics was used to present the baseline parameters. All continuous variables were presented as means (standard deviation, SD), medians (range) and percentages. For comparative studies, time related outcomes were presented as mean (SD) or median (range). The values between MIND and conventional techniques was presented as mean difference or standardized mean difference and 95% confidence interval (95% CI). For single intervention/arm studies, the time for MIND and relevant outcomes were pooled and provided as mean (SD). Safety of the surgical techniques was compared in terms of relative risk (RR) and 95% CI.
The potential heterogeneity among the studies was determined via Cochran’s Q-statistic and I2 statistics. If the P value for heterogeneity was < 0.05 or I2 was > 50%, the heterogeneity will be statistically significant. Safety was determined in terms of event rates and risk ratio (RR) with 95% CI.
Results
Study Selection
Characteristics of The Included Studies
The present systematic review included a total of 17 studies with data obtained on 620 patients altogether for the analysis. Out of which, nine studies compared MIND with CND in which 2 were retrospective and 7 were prospective in nature. Eight studies were of single arm with only MIND in which 5 studies were retrospective and 3 were of prospective setting. In total, 10 were prospective and 7 were of retrospective setting. The demographic characteristics of the studies are summarized in Table 1. The total number of patients ranged from six to 113, whereas, the sample size for MIND and CND ranged from 6 to 75 and from 16 to 43, respectively. The median age ranged from 27.33 to 62.5 and 56 to 63.2 for the patients who underwent MIND and CND, respectively. Among the gender, percentage of male patients ranged from 50% to 85.7% and female from 14.28% to 77.77% for the MIND group. Whereas, in CND group, males ranged from 42.85% to 80% and females from 1.5% to 46%. Median follow-up duration ranged from 1.5 to 35.7 months in MIND group and from 1.5 to 37.3 months in CND group.
Quality Assessment and Publication Bias
For comparative studies, the score ranged from 19 to 20 (ideal score 24) and score range of 11–13 (ideal score 16) was obtained for non-comparative studies. Greater the MINORS score indicates greater the quality of the included studies. In most of the studies, assessment of the study outcomes were not blinded.
Relatively lesser publication bias was found as depicted in the resultant funnel plot as standard error for all was within acceptable range (funnel) (Fig. 2), except for hospital stay.
Efficacy and Safety Outcomes of Comparative Studies
Primary Outcomes
Length of Hospital Stay
Length of hospital stay was evaluated and compared in seven studies between MIND and CND group (Fig. 3). Random effects meta-analysis showed a statistically significant difference between MIND and CND with respect to length of stay in hospital, with an SDM of −0.52 (95% CI −0.89 to −0.16; p = 0.0045) indicating patients undergoing MIND will have significantly less duration of hospital stay when compared to patients undergoing CND.
Duration of Surgery
Eight studies evaluated and compared operative time between MIND and CND groups (Fig. 4). Random effects meta-analysis demonstrated a statistically significant longer operative time for MIND approach compared to the conventional approach, with a total SDM of 1.82 (95% CI 0.47–3.17; p = 0.0082). The 95% CI suggested high confidence with a large effect size. I2 of 96.3% indicated a high degree of heterogeneity among the studies. Operative time was significantly prolonged in the MIND group compared to the CND group.
Intraoperative Blood Loss
Five studies evaluated and compared intraoperative blood loss between MIND and CND group. The SDM for blood loss during surgery was −0.25 (95% CI: −0.82, 0.32; p = 0.39) indicating MIND undergoing patients experienced less blood loss compared to CND group of patients. However, this association was not found to be statistically significant (Fig. 5).
Retrieved Number of Lymph Nodes
A total of seven studies estimated the number of lymph nodes yielded during pathological examination between MIND and CND. There was no significant difference between MIND and CND with respect to the retrieved number of lymph nodes (p = 0.7323). However, the SDM value was favoring MIND though the difference was statistically not significant (SDM −0.06; 95% CI: −0.38, 0.27) (Fig. 6).
Secondary Outcomes
Drainage Duration and Volume
Six studies analyzed drainage duration and five studies estimated the volume of drainage in patients undergoing MIND and CND. The SDMs for drainage duration and volume were −0.22 (95% CI: −0.65, 0.21, p = 0.32) and −0.23 (95% CI: −0.71, 0.26, p = 0.36) respectively. A reduction in drainage duration and volume in patients undergoing MIND compared to CND group was observed, however a statistically significant difference was not observed with both the outcomes (p = 0.32 and 0.36 respectively) (Fig. 7a and b).
Length of Incision
Two studies evaluated length of incision in MIND and CND group. There was a significant difference in incision length between the two study groups (p = 0.03). The SDM for Length of incision was −7.5 (95% CI: −14.48, −0.62) indicating patients in MIND group had a significantly smaller length of incision compared to conventional group (Fig. 8).
Satisfaction of Scar
Cosmetic satisfaction of the scar was assessed using a non-validated scale of grade 1–5, considering highest score 5 as ‘extremely satisfied’ or depending upon the study. In our study, satisfaction with the scar after the surgery was assessed in 2 comparative studies. Patients undergoing MIND surgery expressed more satisfaction of scar when compared to CND group with an SDM of 1.44 (95% CI: −0.09, 2.97), however, this association between the MIND and CND was not statistically significant (p = 0.064) (Fig. 9).
Nodal recurrence rate at follow-up was studied in 6 comparative studies between MIND and CND. Of which, four studies showed no nodal recurrence in the MIND group. One study (lira, 2017) compared disease free survival (DFS) between MIND and CND approach with no statistical difference between the groups.
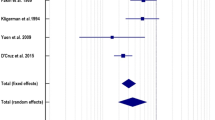
Safety Outcomes in Terms of Surgical Complications
Postoperative complications varied across all 17 included studies. The common complications observed were numbness of earlobe, temporary mouth corner deviation, seroma/hematoma, wound infection and chyle leakage. Overall, the evidence suggested lower rates of all the above complications (except for temporary mouth corner deviation) in MIND group than with conventional group, but the differences observed were not statistically significant (Fig. 10). The relative risk and p values for numbness of earlobe, seroma/hematoma, wound infection and chyle leakage were 0.72 (95% CI: 0.16, 3.21, p = 0.6), 0.6 (95% CI: 0.21, 1.75, p = 0.35), 0.31 (95% CI: 0.03, 2.88, p = 0.3), 0.64 (95% CI: 0.21, 1.96, p = 0.4) respectively. Nevertheless, there was no report of serious adverse events (AEs) and the AEs reported were tolerable. Also, there was no report of any surgery related death in both the techniques.
Forest-plot of the relative risk of adverse events (AEs) associated with MIND versus conventional technique. CI confidence interval, SDM standard difference mean, LL lower limit, UL upper limit, RE random effect, FE fixed model, MIND Minimally Invasive Neck Dissection; CND Conventional Neck Dissection
Pooled Analysis of Single Arm Studies (MIND Group)
A total of 8 studies evaluated the efficacy of MIND alone. Among them, five were retrospective and three were prospective studies (Table 2).
Discussion
As the management of the clinical palpable lymph nodes is essential in the treatment of head and neck cancer especially in case of clinical N0 neck cancer [9], a method with better post-operative outcomes and cosmetic benefits is preferred. Minimally invasive approaches including robotic or endoscopic technique are used in many surgical subspecialties for the treatment of cancer, especially in head and neck cancer [1].
Gagner [10] introduced minimal invasive technique using endoscopy. Narrow workplace and difficulties in dissecting deeper levels by using minimal invasive technique via laparoscopic or endoscopic approach are resolved by performing robotically using retro-auricular and modified facelift approach. Various studies using minimally invasive techniques to treat head and neck cancer have demonstrated efficacy, safety and cosmetic benefits over CND [11,12,13]. Kim et al. in 2012 by introducing robotic neck dissection technique for head and neck squamous cell carcinoma showed good cosmetic and surgical outcomes [14]. Later Kim et al. in 2014 proved the convenience of operating node positive head and neck cancer through retro-auricular or modified facelift approach [15].
This systematic review and meta-analysis was designed to assess the efficacy and safety of MIND technique in oral/head and neck cancer compared to CND. In our study, we analyzed nine comparative studies between MIND and CND for efficacy and safety outcomes. Our data showed the postoperative outcomes of MIND are comparable to CND approach with major disadvantage being the longer duration of surgery. This could be attributed to the time-consuming skin flaps elevation and retractor placement, docking of the da Vinci system, aligning of robotic or endoscopic instruments and also steep learning curve. With increased operative time, the patient has to be under general anesthesia for longer duration which might add to the post-operative complications. These drawbacks can be overcome in future with experience of the surgeon with minimally invasive techniques.
Length of hospital stay was significantly lesser with MIND compare to CND due to faster recovery from minimally invasive surgery. Better immune preservation with minimally invasive approaches with reduction in inflammatory mediator like serum IL-6 and CRP level post-operatively which are elevated due to surgical trauma and stress among patients undergoing CND can be resolved by minimally invasive approaches [16].
In our study, length of incision for MIND was significantly small compared to CND and lesser intra operative blood loss was observed in MIND. Meticulous dissection with small incision performed from the surgeon using MIND techniques could to be attributed for these outcomes, which might have also resulted in lesser drainage volume and duration in our study. CO2 insufflation carried out during the surgery could be the other contributing factor for lower intra-operative blood loss as CO2 has a compression effect on neck vessels [17].
Retrieved number of lymph nodes from MIND approach was not statistically significant from that in the CND. A slight increase in number of lymph nodes yield was observed with MIND might not confirm the oncologic safety but shows the feasibility of the technique. Though some studies [18,19,20] have compared nodal yield as proxy factor for oncological outcomes, long term data regarding overall survival and disease free survival are required to measure true oncological outcomes.
The main advantage of MIND is its capability in presenting cosmetically acceptable scar along with superior efficacy and safety compared to CND. Today cancer patients are cautious about cosmetic appeal particularly with oral/head and neck cancer surgery scars which is aesthetically unacceptable. Whereas, with CND, a long scar over the neck, along with wound related complications are inevitable.
In our study, satisfaction with the surgical scar was assessed by two comparative studies, stating better scar satisfaction with MIND [5, 15]. Both studies performed neck dissection by modified facelift or retro-auricular approach using robotic technique and compared the outcomes including the cosmetic benefits. Satisfaction with the scar was mainly due to aesthetically acceptable scar and the access to the incision site was away from the post-operative radiation field without affecting normal lymphatic drainage. The study also states the advantage of this approach in preserving lymphatic drainage which is significantly disrupted by transverse anterior neck incision of head and neck cancer [15]. However, cosmetic scores were evaluated using non-validated scales hence the interpretation of the scores should be done with caution.
Our meta-analysis showed lower rates of post-operative complications which reflects the safety associated with MIND. Patient under gone MIND have shown lesser post-operative complication which includes numbness of earlobe, (except temporary mouth corner deviation), seroma/hematoma, wound infection and chyle leakage compared to CND. However, none of them were found to be statistically significant. Major post-operative complications were rare. Transient marginal nerve palsy was observed with 11% of participants with robotic-assisted surgery group which was resolved in couple of months [12]. Surgical site wound infection, 2 cases with permanent marginal branch paresis and 5 cases with transient paresis was observed in one study [21]. Other minor peri-operative outcomes associated with neck dissection including injury of marginal mandibular branch of the facial nerve, skin flap, skin burn/necrosis, button hole, lymphocele, facial paresis and surgical wound related infections were observed.
In our study, eight single arm studies evaluated the efficacy and safety of MIND (endoscopic and robotic) in the treatment of head and neck cancer.
Mean values of length of hospital stay, duration of surgery, intra-operative blood loss, retrieved lymph node, drainage volume and duration and length of incision of single arm studies were comparable with that of MIND approach in 2-arm studies. Mean values for duration of surgery in single arm studies was observed to be 181.4 min whereas in 2-arm studies, a mean value of 152.47 min.
Various studies among the single arm have used endoscopic technique in the treatment of head and neck cancer [4, 11, 22,23,24]. The major advantage with endoscopic surgeries were excellent cosmetic outcomes and it is cost effective compared to robotic neck dissection. A 3-year retrospective study of 45 cases conducted in India [11] showed the benefits of endoscopic technique compared to CND in terms of safety and efficacy. The resultant scar from this approach below the clavicle using minimally invasive technique has shown an excellent cosmetic benefit as the scar wound heals fast and lies inside the patient’s clothing. This technique could be an excellent tool for cancer-afflicted and resource-limited settings with oncological benefits, low-cost and lesser scar.
To avoid the long visible transcervical incision which is inevitable with CND, Liang et al. placed a small lateral neck incision through endoscopic approach to treat early stage head and neck squamous cell carcinoma. With 3-years follow-up results, this minimally invasive technique was found to be safe and feasible with better oncological outcomes [22].
Byeon et al. demonstrated the retro-auricular or modified facelift selective neck dissection using laparoscopic approach and suggest this cost-effective alternate treatment option to those who find robotic surgery as expensive [23].
However, MIND via endoscopic approach have certain technical disadvantages which includes narrow working space, which can lead to few or more collisions between the operator and the assistant and limited degree of motion with rigid manually operated instruments in a narrow and angled working space. Limited 2-dimensional vision through an endoscope might lead to unclear view of anatomical structures. And also, physiological tremors could amplify along the length of rigid endoscopic instruments.
To overcome these shortcoming of the endoscopic technique, robotic-assisted surgery using da Vinci surgical systems has been implemented in various surgical subspecialties including head and neck surgery. Byeon et al. showed the feasibility of robotic surgery in treatment of head and neck cancer with excellent cosmetic benefits [13].
There are certain advantages of robotic technique which include improved dexterity and endowrist function with high degree of motion with better hand–eye co-ordination to the surgeon. Physiological tremor can be greatly reduced with the use of appropriate filters. Another remarkable advantage is the enhanced 3-dimensional vision enables the surgeon to identify and dissect anatomical structures [6]. There are few disadvantages to these robotic techniques. First and foremost is the cost associated with these robotic systems which are very expensive and that makes it unaffordable to setup and maintain these systems in many resource-poor settings. And, of course the requirement of extra skilled staff could be the other limitation.
There are few limitations in our study. Most of the studies were carried out in South Korea, except three studies [11, 17, 25]. So, the results obtained from these findings should be cautiously extrapolated to the general population. In nine comparative studies, patients were given the option to choose MIND or CND and additional cost associated with MIND was informed in prior. Also, cosmetic benefits with MIND being one of the major advantages, the scale used to measure the scar satisfaction scores were not validated and hence this might affect the interpretation of study findings.
In conclusion, MIND performed via laparoscopic or robotic technique have better outcomes in terms of length of hospital stay, interoperative blood loss, number of lymph nodes retrieved but significant longer operative time compared to CND. Drainage volume and duration and length of incision was also lesser with MIND compared to CND. MIND approach was also considered safe with less and tolerable post-operative complications. Additionally, cosmetic benefits with better scar satisfaction are the advantages of MIND. However, MIND can only be recommended given the cost of care beyond the potential benefits.
References
Goh HKC, Ng YH, Teo DTW (2010) Minimally invasive surgery for head and neck cancer. Lancet Oncol 11(3):281–286
Dziegielewski PT, Teknos TN, Durmus K, Old M, Agrawal A, Kakarala K et al (2013) Transoral robotic surgery for oropharyngeal cancer: long-term quality of life and functional outcomes. JAMA Otolaryngol Head Neck Surg 139(11):1099–1108
Lee J, Kwon IS, Bae EH, Chung WY (2013) Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab 98(7):2701–2708
Woo SH, Kim JP, Baek C-H (2016) Endoscope-assisted extracapsular dissection of benign parotid tumors using hairline incision. Head Neck 38(3):375–379
Lee HS, Kim WS, Hong HJ, Ban MJ, Lee D, Koh YW et al (2012) Robot-assisted Supraomohyoid neck dissection via a modified face-lift or retroauricular approach in early-stage cN0 squamous cell carcinoma of the oral cavity: a comparative study with conventional technique. Ann Surg Oncol 19(12):3871–3878
Lanfranco AR, Castellanos AE, Desai JP, Meyers WC (2004) Robotic surgery. Ann Surg 239(1):14–21
Möckelmann N, Lörincz BB, Knecht R (2016) Robotic-assisted selective and modified radical neck dissection in head and neck cancer patients. Int J Surg Lond Engl 25:24–30
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 3(9):712–716
D’Cruz AK, Vaish R, Kapre N, Dandekar M, Gupta S, Hawaldar R et al (2015) Elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med 373(6):521–529.
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83(6):875
Nayak SP, Devaprasad M, Khan A (2019) Minimally invasive neck dissection: a 3-year retrospective experience of 45 cases. J Minimal Access Surg 15(4):293–298
Ji YB, Song CM, Bang HS, Park HJ, Lee JY, Tae K (2017) Functional and cosmetic outcomes of robot-assisted neck dissection by a postauricular facelift approach for head and neck cancer. Oral Oncol 70:51–57
Byeon HK, Holsinger FC, Kim DH, Kim JW, Park JH, Koh YW et al (2015) Feasibility of robot-assisted neck dissection followed by transoral robotic surgery. Br J Oral Maxillofac Surg 53(1):68–73
Kim WS, Lee HS, Kang SM, Hong HJ, Koh YW, Lee HY et al (2012) Feasibility of robot-assisted neck dissections via a transaxillary and retroauricular (“TARA”) approach in head and neck cancer: preliminary results. Ann Surg Oncol 19(3):1009–1017
Kim WS, Byeon HK, Park YM, Ha JG, Kim ES, Koh YW et al (2015) Therapeutic robot-assisted neck dissection via a retroauricular or modified facelift approach in head and neck cancer: a comparative study with conventional transcervical neck dissection. Head Neck 37(2):249–254
Fan S, Zhong J-L, Chen W-X, Chen W-L, Li Q-X, Wang Y-Y et al (2017) Postoperative immune response and surgical stress in selective neck dissection: comparison between endoscopically assisted dissection and open techniques in cT1-2N0 oral squamous cell carcinoma. J Cranio Maxillo Fac Surg 45(8):1112–1116
Raj R, Lotwala V, Anajwala P (2016) Minimally invasive supraomohyoid neck dissection by total endoscopic technique for oral squamous carcinoma. Surg Endosc 30(6):2315–2320
Lemieux A, Kedarisetty S, Raju S, Orosco R, Coffey C (2016) Lymph node yield as a predictor of survival in pathologically node negative oral cavity carcinoma. Otolaryngol Head Neck Surg 154(3):465–472
Jaber JJ, Zender CA, Mehta V, Davis K, Ferris RL, Lavertu P et al (2014) A multi-institutional investigation of the prognostic value of lymph nodal yield in advanced stage oral cavity squamous cell carcinoma (OCSCC). Head Neck 36(10):1446–1452
Ebrahimi A, Zhang WJ, Gao K, Clark JR (2011) Nodal yield and survival in oral squamous cancer: defining the standard of care. Cancer 117(13):2917–2925.
Lira RB, Chulam TC, de Carvalho GB, Schreuder WH, Koh YW, Choi EC et al (2018) Retroauricular endoscopic and robotic versus conventional neck dissection for oral cancer. J Robot Surg 12(1):117–129
Liang F, Fan S, Han P, Cai Q, Lin P, Chen R et al (2017) Endoscopic-assisted selective neck dissection via small lateral neck incision for early-stage (T1–2N0M0) head and neck squamous cell carcinoma: 3-year follow-up results. Surg Endosc 31(2):894–900
Byeon HK, Holsinger FC, Koh YW, Ban MJ, Ha JG, Park JJ et al (2014) Endoscopic supraomohyoid neck dissection via a retroauricular or modified facelift approach: preliminary results. Head Neck 36(3):425–430
Huang X, Sun W, Liu X, Liu W, Guan Z, Xu Y et al (2009) Endoscope-assisted partial-superficial parotidectomy through a concealed postauricular skin incision. Surg Endosc 23(7):1614–1619
Albergotti WG, Byrd JK, Nance M, Choi EC, Koh YW, Kim S et al (2016) Robot-assisted neck dissection through a modified facelift incision. Ann Otol Rhinol Laryngol 125(2):123–129
Funding
This manuscript received no funding.
Author information
Authors and Affiliations
Contributions
Study design and concept: S.P.N.; data acquisition and interpretation: V.S.R.; manuscript: S.P.N., B.G., A.S.
Corresponding author
Ethics declarations
Availability of data and material
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Code Availability
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nayak, S.P., Sreekanth Reddy, V., Gangadhara, B. et al. Efficacy and Safety of Novel Minimally Invasive Neck Dissection Techniques in Oral/Head and Neck Cancer: A Systematic Review and Meta-Analysis. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2166–2176 (2022). https://doi.org/10.1007/s12070-020-02066-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02066-7