Abstract
To assess the quality of life in head and neck cancer patients and the various factors which affect the quality of life in head and neck cancer patients was the main aim of the study. A prospective longitudinal study with a sample size of 130 patients was done within the time period of one and a half years. Patients with biopsy proven squamous cell carcinoma of the head and neck were treated as per their treatment protocol either by combined modality or single modality. Follow up at the completion of treatment was done and the quality of life questionnaire was filled out. QoL was assessed pre-treatment and at 4 times at different stages of follow up period. Demographic data was also taken into consideration for comparison which showed that head and neck cancer is more common in the males (80%) between the age group of 35–50 years, chronic tobacco chewers (45%) with most common site of cancer being the oral cavity (61%). Majority of the patients presented at Stage IV of their disease (35%) with largest HRQoL changes seen within the first three months after commencement of treatment. The most debilitating modality of treatment was Surgery + CTRT. Detailed assessment of the various factors which hamper the QoL in head and neck cancer patients should be done by which we can provide quality care and a completely new view into the health care experience and improving patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality of life (QoL) is a multi-dimensional concept and it includes domains related to physical, mental, emotional, and social functioning [1]. A related concept of QoL is well-being, which assesses the positive aspects of a person’s life, such as positive emotions and life satisfaction [2]. It is associated with the individual’s degree of satisfaction found in family life, love life, social and environmental life, and the very existential sense [3].
The notion of QoL has become increasingly important in patient treatment, particularly in oncology where treatment rarely offers complete recovery and there is limited life expectancy. For head and neck cancer (HNC), the principle domains to achieve are mainly survival with improvement of QoL [4]. Health related Quality of Life (HR-QoL) plays a more important role in HNC patients than in any other group of cancer patients. This is because of the possibility of obviously debilitating physical problems as well as the psychological effects of change in body image and loss of function. Patients with HNC, besides harboring a disease which is life threatening, also have to deal with the impact of treatment on numerous aspects of QoL including functional disturbances such as speech, swallowing, hearing, breathing, associated with social interaction, which hold a crucial importance in the individuals life [5].
Worldwide, HNC accounts for more than 550,000 cases and 380,000 deaths annually [6]. Head and neck cancer is the commonest cancer in India and consists of about one-third of all cancers [7]. According to the Indian Council of Medical Research (ICMR) Atlas, approximately 0.2 to 0.25 million new HNC patients are diagnosed each year [8].
Several QoL domains are immensely affected by the treatment regimens for head and neck cancer patients. Treatment may be carried out by means of surgery, radiotherapy, chemotherapy or a combination of these modalities. Permanent mutilations, loss of organs and/or changes to their functions may be caused by surgical interventions. Radiotherapy, with or without chemotherapy may cause transient side effects, which may subside at the end of treatment but prove to be nonetheless very much limiting to the patient [9]. These effects all play a fundamental role in the alteration of the patients well-being which may all trigger a negative impact on the QoL of these individuals [10].
A quantitative assessment of the outcome of treatment protocols in head and cancers still remains elusive. Although quality of life is an important treatment outcome in HNC, cross-study comparisons have been hampered by the heterogeneity of measures used and the fact that reviews of HNC QoL instruments have not been comprehensive to date [11].
Quality-of-life assessment in head and neck cancer is still in its infancy. There is still a need for a clear consensus about which QoL measures are important and whether they can be applied across geographic, spiritual and cultural boundaries. To assess the QoL of the patients affected by HNC it is important to understand the impact of the disease and its treatment in the patient’s daily routine, and improve the care protocol with more encompassing clinical, social and rehabilitation support measures [12]. Hence, the need is required for such studies as a whole for quality of life for HNC patients. It will not only tell us the final end point of the current management protocol, but it would also help us in making amendments to the same [13].
Materials and Methods
Subject Recruitment Criteria
Inclusion Criteria
-
All patients diagnosed with primary squamous cell carcinoma of the head and neck region who have undergone either of the following treatments (surgery, chemotherapy or radiotherapy or combination of any) were included pretreatment and during their follow-up period of 3 months, 6 months, 9 months and 12 months.
Exclusion Criteria
-
Patients who were not able to maintain follow up either personally or telephonically
-
Cases having recurrence or residual cancer within 6 months post treatment.
Methodology
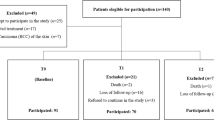
It was a prospective longitudinal study with a sample size of 130 patients within the time period of one and a half years at the Dept. of ENT and Head & Neck Surgery, Shri Krishna Hospital. Participants were treated as per their treatment protocol either by combined modality (Surgery + CT/RT or Surgery + CTRT) or by single modality (Surgery/CT/RT). Follow up at the completion of treatment—post-surgery and/or post-radiation/chemotherapy was done and the quality of life questionnaire was filled out.
QoL was assessed pre-treatment and at 4 times at different stages of follow up period of 3 months, 6 months, 9 months and 1 year of post treatment. Demographic data like age, gender, addictions, staging of the tumour, site of primary, treatment modalities and pretreatment factors like psychological status and other variables were also taken into consideration for comparison as per proforma. We used the original and validated Gujarati version of FACT Head and Neck Questionnaire for which prior permission was taken from the author [Chart 15 of electronic supplementary material].
Detailed analysis of the QoL of all of the patients in the study was done and a comparison was made of the overall QoL scores with respect to each specific domain taking all other variables, which have been included in the proforma, into consideration.
Observations and Results
Observations made from the study are as follows:
Out of 130 cases, 80% were male and 20% were female. According to the distribution of cases according to age, 6 cases were in the age group of 20–35 years, 65 cases were in the age group of 36–50 years and 59 cases were in the age group of more than 50 years of age. According to the distribution of cases according to site of primary tumour, 79 cases had a primary tumour in the oral cavity, 15 had a primary tumour in the oropharynx, 13 cases had a primary tumour in the larynx and 23 cases had a primary tumour in the hypopharynx.
According to the type of addiction, 45% of cases had addiction to tobacco chewing, 32% had addiction of smoking, 17% had addiction to sniffing and 6% of the cases gave no history of any addiction. The distribution of cases according to presence of comorbidity showed that 16% had Hypertension, 6% had Diabetes Mellitus, 5% had multiple comorbidities and 73% of the cases showed no comorbidities. 26 cases had Stage I disease, 41 cases had stage II disease, 17 cases had stage III disease and 46 cases had stage IV disease.
Out of a total of 130 cases, 32% underwent Surgery + Adjuvant Radiotherapy, 31% underwent Surgery Adjuvant Chemoradiotherapy, 17% underwent Chemoradiotherapy, 11% underwent radiotherapy, 7% underwent only surgery, 1% underwent neoadjuvant chemotherapy + surgery and 1% underwent chemoradiotherapy followed by salvage surgery.
The QoL curve shows that the largest HRQoL changes for head and neck cancer patients were seen within the first 3 months after commencement of treatment in our study. But even after 1 year post-treatment none of the variables returned completely to the pretreatment values. The maximum changes in QoL were seen for the head and neck domain as compared to the other domains [Chart 1 of electronic supplementary material].
ANOVA TEST results shows that there is a statistically significant role of gender in the QoL of HNC patients in which female patients experienced a significant drop in functional (p = 0.002) and the head and neck (p = 0.005) quality of life domains in the first 6 months whereas male patients experienced a significant drop in emotional QoL domains (p = 0.018) [Chart 2 of electronic supplementary material].
Patients aged between 25 and 50 years showed a drop in the social domain (p = 0.001) in the first 6 months whereas patients aged more than 50 years showed a drop in the physical domain (p = 0.001) which is statistically significant [Chart 3 of electronic supplementary material].
The study did not show any significant role of presence of any comorbidity on the quality of life of the patient [Chart 4 of electronic supplementary material].
Results showed a significant decrease in the quality of life in patients as the stage of the disease advanced. (p < 0.05) [Chart 5 of electronic supplementary material].
The site of primary disease played a role in altering the quality of life in head and neck cancer patients in which oral cavity cancer patients had the most significant dip in quality of life in functional and head and neck symptom domains (p < 0.05). Laryngeal cancer patients had the most significant debilitation in emotional domain (p = 0.01) [Chart 6 of electronic supplementary material].
The most debilitating modality of treatment was Surgery + CTRT which caused a significant drop in physical, emotional and head and neck symptoms domains (p < 0.05) in comparison to the other modalities which remained significant even after 1 year post treatment [Chart 7 of electronic supplementary material].
Discussion
A total of 130 patients with head and neck cancer were assessed. The demographic data showed that head and neck cancer is more common in the males (80%) between the age group of 35–50 years who are chronic tobacco chewers (45%) with the most common site of cancer being the oral cavity (61%). The data also showed that majority of the patients presented at Stage IV of their disease (35%).
In another study by D’Souza et al. [14], a total of 89 patients with HNC were assessed in which similarly, most (54%) of the participants belonged to the age group of 45–64 years, majority of the HNCs arised from oral cavity (40%) and were diagnosed in the advanced stage III (35%) and IV (35%). Majority (84%) of them had addictions, among which 62% of the participants had habits of smoking, 45% were chewing tobacco and 57% had alcoholism [14].
Another study by Terrel et al. [15] showed that a total of 570 patients with HNC were studied in which majority were male (78%) within the age group of 27–88 (mean 59 years) with habit of smoking (37%) and alcohol drinking (13%) with most common site of primary being larynx (30%) followed by oropharynx (29%) in which majority presented at stage IV disease (44%).
The fact that India is the second largest tobacco consumer in the world accounts for the majority of oral cavity cancers in our study. The discrepancy in results with other studies around the world could be due to this major factor.
Demographic Characteristics
Gender
Female patients experienced a significant drop in functional and the head and neck QoL domains in the first 6 months whereas male patients experienced a significant drop in emotional quality of life domains, in our study. This could possibly be owing to the psychological stress and pressure a male faces in a developing country like India to fulfil his daily wages and chores in order to sustain his household.
In contrast, in a study by Lo et al. [16], gender was not a significant determinant of QoL for HNC patients.
Onakoya et al. [17], similarly showed that there was no significant difference in the mean score between the genders for all the different domains.
Age
In our study, patients aged between 25 and 50 years showed a drop in the social domain in the first 6 months whereas patients aged more than 50 years showed a drop in the physical domain.
This could possibly be due to the social burdens that a youth faces in everyday life which gradually reduces with the increase in age. Along with that the inability to cope up and recover from the physical debilitating effects of cancer treatment could be the possible reason for the relatively low score of physical domain in elderly patients.
Lo et al. [16] showed that the treatment impact on all dimensions of QoL generally affected younger patients more as compared to older patients.
Onakoya et al. [17] showed that patients aged < 65 years old, when compared with those of > 65 years of age had lower mean scores in physical domain but higher in emotional domain.
Comorbidities
Our study did not show any significant role of presence of any comorbidity on the QoL of the patient.
In another study, 2 or more self-reported medical comorbid conditions predicted a moderate decrement in QoL scores. These decrements were noted more so in the physical domains than in the emotional or mental health domains [15].
Qol Curve
The largest HRQoL changes for head and neck cancer patients were seen within the first 3 months after commencement of treatment in our study. But even after 1 year post-treatment, none of the variables returned completely to the pre-treatment values.
In another study, results showed that HRQoL declines after treatment but recovers to baseline levels, generally within 12 months [18].
Another study by Brassio et al. showed that over the 12 months after completion of treatment, patients improved in most QoL dimensions and returned to pretreatment functioning in some. In no area, however, was patients’ functioning at 12 months clinically better than that before treatment [19].
D’Souza et al. [14], showed that there was maximum decrease in mean score of physical well-being as compared to other domains.
In contrast, our study showed that maximum decrease was seen in the head and neck possibly due to the debilitating effects of management for head and neck cancer which cause a significant impact on the various factors like swallowing, pain and voice.
Site of Primary Malignancy
Our study showed that oral cavity cancer patients have the most significant dip in quality of life in functional and head and neck symptom domains according to our questionnaire due to the debilitating and morbid conditions in swallowing and speech post-surgical resection along with the possibility of adjuvant radiotherapy and chemotherapy.
Laryngeal cancer patients have the most significant debilitation in emotional domains owing to the mental instability that comes along with the loss of voice post-laryngectomy and the presence of a permanent stoma postoperatively.
In a study done by Muller et al. [20], patients with laryngeal cancer had better eating scores and worse speech scores compared with other HNC sites, but otherwise had similar general health status.
In another study, Hammerlid et al. [21] showed similar results and they explained that the lower eating scores in the oropharynx, hypopharynx, or oral cavity cancer group may be related to dysphagia, which laryngeal cancer patients may not experience as much since patients with successful laryngeal preservation and even those after laryngectomy do not typically complain as much about dysphagia.
In another study by Chaturvedi et al., concerns and physical evaluation were compared between oral and laryngeal cancers and between preoperative and postoperative patients. Results showed that compared to laryngeal cancer patients, those with oral cancer significantly more often had concerns about current illness, subjective evaluation of health, eating and chewing, social interactions, pain and disfigurement (p < 0.05) [22].
Looking at the clinical characteristics of the oral cancer patients, Barrios et al., in their study, showed that combined therapy and advanced clinical stages of oral cancer adversely affected the HRQoL of patients. They also showed that oropharyngeal cancer patients had worse HRQoL than oral cancer patients [19]. This was owing to the fact that the patients with oropharyngeal malignancy were subjected to surgery and then postoperative adjuvant therapy whereas in contrast to their findings, at our institute, owing to the fact that patients with oropharyngeal malignancies are subjected primarily to chemotherapy and/or radiotherapy, they show a relatively better QoL as compared to patients with oral cavity and laryngeal malignancies.
Stage of the Disease
In our study, a significant decrease was seen in the QoL in patients as the stage of the disease advanced which is owing to the necessity of greater resection margins in surgery causing prolonged recovery time and the necessity of adjuvant therapy along with that.
Similarly, Hammerlid et al. [21] showed that the disease has a bigger effect on QoL in patients with advanced disease than on patients with small tumours.
Another study showed that composite QoL scores are significantly worse in advanced tumours than early stage tumours [23].
Similarly, in a study by Michael et al. [24], in which they studied the long term functional outcome of surgery with postoperative radiotherapy, inferior functional results were noted with increasing T stage which was statistically significant.
In contrast to our study, another study showed that cancer stage was not associated with any of the QoL scales. They justified this by stating that many of the patients with advanced cancers (stage III and IV) are treated with surgery-sparing, chemoradiation protocols, which may potentially preserve function and QoL. In addition, they also stated that QoL decrements that one may expect with more advanced cancer stages may be, to a great degree, related to cancer treatment and number of treatment modalities rather than cancer stage, thereby making stage a less significant predictor of QoL [15].
Treatment Modality
The most debilitating modality of treatment was Surgery + CTRT which caused a significant drop in physical, emotional and head and neck symptom domains in comparison to the other modalities which remained significant even after 1 year post treatment.
Similarly, Fang et al. [25] showed that in their study, some individuals with HNC, after receiving postoperative radiotherapy, suffered from a deterioration of QoL scales, especially in head and neck symptoms.
Our study did not show any significant difference in the quality of life in patients undergoing chemoradiotherapy as compared to radiotherapy alone, henceforth questioning the role of the toxicity of chemotherapy in the QoL of the patient.
In contrast, another study by Klein et al. [18] depicted that combined chemoradiotherapy showed a trend toward worse HRQoL compared with Radiotherapy alone.
Conclusion
The study findings suggest that the treatment and intervention protocol for head and neck cancer patients should not only be focused on survival but also on ensuring QoL throughout the management intervention and stages of recovery. Support and care should not only be provided for the prevention of complications and further progression of the disease but also to facilitate management of pain, psychosocial instability and towards prevention of the debilitating loss of function after treatment interventions.
Along with this, doctors should consider the impact of management interventions on QoL when considering and discussing about treatment option with HNC patients. Detailed assessment of the various factors which hamper the quality of life in head and neck cancer patients should be entitled which can henceforth provide quality care, a completely new view into the health care experience and improving patient satisfaction.
References
de Melo Filho MR, Rocha BA et al (2013) Quality of life of patients with head and neck cancer. Braz J Otorhinolaryngol 79(1):82–88
Connor NP, Cohen SB, Kammer RE et al (2006) Impact of conventional radiotherapy on health-related quality of life and critical functions of the head and neck. Int J Radiat Oncol Biol Phys 65(4):1051–1062
Bottomley A (2002) The cancer patient and quality of life. Oncologist 7(2):120–125
Gotay CC (1996) Trial-related quality of life: using quality-of-life assessment to distinguish among cancer therapies. J Natl Cancer Inst Monogr 20:1–16
Martino R, Ringash J (2008) Evaluation of quality of life and organ function in head and neck squamous cell carcinoma. Hematol Oncol Clin North Am 22(6):1239–1256
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C et al (2017) Global, Regional, and National Cancer Incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 Cancer Groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol 3:524
Sankaranarayanan R, Masuyer E, Swaminathan R, Ferlay J, Whelan S (1998) Head and neck cancer: a global perspective on epidemiology and prognosis. Anticancer Res 18:4779–4786
Kekatpure VD et al (2012) Head and neck cancer in India: Need to formulate uniform national treatment guideline? Indian Journal of Cancer 49(1):6–10
de Alvarenga LM, Ruiz MT, Pavarino-Bertelli EC, Ruback MJC, Maniglia JV, Goloni-Bertollo EM (2008) Epidemiologic evaluation of head and neck patients in a university hospital of Northwestern São Paulo State. Braz J Otorhinolaryngol 74(1):68–73
Stoeckli SJ, Guidicelli M, Schneider A, Huber A, Schmid S (2001) Quality of life after treatment for early laryngeal carcinoma. Eur Arch Otorhinolaryngol 258(2):96–99
Ojo B (1992) A systematic review of head and neck cancer quality of life assessment instruments. Oral Oncol 48(10):923–993
De Graeff A, de Leeuw JR, Ros WJ, Hordijk GJ, Blijham GH, Winnubst JA (2000) Pretreatment factors predicting quality of life after treatment for head and neck cancer. Head Neck 22(4):398–407
Bjordal K, Kaasa S (1995) Psychological distress in head and neck cancer patients 7–11 years after curative treatment. Br J Cancer 71:592–597
D’Souza PJJ et al (2013) Quality of life of head and neck cancer patients receiving cancer specific treatments. JKIMSU 2(1):51–57
Terrel JE et al (2004) Clinical predictors of quality of life in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 130(4):401–408. https://doi.org/10.1001/archotol.130.4.401117
Lo PSY et al (2004) Quality of life measurement in patients undergoin radiation therapy for head and neck cancer: a Hong Kong experience. J Oncol Manag 13(23):1–9
Onakoya PA et al (2006) Quality of life in patients with head and neck cancers. J Natl Med Assoc 98(5):765–770
Klein J et al (2014) Health related quality of life in head and neck cancer treated with radiation therapy with or without chemotherapy: a systematic review. Oral Oncol 50(4):254–262
Barrios R, Glacia Medina B, Tsasakos G et al (2015) Oral and general health related quality of life in patients treated for oral cancer compared to control group. Health Qual Life Outcomes 13(9):1–8
Muller R, Paneff J, Kollner V, Koch R (2001) Quality of life of patients with laryngeal carcinoma: a post-treatment study. Eur Arch Otorhinolaryngol 258:276–280
Hammerlid E, Taft C et al (2001) Health-related quality of life in long-term head and neck cancer survivors: a comparison with general population norms. Br J Cancer 84:149–156
Chaturvedi SK, Shenoy A, Prasad KM et al (1996) Concerns, coping and quality of life in head and neck cancer patients. Support Care Cancer 4(3):186–190
Vartarian JG, Carvalha AL, Yueh B et al (2004) Longterm quality of life evaluation after head and neck cancer treatment in a developing country. Arch Otolaryngol Head Neck Surg 130:1209–1213
Michael MD, Zelefsky J, Gaynor J (1996) Long term subjective functional outcome of surgery plus postoperative radiotherapy for advanced stage oral cavity and oropharyngeal carcinoma. Am J Surg 171(2):258–262
Fang FM, Chien CY, Kuo SC et al (2004) Changes of quality of life of head and neck cancer patients following postoperative radiotherapy. Acta Oncol 43:571–578
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yojana Sharma and Girish Mishra should be considered joint first author.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharma, Y., Mishra, G. & Parikh, V. Quality of Life in Head and Neck Cancer Patients. Indian J Otolaryngol Head Neck Surg 71 (Suppl 1), 927–932 (2019). https://doi.org/10.1007/s12070-019-01620-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-019-01620-2