Abstract
We studied the ethmoidal arteries using preexisting computer tomography of the paranasal sinuses (CT PNS) and statistically scrutinized data obtained between genders. A descriptive study from 77 CT PNS dated January 2016–December 2016 were collected and reviewed by two radiologists. A total of 54 (108 sides) CT PNS were studied of patients aged 18–77 years. 37 are male, 17 are female; with Bumiputera Sarawak predominance of 25 patients, 12 Malays, 16 Chinese and one Indian. Rate of identification are as follows: anterior ethmoidal artery (AEA)-100%, middle ethmoidal artery (MEA)-30%, posterior ethmoidal artery (PEA)-86%. The average distance from AEA–MEA is 8.1 ± 1.52 mm, MEA–PEA is 5.5 ± 1.29 mm and AEA–PEA is 12.9 ± 1.27 mm. The mean distance from PEA-the anterior wall of sphenoid is 7.7 ± 3.96 mm, and PEA-optic canal is 8.5 ± 3.1 mm with no statistical difference when compared between gender. AEA frequently presented with a long mesentery 57.4%, while 87.1% of PEA was hidden in a bony canal. The vertical distance of the AEA-skull base ranges from 0 to 12.5 mm whilst PEA-skull base is 0–4.7 mm. There is no statistical difference in distances of AEA, MEA nor PEA to skull base when analyzed between genders; t(82) = 1.663, p > 0.05, t(32) = 0.403, p > 0.05 and t(75) = 1.333, p > 0.05 respectively. We newly discovered, that 50% of MEA is hidden in a bony canal, and its distance to skull base ranged 0–5.3 mm. MEA and PEA less commonly have a short or long mesentery. Knowledge on the ethmoidal arteries especially in our unstudied population of diverse ethnicity, gains to assist surgeons worldwide, when embarking in endoscopic transnasal surgeries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Caldwell [1] first described radiology of the paranasal sinuses (PNS) in the 1900s. Since then, CT PNS (Computer tomography of paranasal sinuses) has aided clinicians and surgeons alike in establishing diagnosis and treatment. The ethmoidal arteries which arise from the ophthalmic arteries, are important anatomical landmarks in endoscopic transnasal surgeries to critical structures such as the optic nerve and skull base [2]. However, the middle ethmoidal artery (MEA) has not been well studied. We set out to study the ethmoidal arteries amongst our multi-diverse ethnic population, attempting to identify any differences from Caucasian data. We also analyzed the data, to see if any differences existed when comparing a male to a female patient. We aim to correlate radiological features to assist surgeons, when planning for endoscopic transnasal surgeries and ultimately reduce perioperative complications.
Methodology
Study Design and Method
Approval from Malaysia Research Ethics Committee (MREC) was obtained and the study registered with NMRR Research ID 32016.
A retrospective descriptive study of CT PNS of patients from January 2016–December 2016 were collected and analyzed. CT films were traced manually and loaded into Osirix system. The CT films were done using SOMATOTOM Sensation Cardiac 64 (Siemens) with a collimator of 0.75 mm, 120 kV, mAS 100–150 and FOV 123 mm. Subject inclusion criteria are well formed paranasal sinuses, no history of previous sinus surgery and age above 18 years at the time the imaging was done. Films with previous history of facial trauma, incomplete or inadequate quality films, underdeveloped paranasal sinuses and extensive sinusitis, were excluded from the study for more accurate data collection. The films were reconstructed into 2D Orthogonal image and reviewed by two qualified radiologists separately. Where discrepancies occurred, the two radiologists would again review the films, to come to an agreement.
Radiologic Parameters
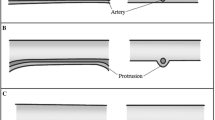
Samples were analyzed for presence of anterior ethmoidal artery (AEA), posterior ethmoidal artery (PEA) followed by middle ethmoidal artery (MEA) using axial scans, then confirmed with sagittal and coronal view (Fig. 1). Once identified, the distances between the arteries and their distances to skull base were measured on a sagittal plane. The distance of PEA to anterior wall of sphenoid and optic canal were measured in a tangential plane, using sagittal view (Fig. 2). The presentation of the arteries whether in a bony canal, a short mesentery or long mesentery were documented and their vertical distance to skull base were measured where possible (Fig. 3). The presentation of artery in a bony canal is defined as running through the skull base bone, a short mesentery is taken as vertical distance less than 1 mm to skull base, where as a long mesentery is calculated as more than 1 mm distance to skull base [2].
Data and Statistical Analysis
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (Version 22) using descriptive statistics. T-test was used to identify any significant differences in distances between AEA to PEA, PEA to anterior wall of sphenoid, PEA to optic canal amongst males versus females. T-test was also used to examine the distances of ethmoidal arteries to skull base, when compared between genders. A p value of less than 0.05, is taken as statistically significant.
Results
A sum of 54 patients totaling 108 samples, consisting of 37 males and 17 females aged between 18 and 77 years old were studied. The majority are Bumiputera Sarawak 25 subjects, 12 Malays, 16 Chinese and one Indian. The AEA was identified in 100% of all sides, MEA found in 30% and the PEA was seen in 86% of all scans.
The range of distances from AEA to MEA is 4.4–11.2 mm, MEA to PEA 3.3–8.8 mm, with a mean distance of AEA to PEA measuring 7.7–17.9 mm, PEA to anterior wall of sphenoid 0–18.7 mm and PEA to optic canal 1–19 mm. The average distance from AEA to MEA is 8.1 ± 1.52 mm, MEA to PEA is 5.5 ± 1.29 mm and AEA to PEA is 12.9 ± 1.27 mm. The mean distance from PEA to the anterior wall of sphenoid is 7.7 ± 3.96 mm, and PEA to optic canal is 8.5 ± 3.1 mm.
Using Independent Sample T-test we found, the distances between AEA to PEA comparing males versus females have no obvious difference, t(85) = 1.415, p > 0.05. There was no statistical difference between the distance of PEA to anterior wall of sphenoid, nor the distance of PEA to optic canal when analyzed between males and females, t(84) = 1.837, p > 0.05 and t(84) = 0.259, p > 0.05 respectively. Distances of AEA, MEA and PEA to skull base between genders, have no statistical difference; t(82) = 1.663, p > 0.05, t(32) = 0.403, p > 0.05 and t(75) = 1.333, p > 0.05 accordingly.
The AEA frequently presented with a long mesentery 57.4%, short mesentery 22.2% and found in a bony canal in 20.4%. The MEA is more commonly seen in a bony canal 50%, had a short mesentery in 38.2% while 11.8% had a long mesentery. A majority of PEA was hidden in a bony canal 87.1%, had a short mesentery in 9.7% and long mesentery in 3.2%. The vertical distance of the AEA to the skull base ranges from 0 to 12.5 mm, MEA to the skull base is 0–5.3 mm, whilst PEA to the skull base 0–4.7 mm.
Discussion
Computer Tomography is the gold standard for evaluation of the paranasal sinuses and are mandatory prior to embarking on any endoscopic or transnasal sinus surgery [3]. It is a vital guide in identification of the ethmoidal arteries, which in turn acts as an anatomical landmark intraoperatively. In succession, the surgeon is thus able to steer clear of danger zones, and ultimately reduce postoperative complications.
We found AEA to be the most consistently identifiable artery, which is seen in all 108 images studied. Vatanasapt et al. and Ferrari et al. also reported a 100% rate of AEA detection on CT scan [4, 5]. Other authors recorded a 92–95% rate of AEA identification (Table 1) [4,5,6,7]. We demarcated MEA in 31% of all images. Similarly, MEA was reported at a frequency of 28.6–36% in other studies (Table 1) [4, 8]. We detected PEA in 81% of our images. Other studies, showed a wide range from 35 to 100% identification of PEA in CT scan (Table 1) [4,5,6,7].
The average distance of AEA to MEA is 8.1 ± 1.52 mm and MEA to PEA is 5.5 ± 1.29 mm. Mason et al. [8] reported the mean distance from AEA to MEA and MEA to PEA are both 11.3 mm (Table 2). We postulate, there may be a difference in anatomy comparing Asian (Malaysian) versus Caucasian population, or perhaps a difference in methodology in obtaining these measurements. However, we found the average distance from AEA to PEA to be 12.9 ± 1.27 mm, which correlates with several other studies done in Spanish, Turkish and Thailand population whose results ranged from 11.24 to 13.7 mm (Table 2) [4, 6, 7]. The mean distance from PEA to the anterior wall of sphenoid is 7.7 ± 3.96 mm. Han et al. [7] reported almost similar findings of 8.1 mm, but Vatanasapt et al. [4] had inconsistent readings ranging 0–18 mm. The average distance from PEA to optic canal is 8.5 ± 3.1 mm. Other authors reported distances ranging from 6.4 to 8.5 mm (Table 2) [4, 6, 7].
Previous texts describe three variations of presentation of AEA [2, 10]. In our study, the majority of AEA 57.4% had a long mesentery. Ko et al. [2] reported 50.5% of AEA having a long mesentery, 33.7% with a short mesentery and remaining 16% hidden in a bony canal. Contrary to this, Basak et al. [11] and Moon et al. [12] reported the majority of AEA 57% and 90% respectively, was hidden in a bony canal. When AEA is exposed as a long mesentery, it puts it at higher risk to be injured during drilling of the skull base. Accidental injuries of the lamella of the cribiform plate and the AEA are the main potential risks during endoscopic surgery, and may cause disastrous consequences [13, 14].
In our series, 50% of MEA is hidden in a bony canal. A short mesentery is seen in 38.2% of MEA while the remaining 11.8% has a long mesentery. Takahashi et al. reported an accessory ethmoidal foramina in 33.3% of their study subjects [15], while Mason et al. demonstrated 26% MEA in their series [8]. In these papers, the existence of MEA has been inferred by the presence of a bony foramina [8, 15]. We identified PEA predominantly in a bony canal 87.1%, while 9.7% had a short mesentery and 3.2% with a long mesentery. This raises a point of interest, as to the authors knowledge, no study has mentioned the possibility of MEA nor PEA presenting with a short or long mesentery. In terms of endoscopic transnasal surgery, the longer the mesentery, the more prone it is, for the artery to be injured. Once injured, it may retract deep into its bony foramina, making it difficult to achieve hemostasis. When hidden in a bony canal, this gives the surgeon some direction, to know that a sufficient amount of drilling is required before reaching the artery.
The vertical distance of the AEA to the skull base ranges from 0 to 12.5 mm. Ko et al. [2] reported the mean distance of AEA to skull base is 0–22.6 mm. We found the distance from MEA to skull base ranged from 0 to 5.3 mm, whilst PEA to the skull base is 0–4.7 mm. We discovered that, the anatomy between men and women was not affected, when comparing distances of ethmoidal arteries to essential structures such as the optic canal and skull base.
Radiological Perspective
We found the ethmoidal arteries more easily identifiable on the axial view. This coincides with findings by Cankal in 2004 where he reported 92% identification of AEA on axial scans, versus 84% identification on coronal scans from the same sample pool [6]. In 2006, Takahashi concluded that thin-section axial images using multidetector row CT are useful in identification of AEA, whilst coronal multiplanar reconstruction images at a section of 1 mm depicted AEA [15]. Ko et al. clearly demarcated 140 images of AEA out of 157 samples using the coronal view, versus 119 identified on a sagittal plane [2]. However, a study by Souza et al. in 2009, purely employed the use of coronal CT scans for identification of AEA [16]. Mason et al. also felt coronal cuts to be most conducive in identifying the middle ethmoidal foramina [8].
The sagittal plane, secondarily aided with an axial view, is best used for any form of measurements (distances of the arteries from each other and from important structures). This is supported by studies done by Canovas et al [7].
In addition, we gained the assistance of two certified and qualified radiologists in this study, to test the reproducibility of the methodology of our study. We found consistent results between the two experts. This ensures that our results are more reliable, and allows reduced biasness in data collection.
Conclusion
Detailed Computer tomographic study of the ethmoidal arteries aid surgeons in endoscopic nasal and skull base surgeries, by assisting in planning the approach of surgery, avoid complications from injury to neurovascular and other important structures, as well as serve as important anatomical landmarks to the skull base, anterior wall of sphenoid and optic canal. The axial cut is the best view for identification of all three ethmoidal arteries, while the sagittal plane allows measurement of distances to important structures. There exists a tertiary (Middle Ethmoidal Artery) in one third of subjects, predominantly found in a bony canal (50%), which puts it at lower risk of injury, during endoscopic transnasal surgery. The MEA and PEA to a lesser extent, presents with a short or long mesentery. Our results differ from the Caucasian data. We infer that the anatomy of Caucasians may differ from Asians, or the technique used for acquiring data may be different. It is good, for the operating surgeon to bear in mind this anatomical difference, when dealing with a patient from a different country. Comparison of distances of all three ethmoidal arteries to the skull base between genders, yielded no difference. There is also no significant difference in distances between arteries, PEA to anterior wall of sphenoid nor PEA to optic canal when comparing men to women. This leads us to conclude that operating in a female or male patient is the same, in terms of distances to important structures. An indepth knowledge of the ethmoidal arterial system in the nasal cavity, allows prevention of unwanted complications and is clinically relevant.
References
Thombury JR, Caldwell EW (1994) Clinical efficacy of diagnostic imaging: love it or leave it. AJR Am J Roentgenol 162(1):1–8
Ko YB, Kim MG, Jung YG (2014) The anatomical relationship between the anterior ethmoid artery, frontal sinus, and intervening air cells; can the artery be useful landmark? Korean J Otorhinolaryngol-Head Neck Surg 57(10):687–691
Cashman EC, MacMahon PJ, Smyth D (2011) Computed tomography scans of paranasal sinuses before functional endoscopic sinus surgery. World J Radiol 3(8):199–244
Vatanasapt P, Thanaviratananich S, Chaisiwamongkol K (2012) Landmark of ethmoid arteries in adult Thai cadavers: application for sinus surgery. J Med Assoc Thai 95(Suppl):153–156
Ferrari M, Pianta L, Borghesi A, Schreiber A, Ravanelli M, Mattavelli D et al (2017) The ethmoidal arteries: a cadaveric study based on cone beam computed tomography and endoscopic dissection. Surg Radiol Anat. https://doi.org/10.1007/s00276-017-1839-6
Cankal F, Apaydin N, Acar HI, Elhan A, Tekdemir I, Yurdakul M et al (2004) Evaluation of the anterior and posterior ethmoidal canal by computed tomography. Clin Radiol 59:1034–1040
Canovas et al (2011) Radiological anatomy of the ethmoidal arteries: CT cadaver study. Acta Otorrinolaringol Esp 62(5):367–374
Mason E, Solares CA, Carrau RL, Figueroa R (2015) Computer tomographic exploration of the middle ethmoidal artery. J Neurol Surg B 76:372–378
Han JK, Becker SS, Sr Bomeli, Gross CW (2008) Endoscopie localization of the anterior and posterior ethmoid arteries. Ann Otol Rhinol Laryngol 117(12):931–935
Stammberger H (1991) Functional endoscopic sinus surgery: The Messerklinger technique. BC Decker, Philadelphia
Basak S, Cz Karaman, Akdilli A, Mutlu C, Odabasi O, Erpek G (1998) Evaluation of some important anatomical variations and dangerous areas of the paranasal sinuses by CT for safer endonasal surgery. Rhinology 36(4):162–167
Moon HJ, Kim Hu, Lee JG, Chung IH, Yoon JH (2001) Surgical anatomy of the anterior ethmoidal canal in ethmoid roof. Laryngoscope 111(5):900–904
Ohnishi T, Yanagisawa E (1994) Endoscopic anatomy of the anterior ethmoidal artery. Ear Nose Throat J 73(9):634–636
Grevers G (2001) Anterior skull base trauma during endoscopic sinus surgery for nasal polyposis preferred sites for iatrogenic injuries. Rhinology 39(1):1–4
Takahashi Y, Kakizaki H, Nakano T (2011) Accessory ethmoidal foramina: an anatomical study. Ophthal Plast Reconstr Surg 27(2):125–127
Souza SA, Souza MMA, Gregorio LC, Ajzen S (2009) Anterior ethmoidal artery evaluation on Coronal CT Scans. Braz J Otorhinolaryngol 75(1):101–106
Funding
This research is a self-initiated study and has not received any funding from any source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Authors J has completed this research as part of her fulfillment in obtaining her Masters degree in Otolaryngology. All other authors declare no conflicts of interest pertaining to this study.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors. Approval from Malaysia Research Ethics Committee (MREC) was obtained prior to the study, and the study registered with NMRR Research ID 32016.
Informed Consent
There are no identifying information used in this article as human participants are not involved in this study.
Rights and permissions
About this article
Cite this article
Kho, J.P.Y., Tang, I.P., Tan, K.S. et al. Radiological Study of the Ethmoidal Arteries in the Nasal Cavity and Its Pertinence to the Endoscopic Surgeon. Indian J Otolaryngol Head Neck Surg 71 (Suppl 3), 1994–1999 (2019). https://doi.org/10.1007/s12070-018-1415-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1415-3