Abstract
The aim of this analytical study was to assess the reduction in intra- and post-operative complications of parotid surgeries for benign lesions following simple surgical steps and to compare the outcome with the literature. A retrospective study of 77 patients requiring parotidectomy surgery for benign parotid lesions was conducted in Department of Otorhinolaryngology, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun from the period of January 2011 to January 2016. Patients were followed up for 1–5 years and serial evaluation was done for all cases who developed any of intra- or post-operative complications in their disease course. The ages of presentation varied from 1.5 to 70 years. There were 51 males and 26 female patients. Majority cases were of pleomorphic adenoma followed by warthins tumor. Superficial parotidectomy was done in 69 patients; 4 cases required near total parotidectomy while total conservative parotidectomy was done in 4 cases. The commonest complication was altered sensations around the ear which was seen in 10 cases followed by temporary facial nerve paresis and sialocele formation which occurred in 3 cases each. This study advocates the importance of detailed anatomical knowledge, behavior of various benign pathologies, experience of surgeon and his fine dissection techniques to ensure minimum risks of injury to important structures in surgical field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign swellings of the parotid gland may arise due to congenital anomalies and lympho-venous cystic lesions, trauma, acute and chronic infectious processes, sialoadenosis, salivary calculi and benign tumors. Surgical intervention is often possible and required in majority of these lesions. Parotid surgery is often associated with some worrisome complications such as facial palsy (transient/permanent), sensory disturbances, Frey’s syndrome, recurrence and disfigurement. Hence apart from disease clearance, aesthetic outcome, patient’s satisfaction and preservation of normal function takes on more importance while performing parotidectomy surgery. Surgical considerations with respect to various benign lesions of parotid gland are usually dictated by the skill, experience and preferences of surgeon; histological nature of lesion; location, extent and size of lesion and patient’s perspectives.
We present a comprehensive review of 77 cases requiring parotidectomy surgery for benign parotid lesions. The purpose of this analytical study was to assess the reduction in intra- and post-operative complications of parotid surgeries for benign lesions following simple surgical steps and to compare the outcome with the literature.
Materials and methods
A retrospective study of 77 patients requiring parotidectomy surgery for benign parotid lesions was conducted in Department of Otorhinolaryngology, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun from the period of January 2011 to January 2016. Details of history as regards to onset of symptoms, duration of disease and previous history of any surgery or other forms of treatment were noted with special note to personal habits like smoking and alcohol consumption. After thorough physical examination patients underwent Fine needle aspiration cytology, tumor localization was done by means of ultrasound of face and neck along with CECT/MRI of head and neck region. Majority of patients had a superficial lobe involvement. Pre operative Facial nerve evaluation was done and documented following House–Brackmann grading system. All patients had a normal facial nerve function pre-surgery. Parotidectomy was performed in all patients as per the extent of involvement of the gland. Under mentioned perioperative techniques were adopted to avoid complications in all cases. 69 cases underwent superficial parotidectomy, 4 cases required near total parotidectomy while 4 cases underwent total conservative parotidectomy for deep lobe tumor. Follow up period ranged from 1 year to maximum of 5 years 8 months.
Results
The histopathological details of 77 cases are tabulated in Table 1. The ages of presentation varied from 1.5 to 70 years. There were 51 males and 26 female patients. Majority cases were of pleomorphic adenoma followed by warthins tumor.
There was involvement of superficial lobe of parotid in 69 patients; they were thus treated by superficial parotidectomy. Whereas 2 cases of parotid abscess, 1 lymphangioma patient and one case of first branchial cleft anomaly required near total parotidectomy due to partial involvement of deep lobe. Total conservative parotidectomy was done in 4 cases of pleomorphic adenoma where almost whole of deep lobe was tumorous (Fig. 1).
Various per operative parotidectomy pictures showing a type II first branchial cleft anomaly with tract (short black arrow) passing in between the branches of facial nerve (long black arrow), also seen is the duplication of cartilaginous part of external auditory canal (white arrow), b a case of lymphangioma of parotid gland where whole of superficial and part of deep lobe was lymphangiomatous, c pleomorphic adenoma involving whole of superficial lobe of parotid with tumor adherent to main trunk of facial nerve and its branches(black arrow), d picture depicting various subdivisions of facial nerve following total conservative parotidectomy for pleomorphic adenoma
Early and late postoperative complications were assessed and tabulated (Table 2).
The commonest complication was altered sensations around the ear which was seen in 10 cases, although this was a temporary problem which resolved by itself within 4 weeks to 8 months of surgery. Temporary facial nerve paresis was seen in 3 cases, of which two cases were of type II first branchial cleft anomaly where the tract was going in close relation to facial nerve and thus had to be separated from the same. The third case was of chronic sialadenitis where there was an extensive fibrosis and granulations thus again requiring lot of manipulations around the nerve. All these cases showed improvement in 4–6 weeks following surgery with complete resolution within 6 months. Sialocele formation occurred in 3 cases of superficial parotidectomy. They were managed by aspiration and pressure dressing and resolved within 2–4 weeks. One case suffering from diabetes mellitus had minimal distal end flap necrosis for which local debridement was done. One patient had hypertrophic scar and none had Frey’s syndrome. All patients were called for follow-up at weekly interval for initial month following surgery, thereby once a month for another 6 months and then once in 3 months. All cases are maintaining regular follow-up. None of the patients have developed any permanent complications or recurrence of disease till date.
The perioperative techniques adopted by us to avoid complications are as follows:
- 1.
The knowledge of anatomy of this area is of utmost importance while performing parotidectomy surgery as the aim of surgery is not only to remove the disease but to achieve normal facial functions. Thus surgeon should be well versed with the anatomy and relations of parotid gland, facial nerve and surrounding structures.
- 2.
Informed consent: it is important to explain about the surgical procedure and outcome to the patient. The probable complications should also be explained to the patient and concerned relatives.
- 3.
Anesthesia: We perform surgery under general anesthesia. Paralytics are used while induction thereby their use is avoided. This helps in intraoperative monitoring of facial nerve.
- 4.
Incision and flap raising: a modified Blair incision is used. It is important to remember that while giving incision an adequate cuff of tissue should be present around the ear lobule; this will prevent pixie-ear deformity. Another point to be remembered while planning the incision is that the tapering of postauricular skin flap should be avoided; else skin flap necrosis occurs post operatively. While raising flaps over the gland superficial musculoaponeurotic system (SMAS) should be included in the flap, except in the cases where tumor is very superficial; in such cases the dissection should be subcutaneous to avoid any inadvertent tumor entry. Wherever feasible in superficial tumors we raise a superficial skin flap to avoid tumor entry and then under direct visualization raise the SMAS flap in anteroposterior direction; a stay suture is given to the SMAS flap which is later utilized at end of tumor surgery during closure (Fig. 2a, b). The advantage of sub-SMAS flap is that it reduces the incidence of postoperative Frey’s syndrome and development of divot defect after gland removal. The flap at the anterior end of the gland should be raised cautiously with a blunt dissector to avoid injury to the distal branches of facial nerve emerging from the gland. Similarly while raising the posterior flaps the posterior branch of greater auricular nerve should be preserved whenever possible. This will cause a lesser area of sensory deficit to the earlobe. During surgery the flap should be covered with warm saline soaked gauges, this will maintain the vascularity of flap and prevents the chances of post operative distal flap necrosis.
Fig. 2 a per-operative picture of superficial parotidectomy being performed for a very superficial parotid tumor depicting an antero-posteriorly raised SMAS flap (black arrow), b showing the SMAS flap sutured back in place before skin closure to avoid Frey’s syndrome and divots defect, c depicting posterior belly of diagastric muscle(thin black arrow) as landmark for main trunk of facial nerve (bold black arrow); nerve lies approximately 1 cm above and parallel to the upper border of the digastric muscle, b relationship between facial nerve (bold black arrow) and stylomastoid artery (thin black arrow) which usually lies just above the main trunk of facial nerve
- 5.
Identification of facial nerve and dissection of gland: identification of facial nerve is of utmost importance in parotid surgery. Although many landmarks have been mentioned in the literature for identification of main trunk of facial nerve, but in our experience posterior belly of digastric is the most reliable landmark (Fig. 2c); the nerve trunk lies approximately 1 cm above and parallel to the upper border of the digastric muscle near its insertion at the mastoid tip. Another useful landmark that we rely upon in routine cases is stylomastoid artery; this artery usually lies just above the main trunk of facial nerve (Fig. 2d). However we have seen that in cases of large tumors, tumors involving the posterior part of gland, inflamed gland, and excessive post inflammatory fibrosis, it becomes difficult to identify the main trunk. In such conditions a retrograde dissection of nerve is done tracing the peripheral branches to main trunk. We commonly use buccal branch of facial nerve for retrograde dissection; the reason being that it is easily identifiable. Buccal branch lies 1 cm above and parallel to the parotid duct, which acts as surgical landmark for this branch. The other landmarks can be retromandibular vein for marginal mandibularis, zygomatic arch for zygomatic branch of facial nerve. Nerve stimulator can also be used for identification of facial nerve. However in our opinion excessive stimulation of nerve with nerve stimulator should be avoided as it can cause temporary paresis of facial nerve. Once the nerve is identified careful dissection is carried out in faciovenous plane of patey, which is a surgical plane artificially dividing the parotid gland into superficial and deep lobe. While dissection we use bipolar cautery or harmonic scalpel to deal with small vessels in close relation to the nerve. Extent of removal of gland depends upon the type of parotidectomy being performed. In cases of near total or total parotidectomy gentle handling of facial nerve and its branching should be done.
- 6.
Parotid duct: whenever feasible we try to preserve parotid duct during superficial parotidectomy. In our experience it reduces the chances of sialocele as the saliva from parotid remnant is drained out through this duct.
- 7.
A suction drain and pressure dressing is kept for 48 h to prevent collection and antibiotic coverage is given for 5 days.
Discussion
The commonest indication for parotidectomy is the neoplasms of parotid gland. Tumors arising in parotid gland are relatively rare comprising between 2 and 6.5% of all head and neck tumors [10] and of them 80% are benign. The other benign conditions requiring parotidectomy are First Branchial Cleft Anomaly presenting as cyst or sinus in relation to parotid gland. Inflammatory diseases like chronic parotitis, deep salivary calculi and parotid abscess are occasionally treated with total parotidectomy, with recognition that surgery in an inflamed gland probably carries a higher risk of postoperative facial nerve dysfunction [11]. In our series also the commonest indication for parotidectomy was pleomorphic adenoma followed by warthins tumor and chronic sialadenitis.
Various types of parotid surgeries have been mentioned in the literature for benign parotid lesions namely superficial parotidectomy, near total parotidectomy and total conservative parotidectomy. Apart from these various limited procedures have been tried like extracapsular dissection, partial superficial parotidectomy [5]. In our series majority of patients underwent superficial parotidectomy whereas few cases required near total and total conservative parotidectomy. Instead of going for limited procedures we performed formal parotidectomy in all cases of pleomorphic adenoma in view of the fact that conservative superficial or deep lobe parotidectomy leads to decreased risk of recurrences [12]. The reasons for recurrences in benign epithelial tumors are intraoperative neoplastic cell spreading, multicentricity of tumor and tumor pseudopodia. Thus it is important to perform an adequate surgical clearance to prevent recurrences.
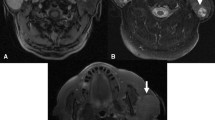
Most dreadful complication of parotid surgery is facial nerve injury. Incidence of facial nerve paresis ranges from 13 to 100% depending upon the underlying pathology, extent of operation, location of tumor and revision surgery [13]. However the rate of permanent paralysis is below 5% with most of recoveries occurring within 12 months [13, 14]. In our series temporary facial nerve paresis was seen in 3.9% of cases with complete resolution within 6 months. None of the cases developed permanent facial nerve palsy. The other common complication described in the literature is Frey’s syndrome or gustatory sweating. About 14–43% patients are symptomatic and less than 10% patients suffer from severe gustatory sweating [9]. It was seen in none of the cases in our series. Commonest temporary complication in our series was altered sensations around the ear which resolved within 8 months in all cases. Thus we can say that by the use of above mentioned peri-operative techniques we can reduce the rate of complications to bare minimal (Fig. 3).
Postoperative pictures of patients, a depicting left facial nerve paresis in a child operated for type II first branchial cleft anomaly, b shows complete recovery of facial nerve paresis in same child 3 months following surgery, c, d picture post right superficial parotidectomy, facial symmetry is well maintained with minimally visible scar mark 6 months post surgery, e early postoperative picture of a child who underwent near total parotidectomy for lymphangioma parotid gland, f same child the incision had to be modified for complete removal of tumor as apart from parotid gland the neck was also involved
Conclusion
The aim of parotidectomy surgery is complete removal of disease without any major complications. This can be best achieved by thorough knowledge of the anatomy of the region and use of meticulous surgical technique.
References
Guntinas-Lichius O, Kick C, Klussmann JP, Jungehuelsing M, Stennert E (2004) Pleormorphic adenoma of parotid gland : a 13 years experience of consequent management by lateral or total parotidectomy. Eur Arch Otorhinolaryngol 261:143–146
Witt RL (2009) Incidence and management of sialocele after parotidectomy. Otolaryngol Head Neck Surg 140(6):871–874
Wax M, Tarshis L (1991) Post-parotidectomy fistula. J Otolaryngol 20:10–13
Marchese-Ragona R, De Filippis C, Marioni G, Staffieri A (2005) Treatment of complications of parotid gland surgery. Acta Otorhinolaryngol Ital 25(3):174–178
Ciuman RR, Oels W, Jaussi R, Dost P (2012) Outcome, general, and symptom-specific quality of life after various types of parotid resection. Laryngoscope 122:1254–1261
Arriaga MA, Myers EN (1990) The surgical management of chronic parotitis. Laryngoscope 100(12):1270–1275
Redaelli de Zinis LO, Piccioni M, Antonelli AR, Nicolai P (2008) Management and prognostic factors of recurrent pleomorphic adenoma of the parotid gland: personal experience and review of the literature. Eur Arch Otorhinolaryngol 265(4):447–452
Greenhill GA, O’Regan B (2009) Incidence of hypertrophic and keloid scars after N-butyl 2-cyanoacrylate tissue adhesive had been used to close parotidectomy wounds: a prospective study of 100 consecutive patients. Br J Oral Maxillofac Surg 47(4):290–293
Linder TE, Huber A, Schmid S (1997) Frey’s syndrome after parotidectomy: a retrospective and prospective analysis. Laryngoscope 107:1496–1501
Parkin DM, Whelan SL, Feray J (1997) Cancer incidence in five continents, vol VII. IARC Scientific Publication No. 143. Lyon International Agency for Research on Cancer
Motamed M, Laugharne D, Bradley PJ (2003) Management of chronic parotitis: a review. J Laryngol Otol 117(7):521–526
Ungari C, Paparo F, Colangeli W, Iannetti G (2008) Parotid glands tumors: overview of a 10 years experience with 282 patients, focusing o 231 benign epithelial neoplasms. Eur Rev Med Pharmacol Sci 12:321–325
Bron LP, O’Brien CJ (1997) Facial nerve function after parotidectomy. Arch Otolaryngol Head Neck Surg 123(10):1091–1096
Gaillard C, Perie S, Susini B, Guily JL (2005) Facial nerve dysfunction after parotidectomy: the role of local factors. Laryngoscope 115(2):287–291
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Maithani, T., Pandey, A.K. & Agrahari, A.K. An Overview of Parotidectomy for Benign Parotid Lesions with Special Reference to Perioperative Techniques to Avoid Complications: Our Experience. Indian J Otolaryngol Head Neck Surg 71 (Suppl 1), 258–264 (2019). https://doi.org/10.1007/s12070-018-1261-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1261-3