Abstract
To assess and compare cytogenic damage in the form of micronuclei in various oral lesions according to duration and frequency of tobacco use. The present cross sectional study was carried out from October 2015 to October 2016. We included total 420 cases with 60 cases in each of the following subgroups, no tobacco habit with no obvious oral lesion (control) and tobacco habit with no obvious oral lesion, oral sub mucous fibrosis, leukoplakia, melanoplakia, erythroplakia, oral squamous cell carcinoma. Oral mucosal cells were collected from both sides of cheek; slides were prepared and examined for cells with micronuclei. The mean micronuclei index distribution in control group, potentially malignant group, and malignancy group was 1.14, 2.63, and 4.88 respectively and was statistically significant. The mean micronuclei index in control group, smoking tobacco and smokeless tobacco group was 1.14, 2.64, and 2.76 and was statistically significant. The mean micronuclei index was significantly higher in those using tobacco, for longer duration and with frequent tobacco use. The mean micronuclei index can be used as a potential screening tool of genotoxic damage and biomarker for epithelial carcinogenesis. The method has practical utility for warning tobacco users that higher than range has a danger of malignant event and therefore this in future can be used as reinforcement to advice of avoiding tobacco before malignancy develops.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral cancer is one of the most common causes of morbidity and mortality nowadays. In developing countries, both smoking, and smokeless tobacco have cancer-causing behavior that continues to be increasing the global burden of oral cancer. The World Health Organization estimated that the proportion of deaths that result from tobacco-related diseases would rise in India [1, 2]. The majority of the oral cancers preceded by the potentially malignant lesions and conditions (potentially malignant diseases [PMD’s]) [3]. These lesions clinically show premalignant mucosal changes that give a warning of risk and at hand an opportunity for detection and preventive measures. Early diagnosis of a potentially malignant lesions and sometimes cancerous lesions may improve the survival and the morbidity of patients; micronuclei (MN) are good prognostic indicators [4].
Main cause of oral carcinoma and precancerous conditions of mouth is the tobacco; both smokeless and smoked versions are equally responsible. Factors such as genetic, environmental and gene environmental interactions, viral, and behavior (smoking, alcohol) have been implicated in the etiopathogenesis of oral cancer [5]. One of the hallmark of cancer progression is DNA damage, resulting either from various carcinogens accumulating from etiologic influences or due to genetic errors [6].
To evaluate genotoxic effects in tobacco users on buccal mucosa, DNA damage can be assessed by chromosomal aberrations, sister chromatid exchanges and micronuclei test [3, 5]. Out of these micronucleus test found to be most easy, sensitive, non-invasive and very economical [7]. A micronucleus (MN) is formed during the metaphase/anaphase transition of mitosis (cell division). The literal meaning of the word micronucleus (MN) describes it as a small nucleus in a large cell, or the smaller nuclei in cells that have two or more such structures. Micronuclei assay in exfoliated buccal mucosal cells is a useful and minimally invasive method for monitoring genetic damage in humans in comparison to obtaining blood samples for lymphocyte, fibroblasts [8, 9].
Oral mucosal cells are the first barrier for ingestion or inhalation route and are capable of metabolizing proximate carcinogens to reactive products. Approximately 90% of human cancers originate from epithelial cells [10]. They represent preferred target site for early genotoxic events induced by carcinogenic agents entering the body through inhalation and ingestion. Our study separately assesses and compares the effects of smokeless and smoked tobacco on the oral mucosa and compares with habit free controls [10]. It will also be evaluated whether the frequency and duration of tobacco habit are proportional to the damage caused [5].
Materials and Methods
This cross sectional study was conducted in the department of Otorhinolaryngology and Head Neck surgery at Medical College and Sir Sayajirao General Hospital, Baroda, Gujarat from October 2015 to October 2016.
Study Subjects
Inclusion Criteria
A total of 420 cases with 60 cases in each of the following sub-groups, (a) no tobacco habit with no obvious oral lesion (control group), (b) tobacco habit with no obvious oral lesion, (c) tobacco habit with oral sub mucous fibrosis, (d) tobacco habit with leukoplakia, (e) tobacco habit with melanoplakia, (f) tobacco habit with erythroplakia, (g) tobacco habit with stage I and stage II oral squamous cell carcinoma.
Exclusion Criteria
Those with (a) extremely poor oral hygiene, (b) age less than 10 years, (c) on long-term orthodontic therapy, (d) chronic source of irritation in oral cavity, (e) alcohol usage, (f) occupational exposure to various chemicals, (g) stage III and IV oral squamous cell carcinoma, (h) known carcinoma patients on chemotherapy and/or radiotherapy were excluded from the study.
Collection of Oral Epithelial Cells
Subjects were asked to rinse the mouth thoroughly with 2 M Saline. Oral mucosal cells were collected from both sides of cheek using two separate clean wooden spatulas. Buccal cells were collected. Transported and processed.
Slide Preparation and Staining
Epithelial cell smears were prepared by spreading the cells on a clean slide, by using liquid cytology. The slides were stained with the papanicolaou stain. RAPID PAP kit used for staining.
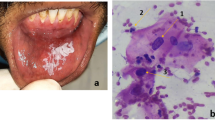
MN Scoring
From each slide, at least 1000 cells were examined under the light microscope using low magnification (× 40) for screening and high magnification (1000×) for counting of MN. Scoring of at least 1000 cells was done under high power compound binocular microscope with Battlefield zigzag method and total number of cells with MN calculated. We had used image capturing system to reduce inter and intra observer bias (Fig. 1).
A MN Index was assigned for exfoliated oral mucosal cells as number of cells with MN/total number of cells counted × 100. Also Mean MN Index was calculated as total number of cells with MN/Total number of study subjects. Two subject specialist observers did it to avoid bias.
Scoring Criteria
Criteria developed by Tolbert et al. (Tolbert’s criteria) [11, 12] for choosing the MN are (a) rounded smooth perimeter suggestive of a membrane, (b) less than a third the diameter of associated nucleus, but large enough to discern shape and color, (c) Feulgen positive, i.e. pink in bright field illumination, (d) staining intensity similar to that of nucleus, (e) texture similar to that of nucleus, (f) same focal plane as nucleus; (g) absence of overlaps with or bridge to the nucleus.
Master charts were prepared for mean MN counts per 100 cells (MN index) separately for tobacco nonusers, tobacco users with no oral lesions and tobacco users with various oral lesions. Also smokeless, smoked tobacco habit and individuals with no form of tobacco habit compared on the basis of frequency and duration of tobacco habit. The mean and standard deviation were calculated. Analysis of variance followed by paired and unpaired t test was then applied to compare the groups between themselves.
Results
Demographics
420 study subjects were evaluated in our department from October 2015 to October 2016. The mean and median age of subjects in our study was 44 and 45 years (17–84 years) with male to female ratio of 2:1. 25% of the potentially malignant cases were in the age group 31–40 years. 36% of the malignant cases were in the age group 41–50 years. This may be due to the fact that as age increases risk of malignancy and exposure to genotoxic agents is more.
The mean micronuclei index in malignancy group was 4.88 and it was 3.23 in the eryrthroplakia group, 2.86 in the submucous fibrosis group, 1.81 in the leukoplakia group, 1.77 in melanoplakia group, and in the control group it was 1.14 (Table 1).
The mean micronuclei index in potentially malignant group (erythroplakia, submucous fibrosis and leukoplakia) was 2.63 and it was 4.88 in the malignancy group, and in the control group it was 1.14. A significant (p < 0.05) stepwise increase was found in the mean number of cells with micronuclei from control to precancer patients, and from precancer to cancer patients. While comparing cancer with the control group, p value was significant at the level of 0.0001, and while comparing precancer with the control group p value was highly significant (Table 2).
The mean micronuclei index in smokeless tobacco group was 2.76 and it was 2.64 in the smoking tobacco group, and in the control group it was 1.14. A significant (p < 0.05) increase was found in the mean micronuclei index from non-tobacco users group to tobacco users group. The difference between total number of cells with MN was not appreciable between smokeless and smoked tobacco groups (p > 0.05), though the total number of cells with MN was higher in subjects using smokeless tobacco (SLT) (Table 3).
The mean micronuclei index in those using tobacco, for less than 5 years was 2.24 and it was 3.03 in those using tobacco, for more than 5 years, and in the control group it was 1.14. Mean total number of cells with MN was significantly higher in those using tobacco, for more than 5 years as compared to less than 5 years, compared to controls. A significant (p < 0.05) stepwise increase was found in the mean micronuclei index from control to those using tobacco, for less than 5 years as compared to those using tobacco for more than 5 years (Table 4). The total numbers of cells with MN were significantly higher in those with frequent use of tobacco as compared with less frequent tobacco users (p < 0.05).
Discussion
The use of a biomarker as an indicator of disease development is that the marker will translate into a relationship between exposure and disease [9]. The only cytogenetic biomarker that has been outlined previously is the technique of classical metaphase analysis for measurement of chromosomal aberrations in human lymphocytes. While MN assay is one of the most commonly used methods for measuring DNA damage in human populations because it is relatively easier to score MN than chromosomal aberrations [13].
Biomonitoring of the changes in patients with diagnosed diseases or pathological changes that may lead to development of cancer and other illnesses is becoming increasingly popular, and may be the most rapidly growing area of application of the MN assay to epithelial cells [14]. Micronuclei are suitable internal dosimeters for revealing specific tissue specific genotoxic damage in individuals exposed to carcinogenic mixtures [3]. Epithelial cells are highly proliferative and are the origin of more than 90% of all human cancers. Therefore the application of micronucleus test in epithelial cells is considered to be sensitive tool for biomonitoring the genetic damage in human population [15].
In the present study, the oral mucosal micronuclei index in the control population was 1.14. In subjects with potentially malignant disorders, the mean micronuclei index was 2.63 and in the cancer patients, the mean micronuclei index was 4.88. In our study a stepwise increase in micronuclei index was observed from control to precancer patients and from precancer to cancer patients. Parvati et al. [15] conducted a similar study and found the mean percentage of micronuclei noted in precancerous group was 0.12% and in cancerous lesions was 0.45%. Parvati et al. suggested a link of this biomarker with neoplastic progression. In accordance with our study, the study conducted by Sangle et al. [16], Palve and Tupkari et al. [4] concluded that there was a gradual increase in micronucleus counts from normal mucosal group, potentially malignant group, to squamous cell carcinoma group, respectively. According to Samanta and Dey et al. [17] the various possible explanations for micronuclei formation in preneoplastic conditions include chromosomal aberrations, chromosomal loss, mitotic apparatus dysfunction, aneuploidy and genetic instability.
The present study evaluated the mean number of micronuclei in smokeless tobacco users, smokers, and the healthy controls. The result showed that the overall level of mean number of cells with micronuclei in smokeless tobacco were higher (2.76) as compared with smokers (2.64) and controls (1.14). This observation was similar to Ozkul et al. [18], Palaskar et al. [19], Bansal et al. [20].
Ozkul et al. compared micronuclei formation in the buccal mucosal cells of smokeless tobacco users with those of the smokers and found that the mean percentage of the micro nucleated cells was 1.86 in the smokeless tobacco users and 1.99 in the smokers. But there was no difference between the mean percentages of the micro nucleated cells in these two groups (p > 0.05).
This can be explained on the basis of smokeless tobacco chewing habit in which the mucosa is in constant contact with the tobacco for longer period causing DNA damage to the mucosal cells by the local absorption of genotoxic agent, that is, nitrosamine present in the tobacco [10, 19]. Besides the use of smokeless or smoked forms of tobacco, there are multiple other reasons for occurrence of MN cells. It has been established that genomic damage is produced by exposure to genotoxic substances, medical procedures (radiation and chemicals), micronutrient deficiency (alpha tocopherol, folic acid), life‐style (alcohol, smoking, drugs, stress), urban pollution, chronic contact with arsenic and genetic factors, such as defects in metabolism and/or in the repair of DNA [21]. Hence, this assay serves as an indicator of DNA damage in a group and fails to predict risk at an individual level.
Shetty et al. [5] concluded that the risk of carcinoma increases with the duration of tobacco habit. Patel et al. [9] found that the mean total number of cells with MN were significantly higher in those using tobacco for longer duration and more frequently. He used Lifetime tobacco exposure (LTE); an arbitrary unit obtained using frequency/day multiplied by duration of years for comparison. Patel et al. [9] found that controls having MNC above cutoff level have greater risk of genotoxicity. Similar to Patel et al., and Shetty et al., in our study the total numbers of cells with MN were significantly higher in those tobacco users with longer duration (> 5 years) and more frequent use of tobacco as compared with short duration tobacco users (< 5 years) with less frequent tobacco usage.
Screening of individuals who are at high risk of malignant transformation is more pivotal in preventing and reducing the number of deaths than the costly and painful treatment later on [15]. From the present study, it is evident that the individual cancer risk was predicted on the basis of increased percentage of micronuclei in the oral epithelial cells and it helps in identifying those patients with precancer who were at the high risk of developing cancer. As most oral cancers presumed to originate from precancerous lesions or conditions, it is highly desirable to identify high-risk individuals and counsel them [14]. Furthermore, increased micronuclei index in the grossly normal appearing oral mucosa of the high risk individuals is associated with greater risk of oral cancer development as suggested by concept of field carcinogenesis [9]. Few patients are usually unwilling to reveal the duration, frequency and other associated habits during case history recording. The buccal exfoliated cells should also be collected after stoppage of habit to check for the decrease in the number of cells with MN and level of genotoxicity.
Conclusion
Mean MN index can be used as a potential screening tool and biomarker of genotoxic damage and for epithelial carcinogenesis. The mean MN Index is positively correlated with duration and frequency of tobacco use. Those patients who have quit the habit of tobacco should also be followed up for the MN index to correlate and to document the reversibility of the genotoxicity.
The method has practical utility for warning tobacco users that higher than range has a danger of malignant event and therefore this in future be used as a reinforcement to advice of avoiding tobacco before malignancy develops. This study reveals that smokeless and smoked formed of tobacco is highly genotoxic and responsible for oral precancerous lesions, conditions and cancer in near future.
References
American Cancer Society (2015) International Agency for Research on Cancer. Global cancer facts and figures, 3rd edn. Atlanta, pp 1–57
Jandoo T, Mehrotra R (2008) Tobacco control in India: present scenario and challenges ahead. Asian Pac J Cancer Prev 9:805–810
Halder A, Chakraborty T, Mandal K, Gure PK, Das S, Raychowdhury R, Ghosh AK, De M (2004) Comparative study of exfoliated oral mucosal cell micronuclei frequency in normal, precancerous and malignant epithelium. Int J Hum Genet 4(4):257
Palve DH, Tupkari JV (2008) Clinico-pathological correlation of micronuclei in oral squamous cell carcinoma by exfoliative cytology. J Maxillofac Pathol 12:2–7
Shetty Suchitra A, Khandige Shreesha (2015) Tobacco use: a study of its cytogenetic and DNA damaging ability. J Evid Based Med Healthc 2(46):8210–8211. https://doi.org/10.18410/jebmh/2015/1106
Warnakulasurya S (2009) Significant oral cancer risk associated with low socioeconomic status. Evid Based Dent 10:4–5
Pratheepa Sivasankari N, Kaur S, Reddy KS, Vivekanandam S (2008) Micronucleus index: an early diagnosis in oral carcinoma. J Anat Soc India 57:8–13
Alexandrescu I, Havârneanu D, Popa D (2006) New approaches in biomonitoring human populations exposed to genotoxic agents: epithelial cell micronucleus assay. J Prev Med 14(3–4):57–65
Patel BP, Trivedi PJ, Brahmbhatt MM, Shukla SN, Shah PM, Bakshi SR (2009) Micronuclei and chromosomal aberrations in healthy tobacco chewers and controls: a study from Gujarat, India. Arch Oncol 17(1–2):7–10
Motgi AA, Chavan MS, Diwan NN, Chowdhery A, Channe PP, Shete MV (2014) Assessment of cytogenic damage in the form of micronuclei in oral epithelial cells in patients using smokeless & smoked form of tobacco and non-tobacco users and its relevance for the oral cancer. J Can Res Ther 10:165–170
Tolbert PE, Shy CM, Allen JW (1992) Micronuclei and other nuclear anomalies in buccal smears: methods development. Mutat Res 271:69–77
Tolbert PE, Shy CM, Allen JW (1991) Micronuclei and other nuclear anomalies in buccal smears: a field test in snuff users. Am J Epidemiol 134:840–850
Fenech M (2002) Chromosomal biomarkers of genomic instability relevant to cancer. Drug Discov Today 7:1128–1137
Saran R, Tiwari RK, Reddy PP, Ahuja YR (2008) Risk assessment of oral cancer in patients with precancerous states of the oral cavity using micronucleus test and challenge assay. Oral Oncol 44:354–356
Devi P, Thimmarasa VB, Mehrotra V, Arora P (2011) Micronucleus assay for evaluation of genotoxicity in potentially malignant and malignant disorders. J Indian Acad Oral Med Radiol 23(2):97
Sangle VA, Bijjaragi S, Shah N, Kangane K, Ghule HM (2016) Comparative study of frequency of micronuclei in normal, potentially malignant diseases and oral squamous cell carcinoma. J Nat Sci Biol Med 7(1):33–38
Samanta S, Dey P (2012) Micronucleus and its applications. Diagn Cytopathol 40:84–90
Ozkul Y, Donmez H, Erenmemisoglu A, Demirtas H, Imamoglu N (1997) Induction of micronuclei by smokeless tobacco on buccal mucosa cells of habitual users. Mutagenesis 12:285–287
Palaskar S, Jindal C (2010) Evaluation of micronuclei using papanicolaou and may Grunwald-Giemsa stain in individuals with different tobacco habits: a comparative study. J Clin Diagn Res 4:3607–3613
Bansal H, Sandhu VS, Bhandari R, Sharma D (2012) Evaluation of micronuclei in tobacco users: a study in Punjabi population. Contemp Clin Dent 3:184–187
Fenech M, Holland N, Chang WP, Zeiger E, Bonassi S (1999) The human micronucleus project—an international collaborative study on the use of the micronucleus technique for measuring DNA damage in humans. Mutat Res 428:271–283
Holland N, Bolognesi C, Kirsch-Volders M et al (2008) The micronucleus assay in human buccal cells as a tool for biomonitoring DNA damage: the HUMN project perspective on current status and knowledge gaps-review. Mutat Res 659:93–108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest in the submission of this manuscript.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Ethical Approval
All procedures performed in the studies involving human participant were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wagh, A., Raval, J., Aiyer, R.G. et al. Micronuclei in Exfoliated Oral Epithelial Cells in Tobacco Users and Controls with Various Oral Lesions: A Study from Gujarat, India. Indian J Otolaryngol Head Neck Surg 71, 109–114 (2019). https://doi.org/10.1007/s12070-018-1260-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1260-4