Abstract
Otitis media with effusion (OME) is a common condition affecting children. It is one of the most common causes for reduced hearing in pediatric age group leading to various learning disabilities including delayed speech development. The aim of this study was to find out various epidemiological characteristics and risk factors for developing OME and various treatment modalities depending on the clinical features and their outcomes in urban pediatric population. A prospective comparative study was done in 100 children taken 50 as cases and 50 as controls for a period of 2 years. The risk factors, common presenting features and the examination and investigational findings (tympanometry) of the study condition were compared among the cases and controls. Among the 50 cases, 28 children were treated medically and 22 underwent surgical treatment in the form of Myringotomy and Grommet insertion. The patients were followed up-to 6 months in both groups.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Otitis media with effusion is defined as a serous or mucoid collection of fluid in the middle ear space and sometimes in the mastoid air cell system. This condition synonymously referred to as secretory, catarrhal, exudative, seromucinous or non-suppurative otitis media. The term otitis media with effusion allows differentiation of the type of effusion and facilitates distinction between acute and chronic forms.
The causative factors for formation and persistence of fluid collection include chronic inflammation within the middle ear and Eustachian tube dysfunction. As Eustachian tube dysfunction causes inadequate gas exchange into the middle ear space, increasingly negative middle ear pressures develop, resulting in the formation of a transudate that fails to clear.
Eustachian tube dysfunction arises from inflammatory disorders, muscular abnormalities, and anatomic factors. In children, the Eustachian tube is smaller, more flexible and has a more horizontal orientation when compared to adults, which might help explain the relatively greater incidence of otitis media with effusion in children. Dysfunction can result from congenital abnormalities, such as cleft palate or myopathies that affect the palatal musculature and consequently the dynamic excursion of the orifice of the Eustachian tube. Inflammation is probably one of the more common causes of tubal problems resulting from mucosal edema with mucous production, and it can arise from any of a number of etiologies, such as, allergic disease, laryngopharyngeal or gastroesopahgeal reflux, syndromic or smoking related ciliary dysmotility, and middle ear/nasopharyngeal biofilms. Anatomic obstruction of the Eustachian tube can result from prominent adenoid tissue, synechiae from surgery, or nasopharyngeal masses.
Aims of the Study
-
To find out various epidemiological characteristics and risk factors of otitis media with effusion (OME) among urban pediatric population in a tertiary care centre.
-
To study the natural history of the disease, therapeutic interventions based on the clinical features and the various outcomes.
Materials and Methods
50 consecutive patients (children between ages 1 and 10) attending Ear Nose Throat (ENT) outpatient department (OPD) with OME, taken as cases and 50 consecutive patients presented without OME taken as controls, during the period of July 2012 to June 2014. Patients were analyzed for different risk factors, symptoms suggestive of OME, Otoscopic examination was done to look for the condition of the tympanic membrane, Tympanometry was done to assess middle ear function and additional test like X-ray neck soft tissues lateral view taken for suspected adenoid hypertrophy.
We included children with (1) recurrent episodes of ear pain (more than 2 episodes), (2) decreased hearing, (3) history of ear discharge.
Children excluded from study were children having (1) otomycosis or otitis externa, (2) perforation of the ear drum, (3) presence of cholesteatoma, (4) immunodeficiency, (5) cleft palate and other cranio-facial abnormalities.
A uniform history was recorded for each patient including recurrent episodes of ear pain, fever, ear discharge or reduced hearing as felt by the parents/care takers. Parents were asked for relevant risk factors like advanced maternal age, birth order of the child, prematurity, history of Neonatal Intensive Care Unit (NICU) admission or intubation, history of breast or bottle feed during first 6 months, nose block or nasal discharge, allergy symptoms, viral infections, passive smoking, day care attendance, and any other sibling having history of OME.
Family structures (nuclear/joint) and type of accommodation in the form of apartment or separate house (villa) are also enquired.
Complete otologic examination by otoscope (WelchAllyn) done in all children.
Audiologic evaluation done by tympanometry/impedence audiometry (I/A) [1].
In children with suggestive history (nose block, mouth breathing), status of adenoid was checked by doing X-ray soft tissue neck lateral view.
After diagnosis, appropriate management was offered to the patients (case group).
Cases were allocated to two groups as per the treating consultants’ preference: non-surgical who underwent watchful wait for 6–12 weeks with symptomatic medical treatment [2] for cases with fever, rhinitis, nose block with: Antihistaminic (levoceterizine), Leukotriene receptor antagonists (montelukast), Nasal decongestanats (xylometazoline nasal drops), Antibiotics (amoxycilline/cephalosporine), and Intranasal steroid spray (mometasone nasal spray) and surgical group undergone myringotomy ± tympanostomy tube [2] (ventilation tube/grommet) insertion(Shah grommet) with or without adenoidectomy under general anesthesia. Culture ± sensitivity of the middle ear fluid sent in some cases and post op antibiotic guided accordingly. All surgeries were done under general anesthesia as day cases using operating microscope (Leica). Radial incision made over anteroinferior quadrant of tympanic membrane [3], Shah Grommet inserted after suctioning of middle ear fluid. Post operatively, patients were put on antibiotics, usually amoxicillin or 2nd generation cephalosporine, along with analgesic as required.
Routine follow-ups were conducted and treatment reviewed in view of clinical symptoms, examination and tympanometry findings. Outcomes at the end of 3 and 6 months were documented.
Improvement was considered with resolution of symptoms/type A or As tympanograms for medically treated or watchful wait group and presence of grommet for surgically treated group.
All patients are examined and treated (medical/surgical) as per decisions of the consultants of ENT Department.
Statistical Methods [4, 5]
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min–Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. The following assumption on data is made, Assumptions: 1. Dependent variables should be normally distributed, 2. Samples drawn from the population should be random, and cases of the samples should be independent. Chi square/Fisher Exact test has been used to find the significance of study parameters on categorical scale between two and more groups.
Statistical Software
The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Results
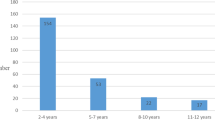
The study population comprised age range from 1 year to 10 years, among which, most common age group presented with OME was 3–5 years, (29 out of 50, 58%).
66% was male (33 of 50) and 34% (17 of 50) was female among cases and 50% in controls each (25 each male and female). The risk factor analysis revealed history of bottle feed, history of passive smoking, history of attending day care have statistical significance among the risk factors studied (Table 1). Presenting complaint among cases in descending order were recurrent episodes of ear pain—24 (48%), decreased response—14 (28%) noticed by parents, blocked sensation in the ears—7 (14%) as described by older children, nose block—3 (6%), ear discharge—2 (4%).
Presenting complaints among controls were rhinitis and mouth breathing 10 each (20% each), sore throat 9 (18%), nose bleed 5 (10%), nose block 4 (8%), ear block 3 (6%), neck swelling 2 (4%), decreased response, noisy breathing, tongue tie, foreign body in nose, itching in the ear, ear bleed, cough: 1 each (2% each).
The tympanic membrane was dull in majority of cases compared to controls which was statistically significant followed by congestion and/or retraction (Table 2). The condition of the ear drum was similar in both sides in 39 (78%) cases, of which, bilateral dull ear drum was seen in 30 cases (60%). 6 cases were bilaterally congested (12%), 2 cases were retracted (4%), bulging in 1 case (2%).
Upon impedence audiometry, B type tympanograms was a statistically significant finding among cases (Table 3). X-ray soft tissue neck lateral view showed adenoid hypertrophy (obstructing 50% of nasopharyngeal airway) in 30% of cases and 22.5% in controls.
For the study of outcomes of various treatment modalities, cases were divided into surgical (22) and medical/wait and watch (non surgical) group (28) and outcomes at the end of 3 and 6 months are calculated in terms of percentage who improved as per the criteria mentioned above. The difference in treatment modalities showed statistical significance at the end of 3 months but there was no significant difference in treatment groups after 6 months. (Table 4).
Discussion
The epidemiology of OME has been extensively studied in many countries, mainly in Denmark, Finland, the Netherlands, UK and USA.
Studies based on Indian population regarding the prevalence, clinical features and diagnosis, as well as outcomes of the various treatment modalities depending on standard guidelines, are lacking.
Zielhius et al. reviewed a total of 23 studies that all used tympanometry as one of the diagnostic instruments to give age-specific prevalence rates up to 10 years of age. The prevalence is bimodal with the first and largest peak of approximately 20% at 2 years of age. This is the age at which many children first attend a playgroup or nursery school. Thereafter the prevalence declines, but there is a second peak of approximately 16% at around 5 years of age when most children start attending a primary school [2].
We found that, 3–5 years of age comprised 58% of our cases, whereas less than 3 years were 20% and those who are more than 5 years comprised 22%. Male children were 66% and female were 34% in our cases. Hence in our study population, the most common age group affected by OME is 3–5 years of age, boys are more affected than girls, and 82% of our cases had bilateral OME as evidenced by flat (type B) tympanograms bilaterally.
A study by G Aydemir and FE Ozkurt, involving 423 children of age 7–12, Istanbul, Turkey revealed, number (no.) of upper respiratory infection and no. of acute otitis media episodes in the previous year, no. of students in the class and presence of snoring as risk factors for developing OME(P < 0.05). Other factors studied like allergic symptoms, duration of kindergarten attendance, duration of breast feeding, smoking by mother/father, no of siblings, no of family members, parental educational level or monthly income were not significant risk factors [6].
In our study, advanced maternal age (>30 years), P 0.073 and history of nose block, P 0.083 have suggestive significance (P value 0.05 < P < 0.10).
History of NICU admission/intubation, (P 0.038) is moderately significant, (P value 0.01 < P ≤ 0.05). History of bottle feed, P < 0.001, history of passive smoking, P < 0.001, history of attending day care, P < 0.001 are strongly significant (P value P ≤ 0.01).Birth order, prematurity, perinatal complication, history of major viral infection, history of allergy, history of sibling having OME, developmental history, immunization status, accommodation pattern, family structure have no significant association with the study condition.
Secondary acute infections of the middle ear fluid may lead to otalgia and otorrhoea which coincide with a cold, upper respiratory tract infection or period of allergic rhinitis. Otoscopy is required visually to confirm the presence of an effusion.
Tympanometry provides an objective assessment of the middle ear status, unreliable in children under 6 months old. Type B traces are highly sensitive in detecting effusions [7].
In our study we found, most of the children with OME had history of recurrent episodes of ear pain (48%) and decreased hearing (28%). Nose block and ear block were less common presenting complaints (6 and 14% respectively). The commonest appearance of tympanic membrane was dull in both sides on Otoscopy (60 and 74% in right and left ear respectively). B type tympanograms were obtained in most ears (82 and 88% for right and left ear respectively).
Rosenfeld RM and Kay D, in a systemic review and meta-analysis concluded that the natural history of otitis media is very favourable. OME after untreated AOM had 59% resolution by 1 month (95% Confidence Interval (CI) 50–68%) and 74% resolution by 3 months (95% CI 68–80%). OME of unknown duration had 28% spontaneous resolution by 3 months (95%, CI 14–41%), rising to 42% by 6 months (95% CI 35–49%). In contrast, chronic OME had only 26% resolution by 6 months and 33% resolution by 1 year [8].
In their article published in The Laryngoscope, 1985, Casselbrant M.L, et al. mentioned that OME has a high spontaneous recovery in preschool children [9].
Tos M recommended that spontaneous improvement of secretory otitis media occurs frequently, and it is recommended to wait 3–6 months before instituting surgical treatment [10].
Among 28 children with OME, followed up with watchful wait and/or symptomatic treatment as mentioned earlier in our study, 27 children showed spontaneous improvement at the end of 3 and 6 months.
In a systemic review of the ventilation tube treatment, Hellstrom S et al. concluded that there is strong scientific evidence (grade 1) that ventilation tube (VT) treatment of SOM improves hearing for at least 9 months and that Quality of Life (QoL) is improved for up to 9 months (grade 2 scientific evidence) [11].
The Agency for Healthcare Research and Quality (AHRQ) research review of Otitis Media with Effusion: comparative effectiveness of treatment, based on studies examined interventions in otherwise healthy, noninfant children found that tympanostomy tube (TT) decreased OME for 2 years compared with watchful waiting (WW) or myringotomy (myr), and improved hearing for 6 months compared with WW [12].
Sundberg L. presented a study consisted of 119 children with SOM lasting 3 months or more. The results suggest that a ten day course of erythromycin could reduce the need for surgical treatment in children with long-standing Secretory Otitis Media (SOM) [13].
Determining the effectiveness of antibiotic therapy for otitis media with effusion (OME), Cantekin E.I and McGuire T.W concluded that their meta –analysis fail to support the continued use of antibiotics in the treatment of OME. RCTs evaluating the efficacy of antimicrobials for the treatment of OME with or without placebo controls were selected and using weighted regression analysis to account for the effects of study quality on efficacy, they found that antimicrobial efficacy for OME is insignificant, less than 2% for an ideal clinical trial (P = 0.660) [14].
In our study, 28 children were followed up with watchful wait and symptomatic treatment and 27 patients (96.4%) improved after 3 months. There was resolution of symptoms like improved hearing response and/or no further episode of ear pain. The tympanometry showed A type. When followed up-to 6 months, the percentage of improvement was sustained. Children who were treated with myringotomy and grommet insertion 11 out of 22 children improved at 3 months (50%) indicated by resolution of presenting symptoms with a presence of grommet in the ear drum. 50% patient had recurrence of symptoms/otorrhoea/grommet extrusion with flat tympanograms. When followed up-to 6 months, the percentage of improvement was increased to 77.3%. When surgical and non-surgical group were compared, the medical/wait and watch group has statistically significant improvement (P value <0.001) at 3 months. But at 6 month, the difference in improvement was only suggestive, but not very significant (P value 0.075).
Conclusions
Otitis media with effusion is a bilateral condition, common in age group of 3–5 years in urban pediatric population. The diagnosis can be suspected in children presenting with history of recurrent ear pain and/or a decreased hearing response.
Significant risk factors for developing the condition among the study population include: advanced maternal age (>30 years), history of nose block, history of NICU admission/intubation, history of bottle feed, history of passive smoking, history of attending day care.
The Otoscopic finding of OME is dull tympanic membrane, associated with a B trace in Impedence Audiometry.
Spontaneous resolution of the condition occurs in majority of children with a wait and watch policy for 3–6 months.
Recommendations and Future Scope
A diagnosis of OME can be suspected in children aged 3–5 years presenting with recurrent episodes of ear pain or child/parent reported decreased hearing response.Parents should be informed about the modifiable risk factors associated with OME like passive smoking, day care attendance and bottle feed, and lifestyle modifications that will affect above factors to be actively encouraged.
Otoscopy is a useful and easy tool of diagnosing OME in children in OPD settings, along with type B tympanograms, hence all children with suspected OME should have Otoscopic examination and impedence audiometry.
Children with OME beyond 3 months may be watched for another 3 months or offered the surgical treatment (myringotomy and grommet insertion).
Since this condition has innocuous symptoms which are often ignored by the care givers, awareness of the condition and the consequences of non treatment should be spread not only amongst caregivers but also family practitioners and pediatricians.
In spite of the present evidence of TT improving hearing in OME children, this treatment is not without complications. Hence large, well-controlled studies would help resolve the risk–benefit ratio by measuring acute otitis media recurrence, functional outcomes, quality of life measures, and long-term outcomes. Moreover, children with craniofacial abnormalities and other co morbidities would definitely need further sub-grouping for better treatment decisions.
References
Stool SE, Berg AO, Berman S, Carney CJ, Cooley JR, Culpepper L et al (1994) Managing otitis media with effusion in young children: American academy of pediatrics. The otitis media guideline panel. Pediatrics 94(5):766–773
Browning G (2008) Otitis media with effusion. In: Scott-Brawn’s otorhinolaryngology, head and neck surgery. 7th ed. Hodder Arnold, London, 2008
Guttenplan MD, Tom LW, DeVito MA, Handler SD, Wetmore RF, Potsic WP (1991) Radial versus circumferential incision in myringotomy and tube placement. Int J Pediatric Otorhinolaryngol 21:211–215
Riffenburg RH (2005) Statistics in medicine, 2nd edn. Academic Press, Cambridge, pp 85–125
Sunder Rao PSS, Richard J (2006) An introduction to biostatistics, a manual for students in health sciences, 4th edn. Prentice Hall of India, New Delhi, pp 86–160
Aydemir G, Ozkurt FE (2011) Otitis media with effusion in primary Schools in Princes’ Islands, Istanbul: prevalence and risk factors. J Int Med Res 39:866–872
Richard Maw A (2006) Secretory otitis media. In: Ludman H, Wright T (eds) Diseases of the ear, 6th edn. Arnold, London
Rosenfeld RM, Kay D (2003) Natural history of untreated otitis media. Laryngoscope. 113(10):1645–1657
Casselbrant ML, Brostoff LM, Flaherty MR, Bluestone CD, Cantekin EI, Doyle WJ et al (1985) Otitis media with effusion in preschool children. Laryngoscope 95(4):428–436
Tos M (1983) Epidemiology and spontaneous improvement of secretory otitis. Acta Otorhinolaryngol Belgica 37(1):31–43
Hellström S, Groth A, Jörgensen F, Pettersson A, Ryding M, Uhlén I, Boström KB (2011) Ventilation tube treatment: a systematic review of the literature. Otolaryngol Head Neck Surg 145(3):383–395
AHRQ Research Review. Otitis media with effusion: comparative effectiveness of treatment. AHRQ Publication No. 13-EHC091-EF; May 2013
Sundberg L (1984) Antibiotic treatment of secretory otitis media. Acta Otolaryngol Suppl 407:26–29
Cantekin EI, McGuire TW (1998) Antibiotics are not effective for otitis media with effusion: reanalysis of meta-analyses. Otorhinolaryngol Nova 8:214–222
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bandyopadhyay, T., Raman, E.V. Otitis Media with Effusion (OME) in Urban Pediatric Population in a Tertiary Care Centre: A Clinical Study. Indian J Otolaryngol Head Neck Surg 70, 267–272 (2018). https://doi.org/10.1007/s12070-017-1178-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-017-1178-2