Abstract
In this paper we used wave 1 (2002) to wave 6 (2012) of the English Longitudinal Study of Ageing (ELSA) to assess whether trajectories in the prevalence of self-reported limiting long term illness differed before and after retirement and whether any such differences in slope were found across socio-economic characteristics and the conditions of work in the final years of employment. The longitudinal analysis used a sub-sample of ELSA comprising those who retired between wave 2 (2004) and wave 6 (2012). We fitted a repeated measure logistic regression to model the trajectory in the log odds of illness before and after retirement. We found evidence of a slower increase in self-reported illness after than before retirement that was most strongly observed for those in the least favourable circumstances prior to retirement (lower social class, depressed prior to retirement and single). A similar retirement effect was observed for those in physically demanding occupations. Whilst we did not detect differences in post and pre-retirement slopes according to other aspects of working conditions we found higher rates of self-reported illness for individuals involved in unsatisfying jobs or in work where demands exceed rewards. These differentials were robust to inclusion of information on socio-economic circumstances and appeared to persist beyond retirement. Our interpretation of the results is that disadvantage across the life course makes those in the least favourable circumstances or involved in physically demanding work less able to draw on social, economic and health reserves to cope with the demands of work in the final years of employment. As a result these groups of disadvantaged individuals experienced a slower increase in rates of illness after than before retirement when the demands of work are removed. Proposals to increase retirement age without also tackling inequalities in circumstances in the final years of employment are likely to increase inequalities in self-reported health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This paper examines trajectories, or change, in the prevalence of self-reported limiting long-term illness (LLTI) around retirement, for older, community dwelling individuals in England between 2002 and 2012. The English Longitudinal Study of Ageing, a nationally representative dataset, is used to consider whether the rate of change in the prevalence LLTI prior to retirement differs to that observed after retirement and whether any differences in trajectories of LLTI on either side of retirement vary according to socio-economic circumstances and the perceived conditions of work.
Retirement has emerged as a key issue within research and policy that addresses the issues of population ageing and health inequalities. Many Western countries have implemented policies to increase the Statutory retirement age (Hamblin 2010; Pond et al. 2010); for example, within the UK, the Pension Act of 2011 laid out a timetable for increasing the Women state pension age from 60 to 65 by 2018 and increasing the state pension age of both men and women to 68 by 2046. The justifications for such policies are linked to claims that a population that is living longer has greater capacity to work to older ages and that increased numbers of workers are needed to cope with the demands and costs of a growing elderly population (Angel and Mudrazija 2011; Harper et al. 2011). However, it is also argued that increasing the age of retirement may have unintended negative consequences in terms of perceived fairness and associated societal cohesion given the stark inequalities in life and healthy life expectancy at retirement according to social position. And it is feared that increasing the Statutory retirement age may exacerbate the extent of health inequalities between social groups and areas at the older ages (Bellaby 2006; Marshall and Norman 2013; Harper et al. 2011; Angel and Mudrazija 2011). In response to such issues, Harper et al. (2011) propose alternative approaches to defining retirement age that reflect inequality in socio-economic circumstances at retirement, for example, a retirement age graduated by lifetime earnings or time spent in the labour market, that provide a means to respond to the challenge of population ageing without exacerbating health inequalities. In this context a clear understanding of trajectories in the prevalence health outcomes through retirement according to socio-economic circumstances and working conditions provides a valuable contribution to a contemporary issue.
One of the challenges in conducting research on the impact of retirement on subsequent outcomes is that retirement can be defined in a number of different ways and at the same time there are various different pathways into retirement. Banks and Smith (2006) identify thee commonly used definitions of retirement including complete and permanent withdrawal from the labour market; receipt of income from a state or private pension; or through individual’s self-definition. What is clear however, is that regardless of the definition used, the majority of people in the UK retire before the working age, a result that is partly explained by the decline in levels of economic activity in the UK, and most other Organisation for Economic Cooperation and Development (OECD) countries (Delson 1996). Banks and Smith (2006) distinguish two pathways into retirement that are strongly patterned according to wealth and social position. The poorest individuals tend to transition out of the labour market into retirement through sickness benefits, a retirement route that is thought to have been driven in part by the collapse in the demand for unskilled labour in many developed countries from the 1980s (Burstrom 2000). For the richest individuals early retirement is financed through occupation pension schemes or through accumulated wealth and investments. A crucial aspect of retirement and its impact on subsequent outcomes is whether the decision to retire is voluntary (e.g., to spend time with family or a partner or to fulfill other ambitions outside work) or involuntary (e.g., as a result of illness, redundancy or failure to find work) (van Solinge 2007). Evaluating the route into retirement is itself complicated by the post-hoc rationalisation process that may mask the influence of involuntary retirement factors.
A body of research has considered how and whether retirement influences inequalities in health post-retirement. Much of this work draws on Retirement Adjustment Theory (Atchley 1976) which suggests that individuals who retire are required to adjust to retired life with the potential for both positive and negative responses to this transition that can then impinge on health. The nature of the transition to retired life is thought to be strongly patterned according to individual and contextual characteristics (for a detailed review of the theoretical literature see Rijs et al. (2012). For example, if an individual is involved in work that is particularly arduous, stressful or unrewarding then we might expect retirement to offer a positive adjustment with the potential for improved health through the removal of these aspects of work that are harmful to health (Mein et al. 2003) and additional time to engage in exercise and other activities with health and wellbeing benefits (Midanik et al. 1995; Mein et al. 2003; Mojon-Azzi et al. 2007). On the other hand an individual might find the adjustments to life after retirement stressful with negative health consequences, especially if retirement is associated with a loss identity or income or if they simply struggle to cope with a new way of life involving less structure and purpose (Reitzes et al. 1996).
In terms of individual characteristics we might expect more educated individuals or more affluent individuals to be better resourced and more likely to be equipped with the social skills to identify and fulfill objectives in retirement (Reitzes and Mutran 2004). Men and women may experience retirement differently because of different experiences within the labour market and in terms of subsequent pension provision, for example (Ginn and Arber 2001). Individuals living as a couple may be able to adjust to a shared retired life more easily than those living alone, but only if the prospect of sharing more time with a partner is an attractive one and this appears to vary by gender (Hillbourne 1999). Poor health in the final years of employment may serve as an involuntary pathway to retirement and lead to poorer health after retirement or, conversely, those individuals in poor health prior to retirement may experience improved health outcomes once removed from the demands of work. The route into retirement, and in particular whether this is voluntary or involuntary, is thought to be a determinant of subsequent health outcomes with those individuals who choose to retire experiencing better outcomes in retirement (van Solinge 2007). Research has suggested that demands of work have shifted from physical to psychological, reflecting changes to structure of employment that have made it less secure and less certain, and, as such, psychological characteristics such as self-esteem, depression and wellbeing prior to retirement may all impinge on the ability to adjust to retired life. Again the pathways are contested; those who have low self-esteem or who are stressed in work may have less capacity to adjust successfully to retired life or they may welcome the release from work demands. The literature suggests that any examination of the impact of retirement on health ought carefully consider the demographic, socio-economic, job/retirement characteristics and psychological factors that may influence retirement and self-reported health (Rijs et al. 2012).
Perhaps in part reflecting the complicated theoretical perspectives on the various pathways through which retirement is thought to influence subsequent health outcomes, in both positive and negative directions, the empirical findings on the impact of retirement on health are also mixed. Conclusions appear to differ according to the aspect of health under investigation, the nature of analysis performed (e.g., cross-sectional versus longitudinal) the timing and reason for retirement and according to socio-economic circumstances. Van der Heide et al. (2013) present a valuable review of findings from 22 studies, selected according to strict methodological criteria, that examine the impact of retirement on mental health, physical health and perceived general health. The review suggests retirement has a positive effect on mental health but for physical and for perceived general health the impact of retirement is ambiguous. An important set of studies reviewed by Oksnanen and Virtanen (2012) are based on occupational studies in France and Finland and have suggested that retirement is associated with improvements in self-reported health (Westerlund et al. 2009), mental and physical fatigue and depressive symptoms (Westerlund et al. 2010), sleep problems (Vahtera et al. 2009) and anti-depressant use (Oksanen et al. 2011). However, these and other similar studies (e.g., Mein et al. 2003) are based on particular occupational cohorts and so findings may not be transferrable to the general population. Interestingly, where there is an impact of retirement to improve health outcomes after retirement there is some evidence to suggest that this appears strongest for those in lower employment grades, or in poor work environments (e.g., high demands and low job satisfaction) and for those who are in poor health prior to retirement (Westerlund et al. 2009), however, other studies show conflicting results with improvements in particular health outcomes for those in higher occupational grades (e.g., Mein et al. 2003; Chandola et al. 2007).
There are several important methodological challenges concerning research on retirement and its influence on health. Establishing causal links is challenging because the retirement decision and health are endogenous variables; for example it is known that one route into retirement is withdrawal from economic activity due to poor health, so in this situation the observed poor health observed after retirement might be the effect not the cause of retirement (Behncke 2012). In terms of methodology, studies are split between those that followed individuals through retirement within a longitudinal design (e.g., Westerlund et al. 2009) and those that compare a group of retirees with a control group (e.g., Bound and Waidmann 2007). A key issue in terms of the studies that compare the health outcomes of retired and an employed group is the omitted variable problem; the retired and employed groups are different according to a range of characteristics, many of which, are unobservable and so it is difficult to claim a difference that is driven by retirement rather than some omitted variable. Longitudinal study designs that compare measures of health before and after retirement are thought to be more informative in determining whether the retirement process is likely to cause change in health (Oksnanen and Virtanen 2012) with such studies selected as the gold-standard by van der Heide et al. (2013) in their review of the literature on retirement and health.
In this paper we make several contributions to the literature; first we extend the body of research that has examined trajectories of health outcomes throughout retirement in particular occupational cohorts (Vahtera et al. 2009; Westerlund et al. 2009, 2010) to a sample that is representative of the general population of England. Second, we exploit the longitudinal nature of the English Longitudinal Study of Ageing (ELSA) and its maturation to include 6 waves of data to follow individuals through retirement developing the existing ELSA-based studies (Bound and Waidmann 2007; Behncke 2012). The analysis shall carefully examine not only any potential impact of retirement on self-reported illness but also the extent to which any such effect varies according to demographic, socio-economic, job/retirement characteristics and psychological factors (depression). Finally, we choose to focus on a self-reported measure of limiting long-term illness based on a question that indicates whether a person has a long-term illness that limits them in their everyday activities for three reasons. First, a body of work supports the validity of such measures of self-assessed health (Charlton et al. 1994; Bentham et al. 1995; Idler and Benyamini 1997; Mitchell 2005) with LLTI found to be most strongly associated with more serious health conditions (Manor et al. 2001) and physical limitations rather than with psychological health (Cohen et al. 1995). Second, LLTI is a useful measure in that it summarises a diverse set of health components (Rijs et al. 2012) and third, self-reported limiting long term illness provides an individual’s evaluation of their health given the conditions they are placed, an important distinction given the policy context of extending working lives.
Methods
Data and Variables
The data source used in the analysis of this paper is the English Longitudinal Study of Ageing (ELSA) a representative sample of the population aged over 50 living in private households in England. ELSA is a rich data source containing information on the socio-demographic characteristics, health, social participation, and biomarkers of older people. Methodological details on survey design and data collection are provided elsewhere (see Cheshire et al. (2012)). Importantly, the survey contains detail on the health and circumstances of older people as they plan for, experience and move into retirement. The first wave of data, collected in 2002 comprises a sample of participants from the Health Survey for England (1998, 1999 and 2001). This original sample of core members (N = 11,391) was then re-interviewed at 2 year intervals with six waves of data currently available. The survey information was collected by face-to-face interview in respondents own homes.
A subset of the ELSA sample is used in the analysis reported in this paper that contains only those people who retired between waves 2 to 6. We also included in our analysis the refreshment samples in waves 3 and wave 4 restricted to those who retired between waves 4 and 6 and 5 and 6 respectively. This gave a sample of 1,897 individuals with a selection procedure as illustrated in Fig. 1.
Self-reported long-term illness is based on two survey questions. The first asks whether an individual has any any long-term illness, disability or infirmity and then the second determines whether any long term illness, disability or infirmity reported in the previous question limits them in their everyday activities in anyway. The question defines long-term as any illness disability or infirmity that has troubled an individual over a period of time or is likely to in the future.
The timing of retirement is based on self-definition through a question on the age at which a participant retired. This question was posed to all individuals who considered themselves as retired or semi-retired. Based on age of retirement we constructed a variable that indicates time to and from retirement which varies from −10 (10 years before retirement) to 10 (10 years after retirement). We examined how risks of limiting long-term illness change in the years leading up to and after retirement. We stratified our analysis of pre and post retirement slopes in LLTI prevalence according to two sets of variables; the first set comprised characteristics of individuals including their gender, living arrangements and whether they suffered from depression. We used the Centre for Epidemiologic Studies-Depression Scale (CES-D) (Radloff 1977) to give a measure of depression based on the prevalence of depressive symptoms. We used a shortened version of the CES-D which includes 8 items and has been shown to give robust results comparable to the widely used 20-item scale and other measures of depression such as the Short Form Composite International Diagnostic Interview (Steffick 2000). We used a dichotomous depression variable for this analysis and following advice in the literature (Steffick 2000) employed a cut-point of four symptoms or more to indicate depression).
The second set of characteristics was composed of variables on work and working conditions that included occupation prestige (managerial/professional, intermediate and routine), job satisfaction, the physical demands of work and a derived variable on the ratio of work demands to rewards. We used a measure of social class based on occupation and the National Statistics socio-economic classification. This variable is intended to provide a broad indication of the social and economic circumstances of survey respondents in final year of work. We used occupational social class, rather than other indicators of socio-economic circumstances (such as income) in order to obtain comparable results to the existing body research on trajectories of the prevalence of health outcomes throughout retirement (Vahtera et al. 2009; Westerlund et al. 2009, 2010). The strong correlation between different measures of social class suggests similar findings would hold across different social class indicators. The work demands to rewards ratio is based on a range of questions on working characteristics. Two questions on work demands are linked to whether a job is physically demanding and whether a job is linked to pressure due to high workloads. There are four questions on job rewards relating to factors including support, recognition, perceptions of salary and job prospects and security. A ratio greater less than 1 indicates the rewards associated with an individual’s work exceed the demands whilst a ratio greater than one suggests that demands exceed rewards. Details on the calculation of this measure of job rewards versus demands are available on request from the authors. Unfortunately the variables on working conditions were not recorded in the first wave of ELSA. We were forced to use a different sample for analysis involving these variables as a result. Here we excluded wave 1 and included only those who were economically active in wave 2 and who retired in any of the subsequent 3 waves. Full details of the ELSA sample of retirees and the distribution of the variables at baseline (first wave observed) are given in Table 1.
Models
To model trajectories in the prevalence of self-reported long-term illness we used a repeated measures logistic regression model fitted using the generalised estimating equations method which takes account the autoregressive correlation structure (Lipsitz et al. 1994). We used a spline model with a knot at retirement and assessed whether the pre-retirement slope in LLTI odds with time to retirement differs to the post-retirement slope. We interacted our pre and post retirement slope terms with each of the variables on individual circumstances and work characteristics to evaluate whether slopes differ according to these variables. In the first set of uncontrolled models we did not include any variables other than the particular variable of interest, time to retirement and their interaction examining unadjusted trajectories of LLTI prevalence before and after retirement. Then we re-fitted a set of controlled models where we included a set of potential confounders including gender, NS-SEC, living arrangements, depression, retirement timing, economic activity, qualifications.
The base model is defined below:
Let:
- π i :
-
probability of having an LLTI for individual i, i = 1,.....1,897
- x :
-
time to retirement
- δ x :
-
1 if x > 0 and 0 otherwise (dummy variable for the post-retirement slope)
Then:
This base model was extended to explore the influence of various individual circumstances and work conditions on the level and trajectories of LLTI prevalence. A specification is provided below for the gender model (uncontrolled).
Let:
- z i :
-
1 if an individual i is a woman and 0 otherwise
Then we have the gender model (uncontrolled) as below:
Finally, this gender model (controlled) was developed to include a set of confounding variables as below.
Let:
- w isj :
-
1 if an individual is a member of the jth population group of variable s (For variable s there are js-1 dummy variables for each of the population groups discounting the reference category)
Results
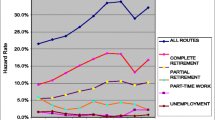
Table 2 gives the parameters estimates for the intercept, slope and post-retirement slope adjustment for each of the 8 models (first in the uncontrolled models and then in the models that control for social, demographic confounders). The table also includes a Wald test of a null hypothesis that the post retirement adjustment to the slope coefficient is equal to 0. For full model statistics see the Appendix (Tables 3 and 4). The model trajectories of LLTI prevalence (uncontrolled controlled) are given in Figs. 2, 3 and 4.
We first consider the evidence as to whether the rate of change in LLTI prevalence with time differs before and after retirement according to socio-economic and demographic variables and self-reported working conditions. The model statistics (Table 2) provide evidence of a slower increase in LLTI rates after than before retirement for all people in the base model. This difference in the slope of LLTI prevalence either side of retirement is not observed for all the variables included in our models; it is observed most strongly for those involved in routine occupations, those who were depressed or single in the final years of work or who retired at the statutory age or at younger ages. For individuals in physically demanding jobs we also observe a slower increase in LLTI rates after than before retirement; however, this difference in slope is only statistically significant (p = 0.05) after controlling for confounding variables. For the other variables (i.e., individuals in managerial or professional occupations, intermediate occupations, those not suffering from depression, living as a couple, satisfied, or not with their job or in occupations where perceived rewards exceed demands or vice versa) we observe no difference in the rate of change in LLTI prevalence on either side of retirement.
We now consider differences in the levels and slopes of LLTI trajectories across the variables on socio-economic and demographic circumstances and working conditions. The intercept term indicates that the highest levels of LLTI at retirement are observed for those who are in routine occupations, single, suffering from depression, retired on time, not satisfied with their job, or in an occupation where perceived demands exceed rewards. As might be expected the fully controlled models reveal significant interaction between these LLTI risk factors so that intercept estimates are attenuated in controlled models and in many cases are no longer statistically significant. Only depression, retiring late, not being satisfied with one’s job and being in a job where demands exceed rewards are significantly different from the reference category in the controlled models.
The pre-retirement slope in LLTI is positive indicating an increase in the risk of LLTI with time before retirement. This slope does not differ across the variables considered with the exception of the retirement timing variable where the slope of LLTI with time is steeper for individuals who retired early compared to those who retired on time (p = 0.05 in the uncontrolled model and p = 0.08 in the controlled model).
Similarly, we observed little evidence of difference in the post-retirement slope adjustment across the variables considered suggesting the rate of change in LLTI prevalence after retirement is largely consistent across socio-economic variables and working conditions, or that our analyses lack the power to detect differences. There are two exceptions to this; we observe a less steep slope in LLTI after retirement for individuals who are depressed in the final years of employment (compared to those not depressed). We observe a steeper increase in LLTI after retirement for individuals in non-physically demanding jobs compared to physically demanding jobs.
Discussion
In summary, the results of our analysis provide evidence of a less steep increase or levelling off in rates of limiting long-term illness prevalence after retirement compared to before that is most evident for those suffering from depression, who are single, who are in the lower social classes and who are in physically demanding work in the years immediately prior to retirement. We also observe a similar discrepancy between the pre-retirement and post-retirement slope for those who retire on time (age 60 for women and 65 for men) and those who retire early. We observe clear differences in levels of LLTI according to working conditions with higher rates in the least favourable working conditions, where demands exceed rewards and where job satisfaction is low but, interestingly, not according to the physical demands of work.
Several recent studies that followed a similar longitudinal design to that reported here have shown an improvement in perceived general health after retirement compared to before (Westerlund et al. 2009; van Solinge 2007; Ostberg and Samuelsson 1994). We do not show the same improvement in LLTI after retirement, but the slower increase or levelling off in LLTI rates after than before retirement taps into a similar theme of a health benefit of retirement compared to the final years of work. The small sample size and less frequent collection of data in ELSA (every 2 years compared to every year and every 6 months in the Westerlund et al. (2009) and Ostberg and Samuelsson (1994) studies) make identification of a difference in health immediately after retirement, compared to before, problematic. Whilst Bound and Waidmann (2007) employ a different methodology to that employed here they also report an improvement in self-reported health trends relative to the pre-retirement trend. Similarly the results reported here are in line with those reported by Marshall and Norman (2013) which show spatial patterns in aggregate area rates of LLTI around retirement that reflect spatial patterns of depression and occupation-based social class. Our paper adds further support to an emerging body of literature that finds evidence for improvement in self-reported measures of health and illness after retirement compared to before.
The social patterning of differences in post and pre-retirement slopes according to individual circumstances prior to retirement is slightly different from that reported in the literature where feelings of control in the retirement process (van Solinge 2007) and work conditions (Westerlund et al. 2010) are cited as the key drivers of improved health outcomes post-retirement (although we do find that slope of LLTI prevalence either side of retirement differs for those in physically demanding work). This discrepancy may reflect different contexts in different countries or the particular occupational cohort used in the Westerlund et al. (2009) study. Or it may simply reflect the difficulty in isolating the many aspects of disadvantage that feed into the effect of retirement on health that is observed; there is strong correlation between working conditions, occupation, depression and feelings of control in the retirement decision.
We argue that the social patterning in LLTI trajectories around retirement is driven by an underlying capacity of vulnerable groups to cope with the demands of work as a result of a range of factors including psychological state, the presence of a partner to offer support and the set of disadvantaged circumstances experienced by those in lower social classes (those in lower social classes earn less, have poorer underlying health and are more likely to be single and in physically demanding work for example). Clearly these aspects of disadvantage prior to retirement are related and strongly correlated. We do not claim to separate an independent impact but rather point towards a general capacity to work healthily in later life; accumulation of disadvantage across the life course means those individuals in the lower social classes have fewer resources to draw upon to continue to work and maintain good health in the final years of work and experience benefits in terms of self-reported health after they retire.
The less steep trajectory in LLTI after than before retirement also appears to differ according to timing of retirement. The difference in post and pre-retirement trajectories of LLTI prevalence is most strongly observed for those who retire early but there is also some evidence for such an effect among those who retire on time. Ideally, information on the motivation for retirement is needed to untangle this result and this was not possible here for reasons discussed in the limitations below. However, we might speculate that those who retire early may be sufficiently young for an improvement in health before the stronger underlying relationship between age and health comes into force at the older ages. And also this group, which are predominantly in the higher social classes (46 %) may have chosen to retire to pursue fulfilling (and health promoting) activities (Midanik et al. 1995; Mein et al. 2003; Mojon-Azzi et al. 2007). The majority of those who retired on time were in the routine (lower social class) occupations (46 %) and so it might be that disadvantage and the capacity to work healthily in later life underlies the retirement effect for this group. Further to this it might also be the case that those who retire on time lack the resources to choose their own retirement path and timing, a result that ties into the work on choice, retirement and health of van Solinge (2007). The finding that physically demanding work in the final years of employment might have harmful effects on self-reported illness that are alleviated in retirement support calls for policies that seek to protect older workers from aspects of work that are physically demanding where possible (Veermeer et al. 2014).
The slower increase in self-reported illness after than before retirement for certain groups has the effect of reducing post-retirement inequalities in self-reported health across divisions based on social class, marital status and mental health (depression). This is an important finding in the context of the policy to increase the statutory age of retirement. If our results are generalizable to the situation where retirement ages are delayed, then existing gaps in health status in the years after retirement are likely to become wider than currently observed. A policy intended to reduce the cost of pensions may be offset by higher costs linked to dealing with the health problems in the final years of work. Such observations are noted elsewhere in the literature (Harper et al. 2011; Veermeer et al. 2014).
The differences in levels of LLTI trajectories across socio-economic and demographic variables are largely in line with previous research. A slight discrepancy is the comparability of levels of LLTI for men and women (the intercept and slope terms for women did not attain statistical significance) given the generally poorer health of women according to other health outcomes. This may in part reflect the organisation of our dataset around time to retirement rather than age, and the younger age of retirement observed for women compared to men. However, there is also evidence to suggest only slight differences in LLTI prevalence among men and women at the older ages (McMunn et al. 2003). A further important point to note is the importance of working conditions (efforts versus rewards and job satisfaction) on LLTI independent of individual risk factors that appears to persist into retirement.
Our study is subject to a number of limitations which we now consider. First, we would have liked to have explored differences in LLTI trajectories around retirement according to the reason for retirement (voluntary or involuntary, due to ill health or redundancy) but unfortunately this variable has a large proportion of missing values and so we were not able to investigate the impact of route into retirement within our analysis. In particular, we do not explore the situation where retirement is for reasons of poor health and the effect this might have on our results. Whilst this is an important weakness of our study, the impact of retirement route on subsequent health outcomes has been investigated elsewhere; Hyde et al. (2004) investigate the impact of pre-retirement factors and retirement routes on circumstances after retirement finding that pre-retirement circumstances are more important determinants of post-retirement health and life satisfaction than retirement route.
Second, retirement is a complicated concept to operationalise and so we cannot rule out the possibility that using other definitions might influence the results we observed. One particular issue is that some individuals may classify themselves as retired but then continue to participate in employment. Although previous analysis has suggested that such activity is relatively rare with retirement tending to be permanent (Banks and Smith 2006), we do observe a number of individuals who appear to continue to work after having defined themselves as retired. We tested the sensitivity of our results to this issue by refitting our models (results not shown) to include only those who are economically active in wave 1 and who then define themselves as retired in all of the subsequent five waves. The results obtained are comparable to those reported, suggesting that our results are robust to this complication of defining retirement.
Third, our occupational measure is a crude indicator of socio-economic circumstances prior to retirement. Other variables such as income or education are likely to give similar results but could have been used to capture the influence of different components or aspects of socio-economic position on the slope of LLTI rates around retirement. Such analysis is beyond the scope of this paper but is recommended to give a nuanced picture of the impact of socio-economic circumstances on self-reported illness before and after retirement. However, at least in the case of ELSA, sample sizes would complicate such analysis.
Finally, ELSA, like other longitudinal studies is subject to attrition which has the potential to influence results if those who drop out are not a random sample. As Table 1 illustrates LLTI prevalence is particularly high in the sub-sample who have missing values for the explanatory variables investigated; for example, we observe the highest rates of LLTI in people with missing data on occupational class (NS-SEC), job satisfaction, job demands, and job effort versus rewards. It is plausible that the high levels of LLTI prevalence in this group with missing data might be driven by factors including participation in insecure employment and its detrimental impact of health (Ferrie et al. 2002) and the likelihood that suffering from an LLTI predisposes people not to answer questions in surveys. We test the sensitivity of our findings to attrition by re-fitting all the models using the longitudinal weights which are available for a subset of the sample who responded to all six waves of ELSA. We are particularly interested in the influence of the weighted analysis on the post-retirement slope adjustment for those groups with differences in pre and post retirement slopes. The results (see Appendix; Tables 6, 7 and 8) for these groups from the weighted analysis reveal a set of post-retirement slope adjustments that are in the same direction (slope adjusted downwards) as reported in previous unweighted analysis (see Appendix; Figs. 5, 6 and 7). However, the parameter estimates for the post-retirement slope adjustments are attenuated, indicating that attrition is likely to be a factor contributing to the less steep slope of LLTI after retirement, compared to before, that is observed for people who are single, in routine occupations, who retired on time, who are in physically demanding occupations and who were depressed in the final years of work. This result is plausible in that those who drop out of the survey are more likely to have an LLTI (see Table 1) and we know that drop out is highest amongst those who are depressed or in routine occupations, for example. Thus part of the slower growth in LLTI after than before retirement for the particular groups affected is likely to be a result of attrition. However, importantly, the longitudinal weights do not change the direction of slope coefficient estimates for these groups and, whilst estimates lose statistical significance, it is likely our analyses lack the power to detect significant differences as a result of the reduced sample size in the sub-sample with longitudinal weights.
Conclusion
In conclusion, our results suggest that the impact of retirement on self-reported long-term illness varies according to circumstances prior to retirement. Disadvantaged individuals appear to move to a less steep increase in LLTI prevalence after retirement compared to before, perhaps as a result of diminished capacity to cope with the demands of work in the final years of work. From a policy context it suggests that moves to a later retirement age may have the unintended consequence of exacerbating health inequality.
References
Angel, J., & Mudrazija, S. (2011). Raising the retirement age: is it fair for low-income workers and minorities. 21(2), 14–21. doi: 10.1093/ppar/21.2.14.
Atchley, R. (1976). The sociology of retirement. New York: John Wiley.
Banks, J., & Smith, S. (2006). Retirement in the UK. Oxford Review of Economic Policy, 22(1), 40–56.
Behncke, S. (2012). Does retirement trigger ill-health? Health Economics, 21, 282–300.
Bellaby, P. (2006). Can they carry on working? Later retirement, health and social inequality in an aging population. International Journal of Health Services, 36(1), 1–23.
Bentham, G., Eimermann, J., Haynes, R., Lovett, A., & Brainard, J. (1995). Limiting long-term illness and its associations with mortality and indicators of social deprivation. Journal of Epidemiology and Community Health, 49, S57–S64.
Bound, J., & Waidmann, T. (2007) Estimating the health effects of retirement. Michigan Retirement Research Center Working Paper. WP 2007–168.
Burstrom, B. (2000). Inequality in the social consequences of illness: how well do people with long-term illness fare in the British and Swedish labor markets? International Journal of Health Services, 30(3), 435–451.
Chandola, T., Ferrie, J., Sacker, A., & Marmot, M. (2007). Social inequalities in self reported health in early old age: follow up of prospective cohort study. British Medical Journal, 334, 990. doi:10.1136/bmj.39167.439792.55.
Charlton, J., Wallace, M., & White, I. (1994). Long-term illness: results from the 1991 census. Population Trends, 75, 18–25.
Cheshire, H., Hussey, D., Phelps, A., & Woods, N. (2012). Methodology. In Dynamics of Ageing: Evidence from the English Longitudinal Study of Ageing. In: Banks J, Nazroo J, Steptoe A. (Eds.), London: The Institute for Fiscal Studies. 2012; ISBN: 978-1-903274-92-7.
Cohen, G., Forbes, J., & Garraway, M. (1995). Interpreting self-reported limiting long-term illness. British Medical Journal, 311, 722–724.
Delson, L. (1996). Gradual retirement: lessons from the Nordic countries and the Netherlands. European Journal of Industrial Relations, 2(1), 55–67.
Ferrie, J., Shipley, M., Stansfield, S., & Marmot, M. (2002) Effects of chronic job insecurity and change in job security on self-reported health, minor psychiatric morbidity, physiological measures and health related behaviours in British civil servants: the Whitehall II study. Journal of Epidemiology and Community Health. 56(6). doi: 10.1136/jech.56.6.450
Ginn, J., & Arber, S. (2001). Pension prospects of minority groups: inequalities by gender and ethnicity. British Journal of Sociology, 52, 519–539.
Hamblin, K. (2010). Changes to policies for work and retirement in EU15 nations (1995–2005): an exploration of policy packages for the 50-plus cohort. International Journal of Ageing and Later Life, 5(1), 13–43.
Harper, S., Howse, K., & Baxter, S. (2011). Living longer and prospering: Designing an adequate, sustainable and equitable UK state pension system. Oxford Institute of Ageing and Club Vita.
Hillbourne, M. (1999). Living together full time? Middle-class couples approaching retirement. Ageing and Society, 19(02), 161–183.
Hyde, M., Ferrie, J., Higgs, P., Mein, G., & Nazroo, J. (2004). The effects of pre-retirement factors and retirement route on circumstances in retirement: findings from the Whitehall II study. Ageing and Society, 24, 279–296.
Idler, E., & Benyamini, Y. (1997). Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37.
Lipsitz, S. R., Kim, K., & Zhao, L. (1994). Analysis of repeated categorical data using generalized estimating equations. Statistical Medicine, 13, 1149–1163.
Manor, O., Matthews, S., & Power, C. (2001). Self-rated health and limiting longstanding illness: inter-relationships with morbidity in early adulthood. International Journal of Epidemiology, 30, 600–607.
Marshall, A., & Norman, P. (2013). Geographies of the impact of retirement on health in the United Kingdom. Health and Places, 20, 1–12.
McMunn, A., Hyde, M., Janevic, M., & Kumari, M. (2003). Chapter 6: Health. In health, wealth and lifestyles of the older population in England. In M. Marmot, J. Banks, C. Lessof, & J. Nazroo (Eds.), The 2002 English longitudinal study of ageing. London: The Institute for Fiscal Studies.
Mein, G., Martikainen, P., Hemmingway, H., Stansfeld, S., & Marmot, M. (2003). Is retirement good or bad for mental and physical health functioning? Whitehall II longitundinal study of civil servants. Journal of Epidemiological Community Health, 57, 46–49.
Midanik, L. T., Soghikian, K., Ransom, L. J., & Tekawa, I. S. (1995). The effect of retirement on mental health and health behaviors: the Kaiser permanente retirement study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 50B(1), S59–S61. doi:10.1093/geronb/50B.1.S59.
Mitchell, R. (2005). Commentary: the decline of death--how do we measure and interpret changes in self-reported health across cultures and time? International Journal of Epidemiology, 34(2), 306–308.
Mojon-Azzi, S., Souza-Poza, A., & Widmer, R. (2007). The effect of retirement on health: a panel analysis using data from the Swiss Household Panel. Swiss Medial Weekly, 137, 581–585.
Oksanen, T., Vahtera, J., Westerlund, H., Pentti, J., Sjösten, N., Virtanen, M., Kawachi, I., & Kivimäki, M. (2011). Is retirement beneficial for mental health? Antidepressant use before and after retirement. Epidemiology, 22, 553–559.
Oksnanen, T., & Virtanen, M. (2012). Health and retirement: a complex relationship. European Journal of Ageing, 9, 221–225. doi:10.1007/s10433-012-0243-7.
Ostberg, H., & Samuelsson, S. M. (1994). Occupational retirement in women due to age. Health aspects. Scandinavian Journal of Social Medicine, 22, 90–96.
Pond, R., Stephens, C., & Alpass, F. (2010). How health affects retirement decision: three pathways taken by middle-older aged New Zealanders. Population Aging, 30, 527–545.
Radloff, L. S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Reitzes, D., & Mutran, E. (2004). The transition to retirement: stages and factors that influence retirement adjustment. International Journal of Aging and Human Development, 59(1), 63–84.
Reitzes, D. C., Mutran, E. J., & Fernandez, M. E. (1996). Does retirement hurt well-being ? Factors influencing self-esteem and depression among retirees and workers. The Gerontologist, 36(5), 649–656.
Rijs, K. J., Cozijnsen, R., & Deeg, D. J. H. (2012). The effect of retirement and age at retirement on self-percieved health after three years of follow-up in Dutch 55–64 year-olds. Ageing and Society, 32(2), 281–306.
Steffick, D. (2000) HRS / AHEAD documentation report: Documentation of affective functioning measures in the health and retirement study. University of Michigan.
Vahtera, J., Westerlund, H., Hall, M., Sjosten, N., Kivimaki, M., Salo, P., Ferrie, J. E., Jokela, M., Pentti, J., Singh-Manoux, A., Goldberg, M., & Zins, M. (2009). Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep, 32(11), 1459–1466.
van der Heide, I., van Rijn, R., Robroek, S., Burdorf, A., & Proper, K. (2013). Is retirement good for your health? A systematic review of longitudinal studies. BMC Public Health, 13, 1180.
van Solinge, H. (2007). Health change in retirement: a longitudinal study among older workers in the Netherlands. Research on Aging, 29, 225–256.
Veermeer, N., Mastrogiacomo, M., & Soest, A. (2014). Demanding occupations and the retirement age in the Netherlands. De Nederlandsche Bank Working Paper. 444. Available at: http://www.dnb.nl/binaries/Working%20Paper%20448_tcm46-315229.pdf
Westerlund, H., Kiyimaki, M., Singh-Manoux, A., Melcior, M., Ferrie, J., Pentti, J., Jokela, J., Leineweber, C., Goldberg, M., Zins, M., & Vahtera, J, (2009). Self-rated health before and after retirement in France (GAZEL): a cohort study. The Lancet 374.
Westerlund, H., Vahtera, J., Ferrie, J. E., Singh-Manoux, A., Pentti, J., Melchior, M., Leineweber, C., Jokela, M., Siegriest, J., Goldberg, M., Zins, M., & Kivimäki, M. (2010). Effect of retirement on major chronic conditions and fatigue: French GAZEL occupational cohort study. BMJ, 341, c6149.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Model trajectories of self-reported limiting long term illness prevalence at retirement according to socio-economic, health and retirement circumstances ((models include socio-demographic controls: gender, occupation, living arrangements, depression, timing of retirement). Longitudinal weights included
Model trajectories of self-reported limiting long term illness prevalence at retirement according to perceived working conditions in final years of employment (controlled and uncontrolled models). Controlled models include socio-demographic controls: gender, occupation, living arrangements, depression, timing of retirement). Longitudinal weights are also included
Rights and permissions
About this article
Cite this article
Marshall, A., Nazroo, J. Trajectories in the Prevalence of Self-Reported Illness Around Retirement. Population Ageing 9, 11–48 (2016). https://doi.org/10.1007/s12062-015-9130-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12062-015-9130-2