Abstract
Prolonged ventilation remains the most common cause of tracheal stenosis. Tracheal reconstruction is the gold standard treatment in these cases. The success of surgery is based on results of the pulmonary function test (PFT) which relies on patients’ performance and their cooperation. The objective of the study was to investigate the impact of tracheal reconstruction in cases of tracheal stenosis on blood gas indices as well as airflow indices and whether arterial blood gas (ABG) can be a better surrogate of adequacy of tracheal reconstruction. This was a retrospective observational study of 61 patients with tracheal stenosis between the ages of 21 and 65 years who underwent tracheal reconstruction. The preoperative and postoperative values of various blood gas indices like partial pressure of oxygen (pO2), partial pressure of carbon dioxide (pCO2), and potential of hydrogen (pH) and airflow indices like forced expiratory volume in 1 s (FEV1) and peak expiratory flow (PEF) were evaluated and found that all the parameters showed significant improvement after tracheal reconstruction with P < 0.0001. Tracheal reconstruction resulted in improvement of oxygenation and airflow parameters which led to relief of symptoms. Hence, ABG can be used as a surrogate marker for denoting the success of the surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
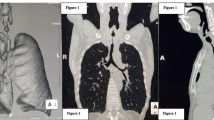
Prolonged intubation remains the most common cause of tracheal stenosis in adult population with an incidence of 6 to 21%. Other common etiological factors are malignancy, extra-tracheal compression, congenital, and traumatic [1,2,3]. The patients usually present with breathlessness, stridor, apnea, and cyanosis [4]. Confirmation is done with chest X-ray (postero-anterior, lateral views), 3-dimensional multi-planar reconstruction computerized tomography (CT), pulmonary function test (PFT), and bronchoscopy [5]. The Myer-Cotton grading of tracheal stenosis is based on the percentage of tracheal stenosis that is detectable in the CT. The medical management of tracheal stenosis involves the use of anti-inflammatory agents, prophylactic antibiotics, mucolytic agents, and chest physiotherapy. The less invasive management approaches which are generally opted for those patients who refuse an extensive surgery include bronchoscopy-guided endotracheal dilatation, tracheal stenting, laser surgery, and spray cryotherapy. These modalities help in avoiding emergency admissions, decreasing the rate of development of severe tracheal stenosis, and also in optimizing the patients for the surgical feasibility of tracheal reconstruction [6, 7]. If all the above modalities of treatment fail, tracheal resection with reconstruction is contemplated, which is the gold standard operation [8].
The success of airway patency translates into symptomatic relief of the patients with improvement in the PFT. But the results of PFT are based on patients’ understanding, performance, and their cooperation. Some of the studies show a good correlation of the spirometric measurements with the length of the stenosis and the grade of the stenosis (percentage of tracheal diameter stenosed) [9, 10]. Arterial blood gas (ABG) analysis shows the adequacy of oxygenation at the cellular level, which is not affected by patients’ performance. The present study investigated the impact of tracheal reconstruction on spirometric as well as ABG indices and whether ABG can be used as a surrogate for the adequacy of tracheal reconstruction.
Materials and methods
After obtaining institutional ethics committee permission for data sharing, a retrospective observational study between the years 2013 and 2021 was conducted. The study included 61 patients with isolated tracheal stenosis who underwent tracheal reconstruction with preoperative and postoperative potential of hydrogen (pH), partial pressure of oxygen (pO2), partial pressure of carbon dioxide (pCO2), forced expiratory volume in 1 s (FEV1), and peak expiratory flow (PEF) data available in the institutional database. All the cases were referred from the Department of Otolaryngology after 6 months of conservative and semi-invasive management yielded no permanent symptomatic relief. The tracheal reconstruction surgery was planned 3 weeks after the last dilation procedure to ensure that inflammation had subsided. Other modalities like laser therapy were not available in our institute and tracheal stenting was reserved only for patients with tracheal stenosis having external compression of the trachea by tumor mass, so those were not included in this study. Twenty-three patients were excluded (multi-level airway stenosis—1, pediatric patients—2, unable to perform spirometry—9, non-availability of data—5, bronchial asthma—1, smokers and chronic obstructive pulmonary disease (COPD), chronic obstructive airway disease—7) from the study. Bronchial asthma, COPD, and smokers who underwent tracheal reconstruction were excluded as the pO2, pCO2, and pH levels by disease pathology would have confounded the relative improvement in ABG indices after tracheal reconstruction, complicating the aim of the study.
Tracheal reconstruction was achieved by proper planning, the right selection of endotracheal tube (ET), and the precise location of the involved segment preoperatively with the help of a CT scan and direct visualization with a fiber optic bronchoscope. The average ET size that was placed was 6.0 in males and 5.5 in females with stenosis > 50%. The surgical approach was cervical in upper or middle tracheal lesions and for lower tracheal lesions a sternal split was undertaken. In tracheostomized patients, the tracheal stoma along with the stenotic part was excised. A guardian suture was placed to keep the anastomosis tension-free and immobilized.
The success of the tracheal reconstruction was defined in terms of improvement in FEV1, PEF, pO2, pCO2, and pH giving symptomatic relief with a respiratory rate < 18 per minute and minimal work of breathing. Preoperative parameters were taken 1 day before the surgery and postoperative spirometric parameters were taken on the 3rd day after surgery as the patients were pain-free and non-sedated to carry out spirometric commands. The normal spirometry is done in comfortable sitting posture without neck flexion, but in these study subjects as there was guardian stitch, the spirometry tests were performed with the flexion of the neck. The first 2 attempts were difficult for most of the patients and were suboptimal, but were performed successfully by all the study subjects as the mouth piece of the spirometer was hand-held. All the ABG data was collected on room air just before performing spirometry on the 3rd postoperative day. FEV1 and PEF less than 80% of the predicted were considered abnormal.
Statistics
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) (Armonk, NY) software, version 21. Demographic profile; the preoperative indices FEV1-1, PEF-1, pH-1, pO2-1, and pCO2-1; and postoperative indices FEV1-2, PEF-2, pH-2, pO2-2, and pCO2-2 were tested with a paired sample t-test. The level of significance was set at a P value < 0.05.
Results
There were 37 males (60.66%) and 24 females (39.34%) in the study population. The number of days of intubation ranged from 12 to 56 days with a mean of 28 days for tiding over the crisis of the primary disease which culminated into tracheal stenosis. The mean tracheal stenotic length was 37 mm and the mean excised tracheal length measured 42 mm. The mean age of presentation was 41.84 years. The percentage of stenosis ranged from 52 to 94% with a mean of 70.67% (Table 1).
On-table extubation was possible in 60 patients (98.36%) and 1 patient (1.64%) had delayed extubation due to prior history of traumatic bilateral recurrent laryngeal nerve palsy. There was 1 mortality (1.64%) in this study on the 5th postoperative day, which occurred due to sudden aspiration. Wound infection occurred in 2 patients (3.28%) and glottic dysfunction was reported in 2 patients (3.28%). The etiology of 58 cases (95.08%) in this case series of tracheal stenosis was prolonged intubation due to medical causes and 3 cases (4.92%) were polytrauma patients who needed prolonged ventilation. Sixteen patients (26.23%) with tracheal stenosis had a history of prior tracheostomy. Fifty-four patients (88.52%) were treated surgically by resection of the stenotic part followed by end-to-end anastomosis of the trachea, while 7 patients (11.47%) required an extensive tracheal resection by the same team of thoracic surgeons. The cervical approach was undertaken in most of the patients with an extension of incision as per the requirement for adequate laryngeal release, and one patient had a cervicomediastinal approach.
The preoperative and postoperative values of the study variables (pH, pO2, pCO2, PEF, FEV1) were compared and found that all the study variables showed improvement in the postoperative period, which was statistically significant (P value < 0.001) (Table 2).
Discussion
Tracheal reconstruction is one of the most challenging surgeries in thoracic surgery. The success of the surgery was assessed by symptomatic relief by the patient, which was subjective, or by a spirometric assessment, which again was dependent on many patient-related factors like consciousness, understanding of the procedure, and the feasibility of performing the procedure. The authors have therefore selected to measure preoperative and postoperative ABG indices along with the spirometric data and verified whether the improvement in spirometric data was being translated in an improvement in ABG and employed ABG as a surrogate marker for the assessment of surgical success. Improvement in oxygenation and metabolic indices, as reflected in pO2, pCO2, and pH, indicated reduced work of breathing and therefore symptomatic relief.
Both ABG and PFT showed improvement post-reconstruction in this study. Improvement in the PFTs post dilatation [11] and following stent placement [12] have been documented in the literature. Kandaswamy et al. showed that the ABG values were lower in the patients with tracheomalacia before establishing a patent airway with that of age-matched controls [13]. The present study also showed that the ABG and other indices were lower in the patients of tracheal stenosis before establishing a patent airway by surgery.
There are a few studies where airflow dynamics have been used for predicting the need for operative intervention and also for the management of idiopathic subglottic stenosis, which showed a good correlation of the spirometric data in stenotic cases [14, 15]. The present study also showed a good correlation between spirometric data and the blood gas indices data which adds strength to the fact that adequate resection and re-anastomosis give better results in cases of established tracheal stenosis refractory to conservative therapies. Hence, ABG can be used as a surrogate marker to check the adequacy of tracheal reconstruction irrespective of spirometric performance.
Limitations
The limitation of the study included patients’ variability in understanding and executing spirometric commands to perfection in spite of best and repeated explanations and demonstrations. This limitation could somewhat be minimized as ABG also showed improvement in these patients accompanied by relief of symptoms. In spite of the authors’ best efforts, long-term follow-up data could not be retrieved from the available medical records.
Conclusion
Symptomatic relief after tracheal reconstruction is a subjective phenomenon, whereas objective measurement of airflow is done by spirometry. Spirometric performance depends on varied patient-related factors, which limit its credibility as a stand-alone parameter. Irrespective of patients’ performance on spirometry, ABG can predict the success of the operation and can be used as a surrogate marker.
Abbreviations
- pO2 :
-
Partial pressure of oxygen
- pCO2 :
-
Partial pressure of carbon dioxide
- FEV1:
-
Forced expiratory volume in 1 s
- pH:
-
Potential of hydrogen
- COPD:
-
Chronic obstructive pulmonary disease
- BMI:
-
Body mass index
- ETS:
-
Excised tracheal stenosis
- CPB:
-
Cardiopulmonary bypass
- ABG:
-
Arterial blood gas
- ET:
-
Endotracheal tube
References
Farzanegan R, Farzanegan B, Zangi M, Golestani EM, Noorbakhsh S, Doozandeh TN, et al. Incidence rate of post-intubation tracheal stenosis in patients admitted to five intensive care units in Iran. Iran Red Crescent Med J. 2016;18: e37574. https://doi.org/10.5812/ircmj.37574.
Biswas A, Mehta HJ, Jantz MA. A 62-year-old woman with refractory wheezing. Chest. 2018;153:e57–62. https://doi.org/10.1016/j.chest.2017.08.019.
Nair S, Nilakantan A, Sood A, Gupta A, Gupta A. Challenges in the management of laryngeal stenosis. Indian J Otolaryngol Head Neck Surg. 2016;68:294–9. https://doi.org/10.1007/s12070-015-0936-2.
Al-Qadi MO, Artenstein AW, Braman SS. The “forgotten zone”: acquired disorders of the trachea in adults. Respir Med. 2013;107:1301–13. https://doi.org/10.1016/j.rmed.2013.03.017.
Shepard JO, Flores EJ, Abbott GF. Imaging of the trachea. Ann Cardiothorac Surg. 2018;7:197–209. https://doi.org/10.21037/acs.2018.03.09.
Fernando HC, Dekeratry D, Downie G, Finley D, Sullivan V, Sarkar S, et al. Feasibility of spray cryotherapy and balloon dilation for non-malignant strictures of the airway. Eur J Cardiothorac Surg. 2011;40:1177–80. https://doi.org/10.1016/j.ejcts.2011.02.062.
Motus IY, Konstantinova OS, Giss NA. Cicatricial tracheal stenosis. Is prevention possible? A single-region experience. Khirurgiia (Mosk). 2023;6:42–7. https://doi.org/10.17116/hirurgia202306142.
Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non- resectable tracheal stenosis. J Thorac Dis. 2014;6:258–70. https://doi.org/10.3978/j.issn.2072-1439.2013.11.08.
Alrabiah A, Almohanna S, Aljasser A, Zakzouk A, Habib SS, Almohizea M, et al. Utility of spirometry values for evaluating tracheal stenosis patients before and after balloon dilation. Ear Nose Throat J. 2022;101:NP62–NP7. https://doi.org/10.1177/0145561320936968.
Pinto J, Chambel B, Freitas C, Conceição M, Morais A, Fernandes G, et al. Spirometry as an integral part of benign tracheal stenosis management. Eur Respir J. 2020;56:2844. https://doi.org/10.1183/13993003.congress-2020.2844.
Abdullah A, Alrabiah A, Habib SS, Aljathlany Y, Aljasser A, Bukhari M, et al. The value of spirometry in subglottic stenosis. Ear Nose Throat J. 2019;98:98–101. https://doi.org/10.1177/0145561318823309.
Vergnon JM, Costes F, Bayon MC, Emonot A. Efficacy of tracheal and bronchial stent placement on respiratory functional tests. Chest. 1995;107:741–6. https://doi.org/10.1378/chest.107.3.741.
Kandaswamy C, Bird G, Gill N, Math E, Vempilly JJ. Severe tracheomalacia in the ICU: identification of diagnostic criteria and risk factor analysis from a case control study. Respir Care. 2013;58:340–7. https://doi.org/10.4187/respcare.01866.
Maresh A, Preciado DA, O’Connell AP, Zalzal GH. A comparative analysis of open surgery vs endoscopic balloon dilation for pediatric subglottic stenosis. JAMA Otolaryngol Head Neck Surg. 2014;140:901–5. https://doi.org/10.1001/jamaoto.2014.1742.
Song SA, Sandhu G, Franco RA Jr. Should we routinely use pulmonary function testing in the management of subglottic stenosis? Laryngoscope. 2021;131:245–7. https://doi.org/10.1002/lary.28678.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical committee approval
Obtained.
Informed consent
Taken.
Human and/or animal rights statement
Not applicable as no experimental technique was used.
Conflict of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghosh, K., Kar, S.K. & Dammalapati, P.K. Analysis of preoperative and postoperative blood gas indices and airflow dynamics with tracheal stenosis undergoing tracheal reconstruction. Indian J Thorac Cardiovasc Surg 40, 440–443 (2024). https://doi.org/10.1007/s12055-024-01694-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-024-01694-w