Abstract
Pyopericardium is rare in the modern antibiotic era but is still infrequently seen in the setting of immunosuppression, recent thoracic surgery and sepsis. Although classically an extension of a thoracic gram-positive bacterial infection, gram-negative bacterial purulent pericarditis may be encountered in the setting of nosocomial infections. Emergent pericardial drainage allows for prompt definitive management and planning for further intervention. Early surgery should be the priority after a failed retrieval of the catheter. Appropriate surgical methods should be employed to minimize complications associated with stuck catheters. We report a case of pyopericardium secondary to a clinically silent lung abscess in an immunocompetent 49-year-old patient. This was treated by standard pericardial drainage via a pigtail catheter. Multiple failed attempts in removal warranted a surgical approach to remove the coiled catheter. The catheter was found to be coiled around the heart with presence of clots in the pericardium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pyopericardium is a rare entity nowadays, due to the widespread use of antibiotics, but is still infrequently seen in the setting of immunosuppression, recent thoracic surgery and sepsis. Classically an extension of a thoracic gram-positive bacterial infection, gram-negative bacterial presence is often associated with nosocomial infections. The standard of care for evacuating a pericardial effusion is pericardial drainage via a pigtail catheter. In extraordinary circumstances, rare complications such as a stuck pericardial catheter warrant further management. We describe a unique presentation of a stuck pericardial pigtail catheter which was successfully retrieved through surgical intervention. The presence of a community acquired Klebsiella pneumoniae pyo-hemo-pericardium as the initial presentation of a clinically silent lung abscess in an immunocompetent patient represents an overlapping series of rare circumstances.
Case report
A 49-year-old woman without comorbidities presented to the emergency with a 10-day history of diffuse progressive chest discomfort and a 2-day history of progressive exertional dyspnea. On examination, a pericardial friction rub was heard with the remaining of the physical examination being insignificant. Electrocardiogram (ECG) revealed diffuse ST elevation and chest X-ray showed cardiomegaly. Echocardiography revealed a moderate to severe pericardial effusion with inferior vena cava (IVC) congestion and early diastolic collapse, confirming cardiac tamponade. Ceftriaxone and azithromycin were administered.
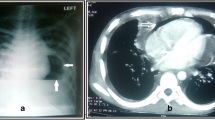
Pericardiocentesis and drainage were performed using a 14 Fr indwelling pigtail catheter under echocardiographic guidance, yielding 600 ml of purulent fluid with blood clots. Microscopy revealed few gram-negative bacteria with numerous pus cells in a background of macrophages and hemorrhage, while culture did not yield specific growth. Pericardial fluid analysis was consistent with a hemorrhagic purulent effusion. Removal of the pigtail catheter was attempted on three independent occasions: blindly, under fluoroscopic guidance (Fig. 1), and after intrapericardial hydrocortisone and fibrinolytic administration. However, the drain could not be retrieved, which warranted a cardiothoracic referral. Retrieval was initially attempted surgically under local anesthesia through a sub-xiphoid incision but was abandoned due to catheter recoiling. A left anterolateral thoracotomy was attempted on the seventh-day post-insertion of drain followed by pericardiotomy, which yielded blood clots with the pigtail catheter coiled circumferentially around the heart, adherent to the pericardium (Fig. 2). The clots were cleaned and the pigtail was removed followed by pericardiectomy and insertion of intercostal drains. Warm betadine saline wash was given followed by hemostasis and closure of the thoracotomy in layers. Incidentally, a lung abscess cavity with necrotic material and pus was found communicating with the pericardial sac in its posterolateral aspect. The pericardium was excised and the abscess cavity was opened into the pleura (Fig. 3). The culture of the tissue sample revealed moderate growth of multidrug resistant (MDR) Klebsiella pneumoniae resistant to aminopenicillins, cotrimoxazole, and ceftriaxone/cefuroxime, but sensitive to amikacin and cefoperazone/sulbactam necessitating a change in the patient’s antibiotic regimen to the same. The patient was asymptomatic and discharged on fifth post operative day.
Discussion
Pyopericardium is a rare pathology in the contemporary clinical setting due to the widespread use of antibiotics. In the pre-antibiotic era, 75% of patients presented as a complication of an intrathoracic focus of infection, as opposed to only 20–25% of patients in the modern era. Other significant sources include hematogenous spread, recent thoracic trauma, and other infections of the heart [1]. In addition, the disease has a high propensity to progress to complications like cardiac tamponade, constrictive pericarditis, and mycotic aneurysms in the setting of nonspecific symptoms due to delayed clinical attention [2, 3]. Pericardial effusions resulting in cardiac tamponade are often due to malignancy, tuberculosis, or an acute pyogenic infection [4]. Staphylococcus aureus is the most common cause of pyopericardium in adults and children. Gram-negative bacteria like Klebsiella pneumoniae are rarely encountered in the setting of community acquired infections in immunocompetent patients. In addition, cases of purulent pericarditis that present antemortem in immunocompetent patients tend to be associated with drug-resistant, hypervirulent microorganisms, as sensitive bugs have been selected out due to irresponsible overuse of antibiotics [2]. Moreover, tuberculosis should be ruled out first in endemic countries, as it is the most common cause of subacute and chronic purulent pericarditis, especially in areas endemic for Human Immunodeficiency Virus (HIV) as well.
Pericardiocentesis is the immediate treatment for cardiac tamponade, especially if the patient is unstable. In our case, drainage of purulent fluid warranted gram stain and culture of the fluid which was inconclusive. In about 50–60% of cases of purulent pericarditis, cultures remain sterile due to early empirical antimicrobial therapy, as with our patient [5]. Drainage of purulent fluid with blood clots warranted a percutaneous pigtail catheter insertion into the pericardium. Traditionally, pericardiocentesis is performed via a subxiphoid pericardiostomy under fluoroscopic guidance. However, the disadvantages of this approach include right ventricle and liver injury. Other methods include parasternal and apical approaches.
Complications of pericardial drains are rare at about 1.2 to 1.6% [6]. Pericardial drainage can lead to infrequent complications like pleuropericardial shunts, mediastinal hematomas, development of transient Atrio-ventricular (AV) blocks, and septic complications such as mycotic aneurysms [7]. Few authors have reported case reports with withdrawal failure reporting possible reasons like knot formation, looping around the heart, catheter breakage, and intrapericardial greater vessel strangulation [6]. Multiple attempts at catheter withdrawal may be futile with an indwelling pericardial catheter in patients with pyopericardium with clots due to the formation of dense adhesions, increasing the risk for potential cardiac damage. Early surgical intervention should be performed if the general condition of the patient permits to avoid cardiac injury, with the additional benefit of preventing recurrences, inadequate drainage, and subsequent constrictive pericarditis seen with severe cases of purulent pericarditis. Various surgical methods have been reported by authors for the extraction of difficult indwelling pericardial catheters. Wu et al. reported effective retrieval of the pigtail catheter by dilating the tract allowing for smooth removal [8]. Chuang et al. had successfully removed a circumferential pigtail knot around the heart via a mini-thoracotomy [9]. Video-assisted thoracic surgery (VATS) and thoracoscopic pericardial windows (TPW) have been newer methods of draining pericardial effusions, as they have been reported to have less post-operative complications and shorter hospital stays [10]. TPW should be only considered in patients with recurrent pericardial effusions with a background of inflammatory disease. TPW has a better visualization of the pericardium and lower risk of myocardial perforation [10].
Conclusion
Purulent pericarditis is a rare complication in the modern healthcare setting with the widespread utility of antibiotics. Stuck catheter is a potential complication of an indwelling pericardial catheter in the setting of pyo-hemo-pericardium. Physicians should refrain from multiple attempts at catheter withdrawal to avoid cardiac injury and should opt for early surgical intervention.
References
Farhat-Sabet A, Hull R, Thomas D. Cardiac tamponade from purulent pericarditis due to Cutibacterium acnes. Case Rep Cardiol. 2018;2018:4739830. https://doi.org/10.1155/2018/4739830.
Cronier P, Eugène B, Passefort S, Gryman R. A pneumococcal purulent pericarditis revealing a pneumonia and complicated by an acute cardiac tamponade. J Cardiol Cases. 2011;5:e61–4. https://doi.org/10.1016/j.jccase.2011.09.010.
Abdelnabi M, Almaghraby A, Saleh Y, El Sayed A, Rizk J. Acute purulent pericarditis treated conservatively with intrapericardial fibrinolysis and intrapericardial and systemic antibiotics. Proc (Bayl Univ Med Cent). 2021;34:498–9. https://doi.org/10.1080/08998280.2021.1889297.
Bhattarai M, Yost G, Good CW, White CF, Nepal H. Primary purulent pericarditis with cardiac tamponade due to oropharyngeal polymicrobial infection: a case report and literature review. Korean J Thorac Cardiovasc Surg. 2014;47:155–9. https://doi.org/10.5090/kjtcs.2014.47.2.155.
Petcu CP, Dilof R, Bătăiosu C, Petcu PD. Purulent pericardial effusions with pericardial tamponade - diagnosis and treatment issues. Curr Health Sci J. 2013;39:53–6.
Kraus MB, Spitznagel RA, Kugler JA. Cardiovascular collapse with attempted pericardial drain withdrawal. Ann Pediatr Cardiol. 2016;9:241–3.
Maggiolini S, Gentile G, Farina A, et al. Safety, efficacy, and complications of pericardiocentesis by real-time echo-monitored procedure. Am J Cardiol. 2016;117:1369–74. https://doi.org/10.1016/j.amjcard.2016.01.043.
Wu S-G, Shih J-Y. Pericardial pigtail knotting. Eur J Cardiothorac Surg. 2011;39:790. https://doi.org/10.1016/j.ejcts.2010.08.041.
Chuang W-P, Chiu K-M. Pigtail slip-knot catches the heart. Catheter Cardiovasc Interv. 2007;70:824–5. https://doi.org/10.1002/ccd.21228.
Sakanoue I, Hamakawa H, Okubo Y, et al. Efficacy and safety of thoracoscopic pericardial window in patients with pericardial effusions: a single-center case series. J Cardiothorac Surg. 2016;11:92. https://doi.org/10.1186/s13019-016-0488-x.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Akhilesh Gonuguntla, Anila Vasireddy, and Aadithiyavikram Venkatesan. The first draft of the manuscript was written by Akhilesh Gonuguntla and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the ethics committee of Kasturba Medical College.
Consent to participate
Informed consent was given by the patient for publication of their medical information and images. Informed consent form can be found as a supplementary document.
Conflict of interest
All authors disclose that they have no conflicts of interest.
Statement of human and animal rights
No animals were part of this case report. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Ethics approval form can be found as a supplementary document.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonuguntla, A., Vasireddy, A., Venkatesan, A. et al. Stuck pericardial pigtail catheter in purulent pericarditis: early surgery?. Indian J Thorac Cardiovasc Surg 39, 60–63 (2023). https://doi.org/10.1007/s12055-022-01417-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-022-01417-z