Abstract
Background
Emergency resuscitative thoracotomy (RT) is a recognised method of controlling non-compressible torso haemorrhage (NCTH) often in adjunct to emergency surgery. Recently, there is much debate regarding resuscitative endovascular balloon occlusion of aorta (REBOA) on its role in civilian trauma cases in controlling NCTH. This study aims to provide an updated review on in-hospital mortality rates in patients who underwent REBOA versus RT and standard care without REBOA (non-REBOA) and to identify the potential indicators of REBOA survival.
Methods
Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were used to perform the study. All adult trauma cases were included, while pre-hospital, military and non-English studies were excluded. A literature search was done on studies from 01 January 2005 to 30 June 2020 using EMBASE, MEDLINE and COCHRANE databases. Risk of bias was assessed using the Methodological Index for Non-Randomised Studies (MINORS) tool. Meta-analysis was conducted using a random effects model and the DerSimonian and Laird estimation method. A significance level of p < 0.05 was used.
Results
Twenty-five studies were included in this study. The odds of in-hospital mortality of patients who underwent REBOA compared to RT was 0.18 (p < 0.01, 0.12–0.26). The odds of in-hospital survival of patients who underwent REBOA compared to non-REBOA was 1.28 (p = 0.62, 0.46–3.53). There was a significant difference found between survivors and non-survivors in terms of their pre-REBOA systolic blood pressure (SBP) (19.26 mmHg, p < 0.01), post-REBOA SBP (20.73 mmHg, p < 0.01), duration of aortic occlusion (− 40.57 min, p < 0.01) and injury severity score (− 8.50, p < 0.01).
Conclusions
REBOA has a potential for wider application in civilian settings, with our study demonstrating lower in-hospital mortality compared to RT. Prospective multi-centre studies are needed for further evaluation of the indications and feasibility of REBOA.
Level of Evidence + Study Type: Level IV. Systematic review with meta-analysis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Haemorrhage is the leading potentially survivable cause of death in trauma patients. Non-compressible torso haemorrhage (NCTH) remains a major difficulty accounting for 60–70% of preventable deaths [1]. It can occur due to solid organ damage from blunt trauma or injury to axial vasculature from penetrating injuries. An inability to directly stem the bleeding means that a large proportion of deaths occur before definitive haemorrhage control can be obtained in hospital [2].
Emergency resuscitative thoracotomy (RT) is a recognised method of controlling NCTH often in adjunct to emergency surgery. The aorta is clamped proximal to the injury site in the hopes of occluding blood flow and stabilising the blood volume loss [3].
Resuscitative endovascular balloon occlusion of aorta (REBOA) was first described in a 1954 case series during the Korean War. The technique involves the insertion of a balloon catheter via the femoral artery into the aorta. Inflation of the balloon for occlusion is then done either in zone 1—between the left subclavian artery and the coeliac trunk, for abdominal haemorrhage or Zone 3—between the lowest renal artery and the aortic bifurcation, for pelvic or lower limb haemorrhage. Variation in technique can occur through choice of sheath size, use of imaging, balloon inflation pressure and time of occlusion [4]. While the indication of applying REBOA differs slightly to RT, they both serve to achieve haemodynamic stability.
There are currently many challenges to implementing REBOA in civilian settings. Firstly, there is no clear protocol on how to fully optimise its use. Complications after REBOA use are not frequently reported. Comparative studies on the effects of REBOA and other methods of resuscitation are also lacking. Finally, to our knowledge, the potential physiological and resuscitative indicators of survival after REBOA use have yet to be studied.
This systematic review and meta-analysis was designed to address the matters discussed above. The key aims are to provide an up-to-date review on in-hospital mortality rates in patients who underwent REBOA versus RT and standard care without REBOA (non-REBOA) and to identify potential indicators of REBOA survival.
Methods
Cochrane [5] and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [6] guidelines were used to perform the systematic review and meta-analysis (supplemental digital content (SDC) 1. table, PRISMA checklist). Our primary PICO (population, intervention, comparator, outcome) strategy was as follows:
-
Population: adults with NCTH following blunt and penetrating injuries
-
Intervention: REBOA
-
Comparator: RT and non-REBOA
-
Outcome: in-hospital mortality/survival
On top of comparing in-hospital mortality/survival between REBOA with RT and non-REBOA, we also aimed to identify indicators for survival.
Inclusion and exclusion criteria
All adult trauma cases (age ≥ 18 years) were included. Studies focussing on pre-hospital use of REBOA were not included as the time to aortic occlusion and duration of occlusion could impact the survival outcomes. Studies which utilised data from the same trauma registries (Japan Trauma Data Bank (JTDB) and American Association for the Surgery of Trauma Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AAST-AORTA) registry)) with overlapping study periods were excluded. Also, for the purpose of focussing on civilian injuries, all military data were excluded. Articles not written in English were excluded from the full-text review, along with animal model studies and human cadaver studies.
Search methods
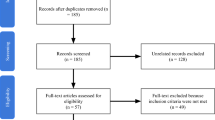
A systematic literature search on studies from 01 January 2005 to 30 June 2020 was carried out using EMBASE, MEDLINE and COCHRANE databases (Fig. 1). Key words such as “REBOA”, “Occlusion of Aorta”, “Trauma”, “Blunt Trauma” and “Penetrating Trauma” were used to execute the search. Combinations of keywords “REBOA AND Blunt Trauma”/ “REBOA AND Penetrating Trauma” were also used (SDC 2. text, search algorithm). All papers were reviewed for relevance in the titles first, and then, a full-text review was undertaken.
Study selection and data collection
Studies were examined and selected by two independent reviewers (HJK, HFK). The title and abstract were screened first. Those that appeared relevant were selected for full-text review. Papers that met the inclusion criteria through mutual consent of the reviewers were then included in the study.
The number of cases and study type were identified for each of the studies included in the analysis. Demographic data such as mean age and male to female ratio were recorded. The mechanisms of injury (penetrating or blunt) and survival rate of the procedure were also noted. Physiological markers such as the systolic blood pressure (SBP) before and after the procedure, heart rate, trauma severity (Injury Severity Score (ISS)), Glasgow Coma Scale (GCS) and resuscitative measures such as time to occlusion, aortic occlusion time and total red blood cell (RBC) transfused were collected to analyse how they influenced survival.
Risk of bias assessment
Studies that were included for statistical analysis were assessed for their internal validity based on the Methodological Index for Non-Randomised Studies (MINORS) tool [7]. Since the studies collected in our review were retrospective case series, we modified the MINORS tool so that items relating to prospective studies were not included. The scoring system was as follows: 0 (red—not reported, high risk of bias), 1 (yellow—reported but inadequate, unclear risk of bias) and 2 (green—reported, low risk of bias). Each study was assessed independently by two reviewers (HJK, HFK).
Statistical analysis
REBOA vs. RT/non-REBOA
Meta-analyses were performed to assess the effect of REBOA on mortality and survival compared to RT and non-REBOA respectively.
Adjusted odds ratio (ORs) and confidence intervals (CIs) were extracted as available. If only raw values were presented, ORs and CIs were calculated using MedCalc [8]. Adjusted and unadjusted ORs were pooled using a random effects model and the generic inverse-variance DerSimonian and Laird estimation method. The results were presented in two forest plots showing the estimated overall ORs of the included studies with a 95% CI. A heterogeneity test was performed using the I2 test, where I2 < 25%, I2 = 25–75% and I2 > 75% corresponded to low, medium and high heterogeneity respectively. Heterogeneity was explored using sub-group analyses of number of centres included and further meta-regression was performed on quality assessment scores and number of years studied. A jackknife sensitivity analysis was also performed through multiple repetitions of the analysis with systematic removal of a single study from the baseline group of studies.
Publication bias and small-study effect were evaluated with funnel plots and symmetry was calculated using Egger’s regression test. Contour funnel plots were also produced to aid differentiation of asymmetry due to publication bias from other factors.
REBOA: survivors vs. non-survivors
Some studies only looked at parameters of patients who underwent REBOA without another comparator. Meta-analyses were performed on various parameters (pre- and post-REBOA SBP, time to occlusion, duration of occlusion, ISS, GCS and RBC transfusion) to compare the difference between survivors and non-survivors. Means and standard deviations were extracted from the papers and analysed with the same model as described above.
A significance level of 0.05 was used for all tests. All statistical analyses were performed on RevMan 5 [9] and STATA® 16 [10].
Results
A total of 661 papers were screened after removing duplicates. Twenty-five studies were eligible for analysis in this review, of which 15 studies were included for quantitative analysis (Fig. 1). Three of the studies were used for meta-analysis to compare in-hospital mortality between REBOA and RT. Four were included to compare REBOA and non-REBOA. Finally, 11 studies were used to compare physiological parameters of REBOA survivors and non-survivors.
Risk of bias
A summary of the risk of bias is shown in Table 1. Most of the bias seen from the included studies are in the “baseline equivalence of groups” section as all the studies were non-randomised. Many studies have attempted to mitigate this by matching the 2 groups—this was not reported or done by Moore et al. [11].
Comparison of REBOA vs. RT (in-hospital mortality)
Three studies [11,12,13] were included in the meta-analysis comparing REBOA and RT. There were a total of 718 and 594 REBOA and RT cases respectively. The male to female ratio was 2.07 for REBOA and 3.28 for RT. Regarding the type of injury, blunt and penetrating injury accounted for 93.2% and 6.8% of the REBOA cases respectively and 72.4% and 27.6% of the RT cases respectively. The average ISS was 37.3 for REBOA and 42.2 for RT.
Meta-analysis
The primary outcome measured in all studies was in-hospital mortality. The meta-analysis of the adjusted and unadjusted odds ratios found that the odds of in-hospital mortality of patients who underwent REBOA compared to RT was 0.18, and this was significantly lower (p < 0.01, 95% CI 0.12–0.26) (Fig. 2). The heterogeneity was low with an I2 of 0%.
Exploration of heterogeneity
Heterogeneity between studies was low as mentioned above and sub-group analyses also showed differences between sub-groups were insignificant (SDC 3a,b,c. graphs, exploration of heterogeneity REBOA vs. RT). Meta-regression performed on quality assessment scores (p = 0.82) and years studied (p = 0.68) found no significant relationship between in-hospital mortality and the two co-variates (SDC 3d,e. graphs, meta-regression on quality assessment scores and years studied). The jackknife analysis showed that the overall OR remained significant, with point estimates ranging from 0.17 to 0.21 with corresponding 95% CIs < 1 in all.
Publication bias
A funnel plot displayed asymmetry which was confirmed through the Egger test (p = 0.64) suggesting possible small-study effects (Fig. 3).
Comparison of REBOA vs. non-REBOA (in-hospital survival)
Four studies [14,15,16,17] were included in the meta-analysis comparing REBOA and non-REBOA. There were a total of 300 and 806 REBOA and non-REBOA cases respectively. The male to female ratio was 2.70 for REBOA and 3.36 for non-REBOA. Mean age was 46.4 for REBOA and 39.8 for non-REBOA. Regarding the type of injury, blunt and penetrating injury accounted for 85.4% and 14.6% of the REBOA cases respectively and 55.5% and 44.5% of the non-REBOA cases respectively. The average ISS was 32.1 for REBOA and 29.0 for non-REBOA.
Meta-analysis
In-hospital survival was used here as some studies had reported this as the primary outcome measure and performed adjustments on this measure instead of in-hospital mortality. The meta-analysis of the adjusted odds ratios found that the odds of in-hospital survival of patients who underwent REBOA compared to non-REBOA was 1.28, but this was not significant (p = 0.62, 95% CI 0.46–3.53) (Fig. 4). The heterogeneity was high with an I2 of 85.84%.
Exploration of heterogeneity
Sub-group analyses were performed with stratification based on number of centres included (p = 0.34, I2 = 93.50% and 62.20%) which was insignificant and had a high sub-group heterogeneity (SDC 4a,b. graphs, exploration of heterogeneity REBOA vs. non-REBOA). Meta-regression performed on quality assessment scores (p = 0.10) and years studied (p = 0.19) found no significant relationship between in-hospital survival and the two co-variates (SDC 4c,d. graphs, meta-regression on quality assessment scores and years studied). The jackknife analysis produced OR point estimates between 0.93 and 1.79, with none of the results being significant.
Publication bias
A funnel plot displayed asymmetry which was confirmed through the Egger test (p = 0.11). A contour funnel plot appeared to have some studies missing in areas of statistical non-significance, making it likely that some of the asymmetry is due to publication bias with some degree of small-study effects (Fig. 5).
Comparison of survivors and non-survivors of REBOA
Eleven studies [15, 17,18,19,20,21,22,23,24,25,26] reported differences in characteristics of patients who survived and did not survive REBOA (Table 2). There was a significant difference found between survivors and non-survivors in terms of their pre-REBOA SBP (19.26 mmHg, p < 0.01), post-REBOA SBP (20.73 mmHg, p < 0.01), duration of aortic occlusion (− 40.57 min, p < 0.01) and ISS (− 8.50, p < 0.01). While the amount of change in SBP between survivors and non-survivors was insignificant (p = 0.90), the change between pre-REBOA and post-REBOA SBPs in both the survivor and non-survivor groups was significant (35.69 mmHg and 34.72 mmHg, both p < 0.01). Insignificant differences were found for time to occlusion (8.98 min, p = 0.42), GCS (− 1.90, p = 0.74) and amount of transfused RBC (− 2.60 units, p = 0.48).
Discussion
Our study aimed to provide a current review on how REBOA compares to current available techniques of resuscitation for non-compressible torso haemorrhage and its outcomes. Further statistical analysis was also performed to identify potential indicators of REBOA survival.
We have found that REBOA has potential benefits compared to RT. In-hospital mortality was significantly lower in patients who underwent REBOA compared to RT with low heterogeneity between the studies. However, the difference in survival advantage of REBOA over RT could be attributed to the difference in patient demographics. As shown previously, only 6.8% of REBOA cases were penetrating whereas for RT 26.7% were penetrating. The average ISS was also higher in patients receiving RT than REBOA suggesting RT was utilised in a more severely injured patient group. Other parameters, such as SBP, GCS and prior cardio-pulmonary resuscitation (CPR), were unfortunately not reported by all papers. The clinical indications of the procedures also tend to differ—RT is generally utilised in cardiac arrests with the best outcomes in penetrating isolated chest traumas whereas REBOA is used in non-penetrating abdominal trauma [11, 13].
Regarding the survival outcomes between patients who underwent REBOA and non-REBOA, we have found that the odds of survival for REBOA was higher but this was insignificant. The heterogeneity between the studies was also high—suggesting that non-REBOA encompasses a diverse group of interventions. Further details on the non-REBOA standard of care were not elaborated on in the papers and it is likely that there was a degree of variation in the trauma protocol between hospitals, thereby making a direct comparison to REBOA difficult.
Currently, there is a consensus that a clear indication and protocol for REBOA use is lacking. Single-centre studies have reported different indications with generic ones such as non-compressible torso trauma with impending cardiac arrest [18], while others used physiological measures such as refractory shock with SBP < 90 mmHg and base deficit > 5 from arterial blood gas analysis [19, 27].
The first aspect to address in the standardised use of REBOA would be optimal patient selection. This would encompass patient demographics such as age, type of injury (blunt or penetrating) and severity of injury. While many of our included studies looked at these parameters, they have been inconsistently reported and their epidemiological nature has made it difficult to draw useful inferences for clinical practice. Also, a suitable surrogate measure of severity of injury needs to be identified. Studies have used physiological markers such as vitals and GCS, biochemical markers such as lactate, and anatomical scoring systems such as ISS. Of note is Barnard et al.’s comment that anatomical scores are rarely available to clinicians at point of care and would not be a relevant clinical consideration [28].
The second aspect to address is a detailed guideline for REBOA application. The stage at which REBOA should be initiated remains a key question. Inoue et al. who analysed JTDB data reported that the use of REBOA varied between centres from prophylactic before-shock use to damage-control use [29]. Joseph et al. also noted that decisions were driven by surgeon experience [15]. Various authors have advocated for the early use of REBOA [29, 30]. There is even a suggestion of a door-to-primary surgery time limit of 60 min as significant differences in mortality were observed [29]. Maximum duration of aortic occlusion to prevent ischaemic damage is also unclear, with Irahara et al. suggesting 45 min [20] and Brenner et al. suggesting 60 min [31]. Technical aspects such as sheath size and imaging methods also vary greatly. In the United States (USA), 11–14 Fr sheaths are used while in Japan 7–10 Fr sheaths are used [21]. Imaging use ranges from that of ultrasound, portable X-rays to simply blind insertion [4, 18, 22, 23]. Finally, the specialty and type of training required differ between centres. At this point, it is worth observing that there are important dissimilarities in the usage of REBOA between Japan and the USA. Japanese studies form a significant proportion of our included studies due to their widespread use of REBOA. The low rate of trauma in Japan means that most centres do not have in-house trauma surgery support and emergency physicians perform REBOA as stop-gap measures [23, 32]. In contrast, REBOA is commonly performed by trauma or vascular surgeons in the USA [23, 33]. The training also differs in the two countries. Norii et al. reported that it is a requirement to have 3 REBOA experiences to qualify as an emergency physician [32]. In the USA, surgeons commonly already possess the relevant skill set but most would have taken up additional courses such as the Endovascular Skills for Trauma and Resuscitative Surgery (ESTARS) [33].
While it has been difficult to make inferences on indicators for REBOA use based on the literature, our analysis of differences in patient characteristics between survivors and non-survivors of REBOA might shed some light on prognostic markers of REBOA outcomes. As there was a statistically significant change in SBP brought about by REBOA in both the survivor and non-survivor groups, it can be said that REBOA is able to achieve temporary haemostasis. Moore et al. concurred on this, reporting fewer earlier deaths from haemorrhage with the majority of REBOA deaths in intensive care units while RT deaths were in the emergency department [11]. A significantly lower pre- and post-REBOA SBPs in non-survivors suggest that it is not that REBOA was unable to raise the SBP in non-survivors, but that they had started off with a lower SBP to begin with and were unable to achieve a minimum SBP required for end-organ perfusion. A significantly higher ISS in non-survivors suggests patients more severely injured were unlikely to survive despite REBOA. Lastly, a significantly longer duration of occlusion in non-survivors suggests that speed of shock reversal is also an important factor. These parameters could be possible early indicators of treatment outcomes and are worth further evaluation in future studies.
Going forward, several aspects of REBOA can be further investigated to better understand the outcomes and complications of the procedure. Various studies have suggested investigating the effects of the zone of occlusion on the perfusion of end organs [12, 19, 31]. It was also suggested that the total duration of patient hypotension, inclusive of that after REBOA insertion, should be accounted for, as a longer duration of shock may predict mortality [34]. Details on variations in procedure, such as the use of partial aortic occlusion as a graded protocol currently used in Japan, should also be included in future studies. With the improvement of REBOA technique, patient survival will theoretically increase; hence, a longer follow-up period of patients will be required to assess its long-term complications and effect on patient’s quality of life.
Limitations
Due to the ethical challenges of randomising patients to REBOA as well as its infrequent use, all studies to date have been done as retrospective case series. These are especially prone to selection bias and the descriptive nature makes it difficult to assess cause-effect relationships. Mitigation of confounding factors was done by using adjusted data for analysis—however, not all the studies presented these as demonstrated in our risk of bias assessment. The intervention was also not a standardised one, as there was consensus across studies about the lack of protocol on indications and application of REBOA [15, 16, 35]. In addition, the retrospective nature meant many studies reported issues with missing data and subjective recall of information [36]. For example, ISS were not calculated if a patient died in the emergency department, as complete imaging and exploration required were usually not performed [11]. Lastly, the small number of studies done reduces the statistical power of analyses done. As such, these factors cast doubt on the validity of pooled results.
The choice of a useful comparator for REBOA poses another problem. As mentioned above, REBOA and RT differ in their usage. Comparing non-REBOA with REBOA was also challenging as it would encompass both a wide range of patient characteristics with differing injury severity and alternative resuscitative measures, e.g. pelvic binders and vasopressors [12].
While we recognise the lack of high-quality studies at present, a meta-analysis was still performed in hope to increase the power of the statistical analysis. As we have demonstrated a possible survival benefit of REBOA, there is value in conducting future studies on this topic. Attempts should be made to design these with clinically relevant control groups while addressing ethical difficulties.
Conclusion
REBOA has a potential for wider application in civilian settings, with our study demonstrating lower in-hospital mortality compared to RT. The implementation of a protocol for REBOA use will require prospective collection of data on the indications, methods, and immediate and long-term outcomes of the procedure. Hopefully, ongoing clinical trials such as United Kingdom (UK) REBOA, Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) and Diagnostic and Interventional Radiology in Emergency, Critical care and Trauma-Intra-Aortic Balloon Occlusion (DIRECT-IABO) [37,38,39] will be able to shed light on how to effectively utilise REBOA.
References
Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006;60:S3–11. https://doi.org/10.1097/01.ta.0000199961.02677.19.
Davenport R. Haemorrhage control of the pre-hospital trauma patient. Scand J Trauma Resusc Emerg Med. 2014;22:A4. https://doi.org/10.1186/1757-7241-22-S1-A4.
Søreide K, Petrone P, Asensio JA. Emergency thoracotomy in trauma: rationale, risks, and realities. Scand J Surg. 2007;96:4–10. https://doi.org/10.1177/145749690709600102.
Brenner ML, Moore LJ, DuBose JJ, et al. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg. 2013;75:506–11. https://doi.org/10.1097/TA.0b013e31829e5416.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Cochrane 2019. Available from: www.training.cochrane.org/handbook.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6. https://doi.org/10.1046/j.1445-2197.2003.02748.x.
MedCalc. Odds ratio calculator. Available from: https://www.medcalc.org/calc/odds_ratio.php.
Review Manager (RevMan). 5.3 ed. Copenhagen: The Nordic Cochrane Centre: The Cochrane Collaboration; 2014.
StataCorp. Stata Statistical Software: Release 16. College Station: TX: StataCorp LLC; 2019.
Moore LJ, Brenner M, Kozar RA, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015;79:523–30. https://doi.org/10.1097/TA.0000000000000809.
Brenner M, Inaba K, Aiolfi A, et al. Resuscitative endovascular balloon occlusion of the aorta and resuscitative thoracotomy in select patients with hemorrhagic shock: early results from the American Association for the Surgery of Trauma's Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg. 2018;226:730–40. https://doi.org/10.1016/j.jamcollsurg.2018.01.044.
Matsumoto S, Hayashida K, Akashi T, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) for severe torso trauma in Japan: A descriptive study. World J Surg. 2019;43:1700–7. https://doi.org/10.1007/s00268-019-04968-2.
Otsuka H, Sato T, Sakurai K, et al. Effect of resuscitative endovascular balloon occlusion of the aorta in hemodynamically unstable patients with multiple severe torso trauma: a retrospective study. World J Emerg Surg. 2018;13:49. https://doi.org/10.1186/s13017-018-0210-5.
Joseph B, Zeeshan M, Sakran JV, et al. Nationwide analysis of resuscitative endovascular balloon occlusion of the aorta in civilian trauma. JAMA Surg. 2019;154:500–8. https://doi.org/10.1001/jamasurg.2019.0096.
Yamamoto R, Cestero RF, Suzuki M, Funabiki T, Sasaki J. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is associated with improved survival in severely injured patients: A propensity score matching analysis. Am J Surg. 2019. https://doi.org/10.1016/j.amjsurg.2019.09.007.
García AF, Manzano-Nunez R, Orlas CP, et al. Association of resuscitative endovascular balloon occlusion of the aorta (REBOA) and mortality in penetrating trauma patients. Eur J Trauma Emerg Surg. 2020. https://doi.org/10.1007/s00068-020-01370-9.
Saito N, Matsumoto H, Yagi T, et al. Evaluation of the safety and feasibility of resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2015;78:897–903. https://doi.org/10.1097/TA.0000000000000614.
Park Y, Yu B, Lee G, Lee J, Choi K, Han A. Implementation of resuscitative endovascular balloon occlusion of the aorta at the Korean Regional Trauma Center. Hong Kong J Emerg Med. 2019. https://doi.org/10.1177/1024907919866563.
Irahara T, Sato N, Moroe Y, Fukuda R, Iwai Y, Unemoto K. Retrospective study of the effectiveness of Intra-Aortic Balloon Occlusion (IABO) for traumatic haemorrhagic shock. World J Emerg Surg. 2015;10:1. https://doi.org/10.1186/1749-7922-10-1.
Teeter WA, Matsumoto J, Idoguchi K, et al. Smaller introducer sheaths for REBOA may be associated with fewer complications. J Trauma Acute Care Surg. 2016;81:1039–45. https://doi.org/10.1097/TA.0000000000001143.
Tsurukiri J, Akamine I, Sato T, et al. Resuscitative endovascular balloon occlusion of the aorta for uncontrolled haemorrahgic shock as an adjunct to haemostatic procedures in the acute care setting. Scand J Trauma Resusc Emerg Med. 2016;24:13. https://doi.org/10.1186/s13049-016-0205-8.
Moore LJ, Martin CD, Harvin JA, Wade CE, Holcomb JB. Resuscitative endovascular balloon occlusion of the aorta for control of noncompressible truncal hemorrhage in the abdomen and pelvis. Am J Surg. 2016;212:1222–30. https://doi.org/10.1016/j.amjsurg.2016.09.027.
Martinelli T, Thony F, Decléty P, et al. Intra-aortic balloon occlusion to salvage patients with life-threatening hemorrhagic shocks from pelvic fractures. J Trauma. 2010;68:942–8. https://doi.org/10.1097/TA.0b013e3181c40579.
Sadeghi M, Nilsson KF, Larzon T, et al. The use of aortic balloon occlusion in traumatic shock: first report from the ABO trauma registry. Eur J Trauma Emerg Surg. 2018;44:491–501. https://doi.org/10.1007/s00068-017-0813-7.
Matsumura Y, Matsumoto J, Kondo H, et al. Early arterial access for resuscitative endovascular balloon occlusion of the aorta is related to survival outcome in trauma. J Trauma Acute Care Surg. 2018;85:507–11. https://doi.org/10.1097/TA.0000000000002004.
Ordoñz CA, Khan M, Cotton B, et al. The Colombian experience in Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA): The Progression from a large caliber to a low-profile device at a level I trauma center. Shock. 2021;56:42–5. https://doi.org/10.1097/SHK.0000000000001515.
Barnard EBG, Morrison JJ, Madureira RM, et al. Resuscitative endovascular balloon occlusion of the aorta (REBOA): a population based gap analysis of trauma patients in England and Wales. Emerg Med J. 2015;32:926–32. https://doi.org/10.1136/emermed-2015-205217.
Inoue J, Shiraishi A, Yoshiyuki A, Haruta K, Matsui H, Otomo Y. Resuscitative endovascular balloon occlusion of the aorta might be dangerous in patients with severe torso trauma: A propensity score analysis. J Trauma Acute Care Surg. 2016;80:559–66. https://doi.org/10.1097/TA.0000000000000968.
Hörer TM, Hebron D, Swaid F, et al. Aorta balloon occlusion in trauma: Three cases demonstrating multidisciplinary approach already on patient's arrival to the emergency room. Cardiovasc Intervent Radiol. 2016;39:284–9. https://doi.org/10.1007/s00270-015-1212-2.
Brenner M, Teeter W, Hoehn M, et al. Use of resuscitative endovascular balloon occlusion of the aorta for proximal aortic control in patients with severe hemorrhage and arrest. JAMA Surg. 2018;153:130–5. https://doi.org/10.1001/jamasurg.2017.3549.
Norii T, Crandall C, Terasaka Y. Survival of severe blunt trauma patients treated with resuscitative endovascular balloon occlusion of the aorta compared with propensity score-adjusted untreated patients. J Trauma Acute Care Surg. 2015;78:721–8. https://doi.org/10.1097/TA.0000000000000578.
DuBose JJ, Scalea TM, Brenner M, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg. 2016;81:409–19. https://doi.org/10.1097/TA.0000000000001079.
Bogert JN, Davis KM, Kopelman TR, Vail SJ, Pieri PG, Matthews MR. Resuscitative endovascular balloon occlusion of the aorta with a low profile, wire free device: A game changer? Trauma Case Rep. 2017;7:11–4. https://doi.org/10.1016/j.tcr.2017.01.006.
Sato R, Kuriyama A, Takaesu R, et al. Resuscitative endovascular balloon occlusion of the aorta performed by emergency physicians for traumatic hemorrhagic shock: a case series from Japanese emergency rooms. Crit Care. 2018;22:103. https://doi.org/10.1186/s13054-018-2032-y.
Romagnoli A, Teeter W, Pasley J, et al. Time to aortic occlusion: It's all about access. J Trauma Acute Care Surg. 2017;83:1161–4. https://doi.org/10.1097/TA.0000000000001665.
Jansen J, Campbell M, Cochran C, Clancy A. UK REBOA Trial 2017. Available from: https://w3.abdn.ac.uk/hsru/REBOA/Public/Public/index.cshtml.
DIRECT So. Direct-IABO Registry 2017. Available from: http://direct.kenkyuukai.jp/about/index.asp?
Trauma TAAftSo. Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) 2013. Available from: https://www.aast.org/Research/MultiInstitutionalStudies.aspx.
Funding
None.
Author information
Authors and Affiliations
Contributions
Ho Juen Ko was responsible for the design of the study, acquisition and analysis of data, and drafting of manuscript. Hui Fen Koo was responsible for design of the study, acquisition and analysis of data, and drafting of manuscript. Nina Al-Saadi was responsible for critical revision of manuscript. Saied Froghi was responsible for design of the study and critical revision of manuscript.
Corresponding author
Ethics declarations
Ethics approval
As this study is a systematic review and meta-analysis using publicly accessible research articles, institutional ethical approval was not sought before commencing the study.
Informed consent statement
Consent to participate or publish not obtained as this study is a systematic review and meta-analysis using publicly accessible research articles.
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ko, H.J., Koo, H.F., Al-Saadi, N. et al. A comparison of mortality and indicators of treatment success of resuscitative endovascular balloon occlusion of aorta (REBOA): a systematic review and meta-analysis. Indian J Thorac Cardiovasc Surg 39, 27–36 (2023). https://doi.org/10.1007/s12055-022-01413-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-022-01413-3