Abstract
Intrathoracic synovial cell sarcomas are extremely rare tumors with a high rate of recurrence after resection. We report one such case of synovial cell sarcoma arising from the chest wall, which was completely intrathoracic without an external component. The tumor was resected twice and in spite of adjuvant chemo-radiation the tumor recurred. Radical resection of the tumor with reconstruction of the chest wall and diaphragm using titanium mesh and polypropylene mesh respectively was done. A latissimus dorsi flap cover was provided. Titanium mesh is an excellent prosthesis of choice for reconstruction, as it provides stability and better cosmesis of the chest wall. Radical resection can be offered for suitable candidates, with very low morbidity and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft tissue sarcomas constitute about 1% of all adult malignancies [1]. They often present as slow-growing indolent tumors of the extremities. Primary synovial sarcomas of the chest wall are rare and carry an unfavorable prognosis [2]. These tumors require aggressive chest wall resection to achieve negative margins. Reconstruction of the defect poses a challenge to the surgeon in terms of providing adequate functional status for the patient with minimal morbidity.
Case report
A 19-year-old male presented with complaints of cough and tachypnea in April 2015. Positron emission tomography–computed tomography (PET-CT) revealed a necrotic mass lesion near the right pericardial region with patchy increased metabolic activity. The tumor was excised through a right posterolateral thoracotomy and was reported as a schwannoma.
After a disease-free interval of 5 years, the patient presented with features of superior vena cava (SVC) obstruction in March 2020. Computed tomography (CT) showed a bilobed circumscribed lesion with smooth lobulated margins measuring 16 × 9.5 × 14 cm in the anterior mediastinum compressing the SVC and projecting into the right hemithorax (Supplementary Fig. 1). CT-guided biopsy was reported as spindle cell neoplasm with atypia. The tumor board was convened at the time of SVC obstruction and radiation was planned as a palliative procedure, in the event of unsuccessful surgical decompression. An emergency sternotomy was done. The tumor was found to be adherent to the pericardium, diaphragm, and a portion of the lung. The mass was debulked without injury to the adjacent structures, but the origin of the tumor could not be made out. The histopathology was reported as a high-grade spindle cell sarcoma consistent with poorly differentiated synovial sarcoma (grade 3). Adjuvant chemo-radiation was given and CT repeated in November 2020 showed complete resolution of the mass.
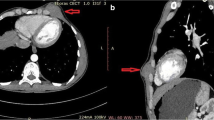
In March 2021, recurrence of the tumor was noted on follow-up CT. A trial of chemotherapy failed to show reduction in size (Fig. 1). As the tumor recurred again, a tumor board was convened and the patient was planned for aggressive resection and chest wall reconstruction.
Diagnostic laparoscopy done to assess operability showed that the liver and the posterior half of the diaphragm were free. Laparoscopy showed that the tumor had not breached the abdominal wall and the peritoneum was intact. No seedlings were noted. An oblique right thoraco-abdominal incision was made. The latissimus dorsi muscle was preserved; the serratus muscle was retracted laterally exposing the chest wall from the 3rd to 11th rib. Diaphragmatic resection was done taking care to achieve adequate margins free of tumor. Anteriorly, the ribs were detached at the costochondral junction and laterally they were resected with a margin of 2.5 cm. The lung parenchyma adherent to the tumor was resected with adequate margins using gastrointestinal anastomosis (GIA) linear staplers (ETHICON™). The tumor, along with the chest wall and part of diaphragm, was removed. The diaphragmatic defect was reconstructed using a polypropylene mesh, 15 × 15 cm, anchoring it to the parietal wall and the remaining diaphragm (Fig. 2). The chest wall reconstruction was achieved using a titanium mesh, which was anchored to the remaining ribs posteriorly and costochondral junction anteriorly (Fig. 3). The latissimus dorsi muscle flap was mobilized to give soft tissue cover to the titanium mesh partially. Intercostal and subcutaneous drains were placed. The histopathology was reported as a monophasic synovial sarcoma with no lymphovascular invasion. All margins were free of tumor.
The patient was able to carry out his daily activities with minimal loss of function. Chest wall contour was well preserved and there was no drooping of the shoulder (Supplementary Fig. 2). Unfortunately, the patient developed multiple lung secondaries 6 months after the surgical procedure, which were identified by CT done as a part of surveillance. He underwent adjuvant chemotherapy but succumbed due to progression of the disease.
Discussion
Soft tissue sarcomas of the thorax are rare in occurrence. The indolent course leads to delayed diagnosis and the necessity to achieve wide R0 resection results in significant defects of the chest wall, requiring elaborate skeletal reconstruction and soft tissue cover.
Male gender, truncal as opposed to distal tumor location, lesions larger than 5 cm, high histologic grade, aneuploidy, poor histological differentiation, and local recurrence are adverse prognostic factors [2].
With aggressive preoperative treatments, acceptable surgical results with low morbidity and mortality can be achieved. Neoadjuvant systemic therapy may reduce local and distant recurrence and improve overall survival. Chest wall resections in primary soft tissue sarcomas can be accomplished safely with a low mortality rate. Long-term survival can be achieved for primary soft tissue sarcomas, but histological grading is of prognostic significance.
In our case, the histopathological evidence claiming the tumor to be of benign etiology led to less aggressive surgical management in the first instance. The second surgery was done as a lifesaving procedure due to SVC obstruction. Complete resection was not achieved and the patient was subjected to chemotherapy and radiation. Recurrent disease with lack of distant spread, young age, and good general condition of the patient made him an ideal candidate for a more radical procedure.
The size of the chest wall defect is directly related to postoperative complications, as a consequence of impaired respiratory function and instability of the chest. Patients who require resection of ≥ 3 ribs, or chest wall defect of size > 6 cm, need reconstruction with prostheses [3]. For defects in sternal and parasternal sites, rigid prosthesis is important to maintain the structural integrity, to prevent chest wall collapse, and to protect the intrathoracic organs. The ideal chest wall prosthetic material should be rigid enough to prevent paradoxical motion during respiration and protect intrathoracic organs, malleable enough for proper contouring, inert, biocompatible as to allow tissue growth, radiolucent to ease radiographic follow-up, resistant to infection, and affordable [4, 5]. Common prostheses used are Marlex mesh (polypropylene), Vicryl mesh, and expanded polytetrafluoroethylene (ePTFE) materials. Though these are cheap and have good affinity for tissue ingrowth, they lack the rigidity provided by titanium meshes; and hence, flail chest occurs when used for large defects.
Titanium meshes have been widely utilized in the repair of skull defects and have been recently proposed as alternatives for chest wall reconstruction [3, 6]. They are usually produced in 0.4-mm and 0.6-mm thickness; the latter being preferred for large anterolateral chest wall defects. They are highly biocompatible and provide enough strength, rigidity, and flexibility, and are relatively more resistant to infection [7]. Titanium meshes also possess suitable radiolucency and are compatible with magnetic resonance imaging [8]. In various case series, titanium meshes have been used and have provided excellent results after chest wall resections.
The patient recovered well with the use of the titanium mesh, as the structural rigidity of the chest wall was maintained. The only downside to the use of titanium mesh, which we felt would be a problem, was the difficulty we would encounter if the need arose to insert an intercostal drain in the future. Wound healing was on par with our experience with other reconstructive prostheses.
Conclusions
Intrathoracic synovial cell sarcoma is a rare entity which requires extensive resection to achieve negative margins. With the advent of newer reconstruction techniques, surgery is possible with minimal morbidity and mortality. Titanium mesh offers the advantage of skeletal stability over the other available prostheses. They could be used more often and also as the primary choice with large chest wall defects.
Data availability
Not applicable.
References
Zahm SH, Tucker MA, Fraumeni JF Jr. Soft tissue sarcomas. In: Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. 2nd ed. New York: Oxford University Press; 1996. p. 984–99.
Zagars GK, Ballo MT, Pisters PWT, et al. Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer. 2003;97:2530–43.
Seder CW, Rocco G. Chest wall reconstruction after extended resection. J Thorac Dis. 2016;8:S863–71. https://doi.org/10.21037/jtd.2016.11.07.
Sanna S, Brandolini J, Pardolesi A, et al. Materials and techniques in chest wall reconstruction: a review. J Vis Surg. 2017;3:95. https://doi.org/10.21037/jovs.2017.06.10.
Gonfiotti A, Santini PF, Campanacci D, et al. Malignant primary chest-wall tumours: techniques of reconstruction and survival. Eur J Cardiothorac Surg. 2010;38:39–45.
Tamburini N, Grossi W, Sanna S, et al. Chest wall reconstruction using a new titanium mesh: a multicenters experience. J Thorac Dis. 2019;11:3459–66. https://doi.org/10.21037/jtd.2019.07.74.
Horio H, Ohtsuka T, Kubota Y, et al. Large chest wall reconstruction using titanium micromesh and a pedicled latissimus dorsi musculocutaneous flap: report of a case. Surg Today. 2005;35:73–5. https://doi.org/10.1007/s00595-004-2868-4.
Iarussi T, Pardolesi A, Camplese P, Sacco R. Composite chest wall reconstruction using titanium plates and mesh preserves chest wall function. J Thorac Cardiovasc Surg. 2010;140:476–7. https://doi.org/10.1016/j.jtcvs.2009.07.030.
Funding
None.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the editing and publishing of this case report.
Corresponding author
Ethics declarations
Ethics approval
Obtained Ref no – bh/ec/soy/cr/21 dated 13–09-2021.
Informed consent statement
Written informed consent was obtained from the patient for publishing this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any experimental studies with human or animal subjects.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12055_2022_1378_MOESM1_ESM.jpg
Supplementary file1 SVC OBSTRUCTION[AX1] – CT thorax showingSVC obstruction prior to the second surgery[AX1]CE: pls insert/present supplementary information correctly. (DOCX 673 KB)
12055_2022_1378_MOESM2_ESM.jpg
Supplementary file2 POST OPERATIVE IMAGE – Photographyshowing the thoracoabdominal healed scar and the cosmesis offered by thetitanium mesh. (DOCX 18 KB)
Rights and permissions
About this article
Cite this article
Nedumaran, B., Krishnasamy, A., Mahalingam, S. et al. Primary intrathoracic synovial cell sarcoma requiring radical resection of the chest wall and diaphragm with reconstruction using titanium mesh. Indian J Thorac Cardiovasc Surg 38, 644–647 (2022). https://doi.org/10.1007/s12055-022-01378-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-022-01378-3