Abstract
Parosteal osteosarcoma represents a low-grade, well-differentiated type of cortical surface osteosarcoma with a relatively better prognosis. Systemic metastasis is rare overall and occurs in 10–15% of patients only. Delayed recurrences (>5 years) of parosteal osteosarcoma are even rarer and only few isolated case reports of local recurrence with systemic metastasis occurring beyond 10 years exist in the literature. We present here a case of femoral parosteal osteosarcoma, successfully treated previously, that recurred with high-grade transformation locally and with lung metastasis after 12 years. The patient was managed by lung wedge resection followed by type A1 rotationplasty. Histopathology report confirmed evidence of high-grade transformation (de-differentiation) both locally and at the metastatic site, in view of strong CDK4 and MDM2 nuclear immuno-expression. The present report highlights the importance of long-term follow-up, even for a seemingly less aggressive osteosarcoma variant with identification of a novel pattern of lung metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma (OS), a primary bone malignancy, is one of the most common neoplasms of the musculoskeletal system. In comparison to widely occurring intramedullary/conventional OS, surface osteosarcomas are much less common (3–6% of total) which include parosteal osteosarcoma (POS), periosteal OS, and high-grade surface OS [1]. POS is an uncommon, distinct, and slow-growing type of surface OS that originates from the cortical surface of the bone. Being a World Health Organization (WHO) low-grade tumor [2], wide resection alone is curative in most cases.
The incidence of metastasis in POS is low; however, they have propensity to differentiate to high-grade conventional OS with systemic metastasis [1]. We present this case to describe a case of POS of the distal femur in a female patient, initially treated by wide resection 12 years ago, who later developed recurrence at the primary site and an unusual pattern of pulmonary metastasis. We reviewed the literature highlighting various aspects related to this rare histopathological phenomenon of de-differentiation in POS and report a novel imaging pattern, with unusual intraoperative experience, encountered while managing one such case.
Case report
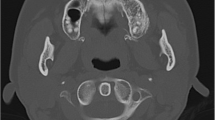
A 28-year-old female had presented to our institution with complaints of pain in the right lower limb. She was a known case with POS of the right distal femur who was previously treated with limb salvage surgery 12 years back at a tertiary cancer center. Postoperative histopathology report revealed low-grade POS with chondroid foci with all margins clear histologically. She was on regular follow-up until 2013. However, she was lost to follow-up in between and was again evaluated for localized pain and swelling along the previous operative site in mid-2019. She was evaluated with contrast-enhanced magnetic resonance imaging (MRI) which revealed a 15.0 × 7.5 × 7 cm lesion in the antero-medial aspect of the thigh in postoperative bed, encasing the right femoral artery. Chest X-ray postero-anterior view revealed a right lung calcified lesion. Computed tomography (CT) of the chest revealed a calcified pleural-based thickening in the right upper lobe of the lung and extending into the oblique fissure (Fig. 1). A CT-guided core needle biopsy from the right pleural plaque was suggestive of metastasis of high-grade OS. She received 4 cycles of Adriamycin-, cisplatin-, and ifosfamide-based chemotherapy at the primary tertiary cancer center. Post chemotherapy, positron emission tomography (PET) evaluation confirmed stable disease without any evidence of disease progression in the right thigh or lung.
Following this patient presented to our institute, slides or blocks from previous surgery were unavailable for our institutional review. The case was discussed in a multi-disciplinary tumor board and surgery was planned for local disease along with pulmonary metastasectomy in view of being a solitary site of metastasis.
Subsequently, the patient underwent a staged procedure of right-sided open pulmonary metastasectomy followed by type A1 rotationplasty. She underwent right-sided diagnostic thoracoscopy using one-lung ventilation, which confirmed the lesion localized to the upper lobe and fissure peripherally. Thoracoscopy revealed lung mass adhered to the parietal pleura by fibrous tissue without direct infiltration (Fig. 2a). A postero-lateral thoracotomy was done and extra-pleural mobilization was done taking parietal pleura en-bloc which served as the lateral margin. Dissection proceeded from the fissure area towards the lung apex. Small wedge of involved lower lobe across the fissure was taken. A clear interface between the bony hard plaque and normal parenchyma of the upper lobe was palpable and the plaque was dissected away from it using a harmonic scalpel. As the dissection proceeded towards the apex, the apical segment of the upper lobe could not be visualized in view of the large-sized plaque. We used chisel-hammer to break the plaque in the apical segment of the lung, and subsequently complete excision of mass along with overlying parietal pleura was achieved (Fig. 2b). The remaining lung parenchyma, which was dissected off from the plaque, was staple ligated with the endovascular gastrointestinal anastomosis (Endo-GIA) stapler providing an additional free margin and closing surface air leak. A chest drain was inserted. Postoperative chest X-ray showed expanded lung and chest tube was removed on postoperative day 2 and the patient was discharged on day 3. Two months later, the patient underwent type A1 rotationplasty for recurrence in postoperative tumor bed in the right thigh. She withstood the procedure well and discharged uneventfully. The patient is on follow-up now for 3 months and is doing well.
Histopathology report from local as well as from lung metastasis showed anastomosing bone trabeculae with intervening fascicles of neoplastic spindle cell proliferation with moderate atypia and significant mitosis. On immunohistochemistry (IHC), the neoplastic spindle cells show diffuse and strong nuclear positivity for CDK4 and MDM2, suggestive of high-grade conventional metastatic OS, de-differentiating from POS (Fig. 3a–f).
Histopathology section showing (a) neoplastic spindle cells infiltrating surrounding skeletal muscle (thin arrow). Osteoid deposition is seen by these cells (thick arrows). (b) Neoplastic spindle cells exhibit marked atypia with significant mitosis (arrow). (c) Neoplastic spindle cells are heterogeneously positive for MDM2 with moderate intensity. (d) Neoplastic spindle cells show diffuse and strong nuclear CDK4 immuno-expression surrounding osteoid (arrow). (e) Sections from metastatic lung lesion show neoplastic spindle cells infiltrating lung parenchyma alveoli (thin arrow) and significant osteoid deposition is seen by these cells (thick arrow). (f) CDK4 nuclear immuno-expression is seen strongly in neoplastic spindle cells surrounding the osteoid (thick arrow), while no expression is seen in pneumocytes lining the alveoli (thin arrow)
Discussion
The first description of POS in the literature was by Geschickter and Copeland in 1951, when they described it as “parosteal osteoma” [3]. In 1994, Okada et al. [4] described parosteal variant to be present if (a) cortical surface lesion seen on X-ray; (b) on pathology, the tumor is well differentiated (grade 1 or 2) with well-formed osteoid within a spindle cell stroma; and (c) less than 25% of the medullary cavity involvement. Most recently, WHO described POS as a low-grade cortical surface bone tumor, which may progress to high-grade sarcoma—referred to as de-differentiation [2].
De-differentiation of POS has been described uncommonly in literature. In a recent publication by Rizzoli Institute, they reported 195 cases of POS over a period of 120 years with only 48 cases showing de-differentiation. The authors studied old tissue blocks using diagnostic CDK4 and MDM2 IHC markers and reclassified them as per the current classification system which was misclassified earlier due to lack of uniform histopathological description criteria for POS before 1990s. De-differentiation can occur either synchronously or at the time of recurrence [5].
Both local recurrence and risk of systemic metastasis is low in conventional POS. However, our patient developed both with a delayed presentation after 12 years of margin-negative resection. Ruengwanichayakun et al. [5] reported 23% recurrence rate in patients with POS in Rizzoli series with a median time to recurrence of 36 months. The publication did not provide data on recurrence rate in conventional POS group separately. In this series, although 19% (n = 37) patients developed lung metastasis, only 4.8% developed metastasis in conventional POS cohort compared to 62% in patients presenting initially with de-differentiated POS. Hence, per se conventional POS constitutes a low-risk group. Delayed recurrences defined as recurrence occurring after 5 years are uncommon. Only case reports [6] have been described in literature of such a phenomenon happening more than a decade after the initial disease, so this case adds aptly to an already scanty data on de-differentiation in a conventional POS after a decade.
In the present case, the imaging appearance of lung deposit was unusual and has never been described earlier in literature. Seo et al. [7] had given a detailed description of atypical pulmonary metastasis occurring from OS metastasis with either focal bony deposits or pneumothorax; however, a streak of bony calcification/ossification involving peripheral lung parenchyma of whole lobe of the lung, with extension into fissure, has never been encountered before the present case. Similarly, in pediatric patients, Gagnon et al. [8] had described atypical pulmonary deposits from sarcomas as well as carcinomas, wherein only focal nodular deposits with calcification from OS metastasis have been widely described, but references for rim-like calcification do not exist in literature to date, to the best of our knowledge, after literature search.
The inevitable question that arises from this case is: why should a recurrence happen after a supposedly “curative” treatment given to the patient? POS being a low-grade surface OS does not warrant chemotherapy. The present patient did not receive chemotherapy, as per the prevailing guidelines at that time. Margin-negative surgery suffices as a curative treatment option. Studies have found a statistically significant association only between surgical margin and recurrence [1]. In the largest series by Rizzoli Institute, presence of de-differentiated component in primary tumor was associated with significantly adverse prognosis [5].
POS has a most favorable prognosis amongst all OS types. In the study by Song, 10-year overall survival was 86% with majority of patients having an event-free survival after a decade-long follow-up [9]. In this subset of patients with favorable prognosis, the exact follow-up plan after 5 years of disease-free interval seems unclear. Most guidelines, including the National Comprehensive Cancer Network (NCCN) 2020 [10] guidelines, recommend at least a yearly follow-up after 5 years. “Lost to follow-up” is an important challenge in cancer care with many patients quitting contact with health care system at variable time intervals. Studies have determined that long-term follow-up may not prevent recurrences, but may detect recurrences at a treatable stage [11]. It is imperative that a thorough discussion with patients and care-givers be undertaken to determine the follow-up plan explaining the pros of it. There remains a continuous need to motivate and stress upon the patients to remain in annual, life-long follow-up for favorable disease outcomes and to detect recurrences at a salvageable stage.
In accordance with oncological principle of en-bloc excision of malignant masses, we acknowledge the fact that every attempt should be made in all cases for en-bloc removal of tumor which could not be followed in principle in this case. We had to break a portion of bony hard deposit to access disease in the apico-posterior region for complete excision of mass which was substantiated later by margin-negative (R0) resection. However, this was the best effort for removing a high-grade recurrence and preservation of functional lung volume in a young patient at risk of additional lung metastasis, requiring further metastasectomy in foreseeable future. Hence, the patient will remain in close follow-up to detect any recurrence at early and salvageable stage.
Conclusion
The present case represents an unusually delayed and rare recurrence with de-differentiation occurring in a conventional POS with demonstration of a novel imaging pattern of OS lung metastasis for future reference. At the same time, this report further re-emphasizes the importance of prolonged follow-up for optimizing long-term outcomes of cancer survivors.
References
Kumar VS, Barwar N, Khan SA. Surface osteosarcomas: diagnosis, treatment and outcome. Indian J Orthop. 2014;48:255–61.
World Health Organization, International Agency for Research on Cancer. WHO classification of tumours of soft tissue and bone. 5th ed. Cree, I editor. Lyon: IARC Press; 2020.
Geschickter CF, Copeland MM. Parosteal osteoma of bone: a new entity. Ann Surg. 1951;133:790–806.
Okada K, Frassica FJ, Sim FH, Beabout JW, Bond JR, Unni KK. Parosteal osteosarcoma. A clinicopathological study. J Bone Joint Surg Am. 1994;76:366–78.
Ruengwanichayakun P, Gambarotti M, Frisoni T, et al. Parosteal osteosarcoma: a monocentric retrospective analysis of 195 patients. Hum Pathol. 2019;91:11–8.
Ellegast J, Barth TFE, Schulte M, Bielack SS, Schmid M, Mayer- Steinacker R. Metastasis of osteosarcoma after 16 years. J Clin Oncol. 2010;29:e62–6.
Seo JB, Im JG, Goo JM, Chung MJ, Kim MY. Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics. 2001;21:403–17.
Gagnon M-H, Wallace AB, Yedururi S, Khanna G. Atypical pulmo- nary metastases in children: pictorial review of imaging patterns. Pediatr Radiol. 2021;51:131–9.
Song WS, Jeon D-G, Cho WH, et al. Clinical outcome of parosteal osteosarcoma. J Korean Bone Joint Tumor Soc. 2013;19:20–7.
bone.pdf. [cited 2020 Dec 21]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/bone.pdf.
Gill A, Gosain R, Bhandari S, et al. “Lost to follow-up” among adult cancer survivors. Am J Clin Oncol. 2018;41:1024–7.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the Institutional Ethics Committee (IEC) in view of the retrospective nature of the study; all the procedures being performed were part of the routine care and as patient’s consent was already taken for publication.
Consent to publish
The participant has consented to the submission of the case report for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goel, V., Pasricha, S., Pruthi, M. et al. Parosteal osteosarcoma with high-grade transformation and lung metastasis after 12 years: a rare presentation. Indian J Thorac Cardiovasc Surg 38, 62–66 (2022). https://doi.org/10.1007/s12055-021-01214-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01214-0