Abstract
Gastrinomas are located largely in the pancreaticoduodenal region. However, gastrinomas have also been found in non-pancreaticoduodenal regions. Our study is a rare report of gastrinomas within the thoracic cavity. A 53-year-old male patient presented with acute abdomen and multiple prepyloric ulcers. Serum gastrin level was significantly elevated. Computed tomography (CT) scan of the chest, abdomen, and pelvis showed a mass in the inferior section of the right hemithorax. Octreotide scan also confirmed a neuroendocrine tumor (NET)-like mass in the right para-aortic region in the right hemithorax. In thoracotomy, a hypervascular solid tumor was detected adjacent to the aorta, also receiving a branch from the aorta. We ligated the feeding artery and resected the 3-cm tumor. The post-operative serum gastrin level was 36 pg/mL, which implied that the tumor was successfully resected. The pathology assessment reported nests of monotonous low-grade neuroendocrine cells with salt and pepper nuclei with rare mitotic features, cellular uniformity, and abundant amphophilic cytoplasm, confirming the diagnosis of gastrinoma. Based on our report, we suggest that the search for gastrinomas should include not only the abdominal sites but also uncommon areas like the thoracic cavity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrinoma is a functional neuroendocrine tumor (NET), primarily characterized by increased gastric acid secretion leading to abdominal pain, secretory diarrhea, and severe ulcers in different areas of the stomach, known as Zollinger–Ellison syndrome (ZES). It is estimated that 0.5 to 21.5 cases per million population are diagnosed with gastrinomas each year [1]. Studies have shown that 0.1% of peptic ulcers and 2–5% of recurrent ulcers are caused by gastrinomas [2]. Gastrinomas are generally sporadic (75–80%). Nonetheless, approximately 20 to 25% are linked with multiple endocrine neoplasia type 1 (MEN-1) [1]. Gastrinomas are located largely in the pancreaticoduodenal region (duodenum (70%) and pancreas (25%)) [3]. However, gastrinomas have also been found in non-pancreaticoduodenal regions, such as the small intestine mesenteric lymph nodes, spleen, stomach, liver, and thoracic cavity. Gastrinomas are frequently misdiagnosed because they are relatively rare and lack specific signs or symptoms. Although serum gastrin level is of great significance, a definite diagnosis relies on pathological and immunohistochemical assessments. Surgical management is still the sole curative treatment for gastrinomas [3]. The current study reports a 53-year-old male patient diagnosed with gastrinomas in the thoracic cavity, who was treated successfully by surgical resection. Written informed consent was acquired from the patient for publication of this report.
Case report
In 2018, a 53-year-old male patient presenting with acute abdomen was admitted to the emergency department of Imam Khomeini Hospital (Tehran, Iran). The patient presented with sudden and severe abdominal pain with no previous history of smoking, drinking, and non-steroidal anti-inflammatory drugs (NSAIDs) and anticoagulant medication. On physical examination, the patient had tenderness, rebound tenderness, and guarding, particularly in the epigastrium. The patient underwent explorative laparotomy with a diagnosis of peritonitis. A prepyloric peptic perforation was detected during surgery, which was repaired using oversew and omental patch technique. During surgery, a sample biopsy was obtained from the margin of the tumor to test for malignancy, which was negative.
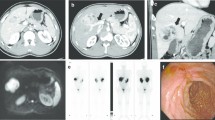
The patient underwent endoscopic evaluation at the 3-month follow-up visit to investigate the cause for prepyloric ulcer. Endoscopy showed multiple ulcers in different parts of the stomach. Serum gastrin level was measured with suspicion of gastrinoma, which was significantly elevated (1457 pg/mL; normal range, 13–115 pg/mL). Urea breath test for Helicobacter pylori was negative. Ultrasonographic assessment of the abdomen and the pelvis showed no significant pathologic finding, but computed tomography (CT) scan of the chest, abdomen, and pelvis revealed a mass in the inferior section of the right hemithorax (Fig. 1a). With suspicion of NET, an octreotide scan was conducted, revealing a NET-like mass in the right para-aortic region in the right hemithorax (Fig. 1b). Due to several clinical and paraclinical evidence indicative of gastrinoma (including multiple gastric ulcers, elevated serum gastrin level, NET-like mass in octreotide scan), the patient underwent posterolateral thoracotomy. After releasing the adhesions, a hypervascular solid tumor was detected adjacent to the aorta, also receiving a branch from the aorta. We ligated the feeding artery, resected the 3-cm tumor, and sent the tumor sample for pathologic evaluation (Fig. 2). The post-operative serum gastrin level was 36 pg/mL, which implied that the tumor was successfully resected. The pathology assessment reported nests of monotonous low-grade neuroendocrine cells with salt and pepper nuclei with rare mitotic features, cellular uniformity, and abundant amphophilic cytoplasm, confirming the diagnosis of gastrinoma (Fig. 3). After the surgery, the patient was transferred to the intensive care unit (ICU) and after 24 h to the thoracic surgery ward. The patient was discharged in good general condition 12 days after the surgery. After a 6-month treatment with proton pump inhibitors, the patient was followed with clinical and laboratory evaluation and endoscopy. On clinical evaluation, his pallor was improved, and the patient had experienced a 10% weight gain. On laboratory evaluation, the hematocrit was increased by 11%, and the serum gastrin level was in the normal range. In agreement, endoscopy showed improved and healed ulcers.
The microscopic view of the resected tumor with different magnifications. (a) Ribbons/trabeculae and rosette formation (low magnification; ×4). (b) Cellular uniformity, salt and pepper nuclei and rare mitotic figures; compatible with well-differentiated neuroendocrine tumor (high magnification; ×40); black arrows show salt and pepper nuclei appearance
Discussion
Gastrinomas are NET entities typically associated with gastric hypersecretion, hyperacidity, and severe or recurrent gastric ulcers. Gastrinomas are a relatively rare NET with an incidence of 0.5 to 21.5 cases per million population [1]. Even so, gastrinomas are the second most common type of NET after insulinomas [3]. Gastrinomas can be categorized into two separate groups of sporadic gastrinomas (entailing 75% of all gastrinomas) and gastrinomas associated with MEN-1. MEN-1 is usually associated with hyperparathyroidism, pancreatic NETs, and pituitary adenoma. While most gastrinomas grow slowly, nearly 50–60% are malignant and metastatic at diagnosis with a 5-year survival rate of 20–38% [4]. Peripheral lymph nodes and the liver are the most common metastatic sites.
Development of peptic ulcers in atypical areas including distal duodenum and jejunum or multiple peptic ulcers necessitates diagnostic evaluations for gastrinomas. Furthermore, gastrinomas are among the differential diagnosis for refractory or recurrent peptic ulcers, secretory diarrhea, rugal stomach hypertrophy, esophageal stricture, perforated ulcers, and peptic ulcers with hypercalcemia. In this report, our patient had multiple peptic ulcers in the stomach, raising the suspicion that gastrinoma might be the underlying cause.
Current literature on gastrinomas shows that gastrinomas are located almost always in the pancreaticoduodenal region (duodenum (70%) and pancreas (25%)) [3]. However, there are few reports of gastrinomas in other regions, including the heart, the liver, spleen, intestine mesenteric lymph nodes, and thoracic cavity. In 1997, Gibril et al. [5] described a patient with a cardiac gastrinoma causing ZES. The exact identification of this gastrinoma in the heart (and extra-abdominal site) was facilitated using octreotide scanning for somatostatin receptors that gastrinomas typically possess in great numbers. Later in 1999, Noda et al. [6] reported a successful resection of a gastrinoma located in the interventricular septum using cardiopulmonary bypass, blood cardioplegia, and mild hypothermia.
Similar to our report, Sampathirao et al. [7] reported a case of thoracic neuroendocrine tumor in a patient who presented with peptic ulcers and raised serum gastrin level. As in our report, they could not identify the location of a possible gastrinoma or any other mass in the abdomen with conventional imaging modalities and endoscopic evaluation. Somatostatin receptor-targeted imaging with 68Ga-DOTATATE positron emission tomography–computed tomography (PET-CT) was conducted and showed a somatostatin receptor-expressing paravertebral tumor next to the thoracic aorta in the left lung. In contrast to their study, we used an octreotide scan for the identification of gastrinoma. Moreover, the gastrinoma was in the right hemithorax of our patient.
The main differential diagnosis of ZES and multiple peptic ulcers are Helicobacter pylori infections, NSAID and anticoagulant medication, malignancies, retained gastric antrum, and gastric outlet obstruction. In this case, a sample biopsy from the margin of the tumor was negative for malignancy. Furthermore, the urea breath test for Helicobacter pylori was negative. Other possible structural causes were ruled out using a thoraco-abdominopelvic CT scan.
Our study is a rare report of gastrinoma within the thoracic cavity. The elevated gastrin level coupled with multiple peptic ulcers on endoscopic evaluation raised the differential diagnosis of a gastrinoma. A suspicious mass was seen in the thoracic cavity, which was later confirmed to be a gastrinoma on histopathological studies. Based on our report, we suggest that the search for gastrinomas should include not only the abdominal sites but also uncommon areas like the thoracic cavity.
Data availability
Not applicable.
Code availability
Not applicable.
References
Falconi M, Eriksson B, Kaltsas G, et al. ENETS Consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016;103:153–71. https://doi.org/10.1159/000443171.
Andersen DK. Current diagnosis and management of Zollinger-Ellison syndrome. Ann Surg. 1989;210:685–703. https://doi.org/10.1097/00000658-198912000-00001.
Zhang W-D, Liu DA-R, Wang P, Zhao J-G, Wang Z-F, Chen LI. Clinical treatment of gastrinoma: A case report and review of the literature. Oncol Lett. 2016;11:3433–3437. https://doi.org/10.3892/ol.2016.4397.
Fendrich V, Langer P, Waldmann J, Bartsch DK, Rothmund M. Management of sporadic and multiple endocrine neoplasia type 1 gastrinomas. Br J Surg. 2007;94:1331–41. https://doi.org/10.1002/bjs.5987.
Gibril F, Curtis LT, Termanini B, et al. Primary cardiac gastrinoma causing Zollinger-Ellison syndrome. Gastroenterology. 1997;112:567–74. https://doi.org/10.1053/gast.1997.v112.pm9024311.
Noda S, Norton JA, Jensen RT, Gay WA Jr. Surgical resection of intracardiac gastrinoma. Ann Thorac Surg. 1999;67:532–3. https://doi.org/10.1016/S0003-4975(98)01205-3.
Sampathirao N, Basu S. Rare occurrence of hypergastrinemia due to thoracic neuroendocrine tumor: detection and characterization by 68Ga-DOTATATE PET/CT. J Nucl Med Technol. 2016;44:203–4. https://doi.org/10.2967/jnmt.115.171603.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Written informed consent was acquired from the patient for participation in this report.
Consent for publication
Written informed consent was acquired from the patient for publication of this report.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rafieian, S., Vahedi, M., Jahanbin, B. et al. Primary thoracic gastrinoma causing Zollinger-Ellison syndrome. Indian J Thorac Cardiovasc Surg 37, 706–709 (2021). https://doi.org/10.1007/s12055-021-01211-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01211-3