Abstract
Rosai-Dorfman disease (RDD) is a rare nonmalignant disorder which seems to be a proliferation of histiocytes of unknown etiology that mainly affects lymph nodes but most other organs of the body. Our case is a diagnostic dilemma due to its atypical presentation. We report a history of Moroccan female 57 years old who was thought to have recurrent hemoptysis with endobronchial obstructive tumor and atelectasis of the lung. The diagnosis of Rosai-Dorfman disease was eventually made following a range of investigations including CT scans and histological analysis of specimens after bronchial débulking through rigid bronchoscopy. She has an upper right destroyed lobe and lobectomy was performed with histologically a definitive diagnosis of RDD. She remains well with no further progression of the disease. We think that Rosai-Dorfman disease can mimic endobronchialcarcinoma, so histological confirmation should be sought in all cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1969, Rosai and Dorfman (RDD) described a benign pathological entity termed sinus histiocytosis with massive lymphadenopathy [1]. The lymph node sinuses appear dilated and colonized by large numbers of these histiocytes. Extranodal manifestations have been reported in 43% of cases and may affect almost every tissue, including vital organs. Intrathoracic manifestations of RDD were reported only in 3% of patients with RDD [2]. In our knowledge, there is no case report describing the involvement of bronchus; only tracheal involvement was reported by Zhou et al. [3].
The aim of this article is to present the diagnosis and therapeutic management of Rosai-Dorfman disease through a case of bronchial involvement.
Case report
A 57-year-old non-smoking Moroccan female presented with history of recurrent hemoptysis with dry cough in last 3 months. She was referred to our department for evaluation of abnormal chest x-ray showed heterogeneous opacity in upper field of right pleural space (Fig. 1). She had been become increasingly dyspnea on exertion and hemoptysis most frequent. She had no chest pain, weight loss, or night sweats.
On presentation to the department, her physical examination showed a low breath sounds in the right upper field without palpable lymphadenopathy. Laboratory investigations including C reactive protein, complete blood count, renal and liver function tests were within normal limits.
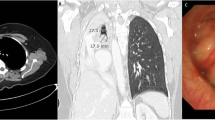
On admission, chest computed tomography (CT) of the thorax was performed which showed a soft tissue mass in the upper field of right lung with a zone of consolidation suspect of atelectasis (Fig. 2).
Bronchoscopic findings proved a protruding lesion from orifice of bronchus of right upper lobe (RUL). Multiple biopsies were performed. Histological analysis of the specimens revealed massive histiocytic infiltration underneath the bronchial epithelium with lymphocytes within the cytoplasm of histiocytes like cells. Immunohistochemistry showed that the histiocytes were reactive to S100 protein and CD68 but not CD1a, confirming a diagnosis of Rosai-Dorfman disease.
After multidisciplinary team discussion, thoracotomy and resection of the right upper lobe was performed without complications.
The postoperative period was without incident and the hemoptysis disappeared. The patient was discharged 8 days after surgery. The patient was completely asymptomatic and she did never complain of cough.
Postoperative histological examination of the mass showed dense infiltrate composed predominantly of histiocytes with vesicular nuclei; these histiocytes engulfing numerous intact lymphocytes within their eosinophilic cytoplasm, a condition called lymphocytophagocytosis or emperipolesis (Fig. 3a). Immunohistochemistry showed that the histiocytes stained positive for S-100 protein and the macro phage markers CD68 (Fig. 3b). There was no CDla expression. The diagnosis of Rosai-Dorfman disease was established. The patient remained well without any treatment or evidence of progression since May 2011 today.
Discussion
Rosai-Dorfman disease (RDD) was erst described in 1969 [1], also known as sinus histiocytosis that the most common presentation is bilateral massive painless cervical lymphadenopathy [2]. It is a rare non-malignant proliferation of histiocytes of unknown etiology with male preponderance, which runs a protracted course with remissions and to date, there is no known treatment.
It affects lymph nodes and various extra nodal sites as well. Mediastinal lymphadenopathy is the most common intrathoracic manifestation of RDD [3]. Fever, weight loss, hemoptysis, nasal discharge, and obstruction may also be presenting features of this disease [2]. The common symptoms include painless, bilateral cervical lymphadenopathy with fever. Histopathologically, the condition is due to an inflammatory infiltrate of a subtype of S-100 positive histiocytes characterized by hemophagocytosis.
Other intrathoracic manifestations included airway disease, pleural effusion, cystic and interstitial lung disease. Case reports have been published on primary central airway involvement; endobronchial disease was documented in our study with pseudotumoral bronchial involvement and recurrent hemoptysis. Imaging endings was consistent with a large mass of lung mimicking lung carcinoma. From a macroscopic point of view, bronchoscopy confirmed about 90% obstruction of the superior right lobar bronchus with the lesions which are polyploidy and zoophytic. Prior to surgical lobar specimen, the provisional diagnosis based on bronchial debunking through rigid bronchoscopy with histology analysis of tissue specimen.
Confirmation of RDD is made by identification of emperipolesis and immune-histochemical staining with S100 protein+/CD68 +/CD1a. The phenomenon of emperipolesis is highly useful for the diagnosis of RDD; it consists of numerous large histiocytes with abundant pale cytoplasm and phagocytized lymphocytes; the lymphocytes are not attacked by enzymes and appear intact within the histiocytes (in contrast to phagocytosis) [4].
Viruses such as human herpes simplex and human immunodeficiency virus have been associated without strong evidence, and the role of macrophage colony stimulating factor has also been considered as a possible trigger factor [3, 4].
Extranodal involvement has been reported in approximately 43% of patients. Different extranodal sites including the skin, central nervous system, kidneys, orbit, skull, liver, pancreas, and oral cavity have been reported to be involved [2]. Involvement of the larynx, lung, and pleura has been reported in only a few cases, so histological confirmation should be sought in all cases given the benign nature of the disease. Pulmonary involvement is rare and occurs approximately in only 3% of cases with extranodal disease. It can mimicking lung carcinoma and even show increased activity on positron emission tomography (PET-CT) scanning. The 18F-fluorodeoxyglucose (18FDG) (PET-CT) scan may demonstrate pathologic uptake in involved organs and may be useful in documented the extent of disease in patients with RDD [2].
RDD may closely simulate other disease states in its clinical manifestations, especially malignant lymphoma, histiocytosis, and non-neoplastic disorders including storage diseases. RDD is occasionally complicated by sickle cell disease, autoimmune lymphoproliferative syndrome, and histiocytic sarcoma in the literature [3].
Rosai-Dorfman disease is a rare disorder which follows a relatively benign course in most patients and the occurrence of intrathoracic involvement with RDD does not seem to portend a worse prognosis compared to other patients without thoracic involvement [5]. There is no ideal treatment for RDD; generally, the management ranges from just observation to radiotherapy, surgical debunking, or resection depending on the organ involved and severity of the disease. Multiple chemotherapeutic agents have been tried with variable degrees of success and there have been some reported effects from the use of corticosteroids [3, 4].
Conclusion
In conclusion, the pathogenesis of RDD with massive endobronchial involvement remains unclear but the prognosis seems good after resection of destroyed lobe. The disease is generally self-limiting and treatment with low dose corticoid is usually successful.
References
Rosai J, Dorfmann RF. Sinus histiocytosis with massive lymphadenopathy: a pseudolymphomatous benign disorder—analysis of 34 cases. Cancer. 1972;30:1174–88.
Ali A, Mackay D. Rosai-Dorfman disease of the lung. Thorax. 2009;64:908–9.
Zhou LF1, Chen L, Zhu Q, et al. Unusual life-threatening Rosai-Dorfman disease of the trachea: role of NF-Κb. Thorax 2010. 65:927–9.
Noguchi S, Yatera K, Shimajiri S, et al. Intrathoracic Rosai-Dorfman disease with spontaneous remission: a clinical report and a review of the literature. Tohoku J Exp Med. 2012;227:231–325.
Cartin-Ceba R, Golbin JM, Yi ES, Prakash UB, Vassallo R. Intrathoracic manifestations of Rosai-Dorfman disease. Respir Med. 2010;104:1344–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funds for this case.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
Informed consent was obtained for this case from the patient.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Alloubi, I., Marouf, R., Lazguet, Y. et al. Endobronchial Rosai-Dorfmann disease mimicking lung carcinoma: case presentation. Indian J Thorac Cardiovasc Surg 33, 64–66 (2017). https://doi.org/10.1007/s12055-016-0474-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-016-0474-x