Abstract
Glycogen storage diseases (GSDs) are caused by abnormalities in enzymes that are involved in the regulation of gluconeogenesis and glycogenolysis. GSD I, an autosomal recessive metabolic disorder, is the most common GSD and has four subtypes. Here, we examined GSD Ia caused by the defective glucose-6-phosphatase catalytic (G6PC) gene. We investigated the frequency of GSD Ia and clarified its molecular aspect in patients with the main clinical and biochemical characteristics of GSD, including 37 unrelated patients with a mean age of three years at the time of diagnosis. All patients belonged to the Azeri Turkish population. Hypoglycaemia and hypertriglyceridaemia were the most frequent laboratory findings. Mutations were detected by performing direct sequencing. Mutation analysis of the G6PC gene revealed that GSD Ia accounted for 11% in GSD patients with involvement of liver. Three patients were homozygous for R83C mutation. In addition, a novel stop mutation, Y85X, was identified in a patient with the typical features of GSD Ia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glycogen storage diseases (GSDs) are a heterogeneous group of inherited disorders caused by defects in glycogen degradation and synthesis. GSDs are mainly observed in children and it mostly affects the liver, muscle and heart (Koshy et al. 2006). GSDs can be differentiated based on clinical, biochemical and enzymatic examination of the liver tissue. Based on enzyme deficiency, they are classified into 10 major types (Mundy and Leeb 2004), and GSD I, GSD III, GSD VI and GSD IX usually affect the liver severely (Kido et al. 2013). GSD I, which was first described by von Gierke, is the most common form of GSD (Özen and Bayraktar 2007). GSD I has four subtypes, namely GSD Ia, characterized by defects in glucose-6-phosphatase catalytic subunit (G6 Pase); GSD Ib, presented by deficiency in glucose-6-phosphate translocase; GSD Ic, described by defects in a putative phosphate transporter; and GSD Id, caused by defects in a putative glucose transporter (Chou and Mansfield 2008; Kasapkara et al. 2012).
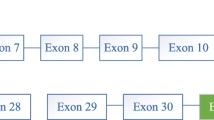
GSD Ia is a recessively inherited metabolic disorder prevalence of approximately about one in 100,000 live births (Mundy and Leeb 2004; Zheng et al. 2015). It is caused by a defect in the glucose-6-phosphatase catalytic (G6PC) system, which catalyzes the hydrolysis of G6P to phosphate and glucose. G6PC is a single-copy gene and is located on chromosome 17q21 (Lei et al. 1994a, 1994b). It consists of five exons spanning approximately 12.5-kb DNA and has tissue-restricted expression, predominantly in liver, kidney and intestine (Lei et al. 1993, 1994a, 1994b). The gene encodes a hydrophobic protein containing 357 amino acids and nine transmembrane domains (Pan et al. 1998). Analysis of mutations in the G6PC gene can be performed to obtain more conclusive results (Mundy and Leeb 2004; Liang et al. 2013).
Defects in the G6PC system increase glucose-6-phosphate (G6P) levels in the cytoplasm. This triggers alternative metabolic pathways that lead to the accumulation of glycogen in liver and kidneys, thus contributing to progressive hepatomegaly and nephromegaly. Elevated cytoplasmic G6P levels result in metabolic consequences, such as hypercholesterolamia, hypertriglyceridamia, hyperuricaemia and lactic acidamia (Janecke et al. 2001; Eminoğlu et al. 2013). To date, various mutations have been reported in the G6PC gene, including missense (the most prevalent form), nonsense, insertion/deletion and splicing (Rake et al. 2000; Chou and Mansfield 2008). Here, we present molecular analysis of suspected GSD Ia patients to provide a DNA-based method for carrier and prenatal diagnosis in Iranian Azeri Turkish patients.
Materials and methods
Study subjects
In the present study, we included 37 unrelated patients with a mean age of 3 years (age range between 5 months and 13 years) who demonstrated clinical features of GSD (Froissart et al. 2011; Kishnani and Chen 2015). The patients were screened by their physicians at a children’s hospital in Tabriz between February 2011 and July 2014, and were referred to our laboratory for molecular investigation (table 1).
Of the 37 patients, 34 were from the northwestern region of Iran and three were from the Republic of Azerbaijan (located to the northwest of Iran). All patients had the same ethnic background (Azeri Turkish population).
The study was approved by the institutional review board and ethical committee of the Tabriz University of Medical Sciences, Tabriz, Iran. Informed consent was obtained from the families of the patients. Diagnostic criteria were based on the clinical and biochemical features of GSD; however, liver biopsy, enzyme analysis and mutation analysis were not performed (Froissart et al. 2011; Kishnani and Chen 2015).
We first measured the levels of serum creatine kinase (CK) and creatine phospho kinase (CPK), and excluded three patients with high CK and CPK levels from molecular analysis due to suspected GSD-III (Kishnani et al. 2010; Mogahed et al. 2015; Zheng et al. 2015).
Preparation of genomic DNA
Approximately 5 ml of intravenous blood samples were collected from all the patients into EDTA vacutainers and used for DNA extraction. Genomic DNA was extracted from leucocytes present in the peripheral blood by using the salting-out method.
PCR amplification and sequencing
Complete G6PC exons 1, 2, 3, 4 and 5 and intron/exon borders were amplified by performing PCR. Amplification was performed using a 25- μL reaction mixture containing 50 ng of genomic DNA, 200 μmol/L of dNTPs, 10 pmol of each primer, 1.5 U of Taq DNA polymerase, 1 × PCR buffer (10 mmol/L of KCl, 10 mmol/L of Tris-HCl (pH 8.3), 1.5 mmol/L of MgCl 2) and 6 mmol/L of MgCl 2 (Cinnagene, Tehran, Iran). PCR was performed using the following protocol: initial denaturation at 95 ∘C for 2 min; 35 cycles of denaturation at 95 ∘C for 30 s; annealing for 40 s; extension at 72 ∘C for 40 s; and final extension at 72 ∘C for 5 min (Gene Amp@ PCR System, Bio-Rad, USA). PCR-amplified fragments were purified, and mutation analysis was performed by direct DNA sequencing using reverse and forward primers (Macrogen, Seoul, South Korea).
Results
In total, 70% patients had an affected family member. Consanguineous marriage was observed in the families of 74% patients. Major findings of biochemical and physical examinations at the time of diagnosis were hypoglycaemia (blood sugar, <50 mg/dL) in 27 patients and increased serum triglycerides (>200 mg/dL) in 24 patients (table 1). Hepatomegaly was observed in all the patients, with most patients demonstrating a doll-like face. DNA sequencing demonstrated that three patients were homozygous for a substitution mutation 326C >T (R83C). Mutation analysis of G6PC identified a novel mutation, Y85X, in homozygous form in one patient (figure 1).
The 233C >A (Y85X) mutation leads to the substitution of tyrosine by a stop codon. This substitution results in the premature stop codon producing a truncated protein, which is only 24% of the original full-length protein and is predicted to have no catalytic activity. The newly identified mutation was present in an affected child born to consanguineous healthy, but carrier parents. The affected patients with the detected mutations belonged to four unrelated Iranian Azeri families. Mutation analysis of DNA obtained from their parents demonstrated that they carried the same mutation in the heterozygous form (figure 2). Other patients did not have mutations in G6PC. Meanwhile, three SNPs (rs758804611, rs222961 and rs144652516) were found in heterozygote status in three different patients other than the mutants (table 1).
Discussion
Characterization of G6PC and identification of mutations in this gene provide a DNA-based tool to diagnose patients clinically suspected of having GSD Ia. Moreover, mutation analysis of a family at risk of conceiving offspring with GSD Ia offers a DNA-based tool for prenatal diagnosis. Early diagnosis allows the employment of adequate metabolic control strategies and treatments to prevent complications and thus increases the quality of life (Mogahed et al. 2015). The rates of consanguineous marriages are high in Iran, therefore, a high prevalence of autosomal recessive metabolic diseases, such as hepatic glycogenoses is predictable (Hasanzadeh-Nazarabadi et al. 2006; Gialluisi et al. 2012). The prevalence of hepatic glycogenoses in Iran is unknown, and no case studies or detailed mutation studies on GSD have been reported to date (Motamed et al. 2011). Clinical diagnosis of GSD in patients included in the present study was not previously confirmed by performing enzyme assay of biopsied liver tissue or mutation analysis.
Mutation analysis of G6PC was performed for 34 patients with GSD who belonged to 34 unrelated families, and who had clinical and biochemical characteristics resembling those of GSD Ia. Direct DNA sequencing was performed to screen mutations in the coding region, intron/exon junctions and 5 ′ UTRs and 3 ′ UTRs of the G6PC gene. Upon molecular investigation, four of 34 GSDs (12%) with liver involvement were verified as being affected by GSD Ia. Molecular analysis of parents of these patients with GSD Ia, identified mutant alleles of G6PC in both parents. The R83C mutation in G6PC occurs at a CpG dinucleotide rich and is a C >T transition at nucleotide 326. The R83C mutation is common in Czech and Slovak (40%) (Kozák et al. 2000), Italian (46.2%) (Stroppiano et al. 1999) and Turkish (68.5%) patients with GSD Ia (Eminoğlu et al. 2012), and accounts for six of eight mutant alleles of G6PC in the present study. The active site mutation, R83C is associated with undetectable phosphohydrolase activity of G6 Pase in liver biopsy of patients (Lei et al. 1994a, 1994b). This is consistent with the results of in vitro investigations that Arg to Cys substitution at codon 83 abolishes the phosphohydrolase activity of G6 Pase (Lei et al. 1994a, 1994b). The homozygous Y85X nonsense mutation, producing a truncated protein, is predicted to be associated with no residual activity.
This evidence eases genotype–phenotype description, at least for patients homozygous for these two mutations. All patients affected by GSD Ia, either with R83C or with the novel mutation (Y85X), are associated with younger age at the time of diagnosis (<2 year) and with clinical findings including hepatomegaly, growth retardation and doll face. Triglyceride serum uric acid values were higher in all the four patients, and they also suffered from severe hypoglycaemia (table 1). Because of insufficient sample size and lack of allelic heterogeneity, statistical analysis and comparison between biochemical parameters associated with different mutations could not be performed. As reported previously, GSD Ia patients exhibit phenotypic heterogeneity; moreover, there is no clear evidence for a firm genotype–phenotype relationship for each GSD Ia gene mutation (Matern et al. 2002; Chou and Mansfield 2008). The GSD types with liver involvement are best distinguished through enzyme studies of liver tissue obtained by wedge biopsy. However, clinical, biochemical and histological features may suggest the type of GSD (Kishnani and Chen 2015). Type I, III and IX constitute 80% of hepatic GSDs (Chen 2001). In this study, around 12% (four of 37) of patients suffered from GSD Ia and the remaining patients might be affected by other subtypes of GSD which are not analysed. On the other hand, the primers that we designed and used allowed only the detection of mutations located in the coding region and intron/exon junctions and 5 ′ UTRs and 3 ′ UTRs of the gene. Therefore, mutations in the intron regions of G6PC gene, which may affect the rate of gene transcription or stability of the G6PC mRNA were not sequenced and eluded detection.
Finally, these results emphasize that GSDs are multisystem diseases that are particularly hard for clinicians to diagnose, and suggest that molecular diagnosis of GSDs is helpful to verify disease type and to offer appropriate clinical approach. Moreover, knowledge of the family’s pathogenic mutations facilitates to predict the risk of recurrence for future children; thus, it assists in counselling, carrier testing and prenatal diagnosis.
References
Chen Y. T. 2001 Glycogen storage diseases. In The metabolic and molecular bases of inherited disease (ed. C. Scriver, A. Beaudet, W. Sly, D. Valle, B. Childs and K. W. Kinzler), 8th edition, pp. 1521–1555. McGraw-Hill, New York, USA.
Chou J. Y. and Mansfield B. C. 2008 Mutations in the glucose-6-phosphatase-A (G6PC) gene that cause type Ia glycogen storage disease. Hum. Mutat. 29, 921–930.
Eminoğlu F. T., Ezgu F. S., Hasanoglu A. and Tumer L. 2012 Rapid screening of 12 common mutations in Turkish GSD 1a patients using electronic DNA microarray. Gene 518, 346–350.
Eminoğlu F. T., Tümer L., Okur I., Ezgü F. S. and Hasanoğlu A. 2013 Clinical properties and disease prognosis in cases of glycogen-storage disease type 1a and type 1b. Turk. Arch. Ped. 48, 117–122.
Froissart R., Piraud M., Boudjemline A. M., Vianey-Saban C., Petit F., Hubert-Buron A. et al. 2011 Glucose-6-phosphatase deficiency. Orphanet. J. Rare Dis. 6, 27.
Gialluisi A., Pippucci T., Anikster Y., Ozbek U., Medlej-Hashim M., Mégarbané A. et al. 2012 Estimating the allele frequency of autosomal recessive disorders through mutational records and consanguinity: the homozygosity index (HI). Ann. Hum. Genet. 76, 159–167.
Hasanzadeh-Nazarabadi M., Rezaeetalab G. H. and Dastfan F. 2006 Study of Youths’ knowledge, behavior, and attitude toward consanguineous marriages. Iranian J. Publ. Health. 35, 47–53.
Janecke A. R., Mayatepek E. and Utermann G. 2001 Molecular genetics of type 1 glycogen storage disease. Mol. Genet. Metab. 73, 117–125.
Kasapkara Ç. S., Tümer L., Okur I., Eminoğlu T., Ezgü F. S. and Hasanoğlu A. 2012 Hypercalcemia in glycogen storage disease type I patients of Turkish origin. Turk. J. Pediatr. 54, 35–37.
Kido J., Nakamura K., Matsumoto S., Mitsubuchi H., Ohura T., Shigematsu Y. et al. 2013 Current status of hepatic glycogen storage disease in Japan: clinical manifestations, treatments and long-term outcomes. J. Hum. Genet. 58, 285–292.
Kishnani P. and Chen Y. T. 2015 Defects in metabolism of carbohydrates. In Nelson textbook of pediatrics (ed. R. M. Kliegman, B. F. Stanton, J. S. Geme, N. Schor, R. E. Behrman), 20th edition, pp. 719–725. Saunders, Philadelphia, USA.
Kishnani P. S., Austin S. L., Arn P., Bali D. S., Boney A., Case L. E. et al. 2010 Glycogen storage disease type III diagnosis and management guidelines. Genet. Med. 12, 446–463.
Koshy A., Ramaswamy K., Correa M. and Rekha S. 2006 Glycogen storage disease: report of 17 cases from southern India. Indian J. Gastroenterol. 25, 182–184.
Kozák L., Francová H., Hrabincová E., Štastná S., Pešková K. and Elleder M. 2000 Identification of mutations in the glucose-6-phosphatase gene in Czech and Slovak patients with glycogen storage disease type Ia, including novel mutations K76N, V166A and 540del.5. Hum. Mutat. 16, 89.
Lei K. -J., Shelly L. L., Pan C. -J., Sidbury J. B., Chen Y. T., Nordlie R. C. et al. 1993 Mutations in the glucose-6-phosphatase gene that cause glycogen storage disease type 1a. Science 262, 580–583.
Lei K. -J., Pan C. -J., Shelly L. L., Lin B., Sidbury J. B., Chen Y. T. et al. 1994a Mutations in the glucose-6-phosphatase gene are associated with glycogen storage disease types Ia and IaSP, but not lb and Ic. J. Clin. Invest. 95, 234–240.
Lei K. -J., Pan C. -J., Shelly L. L., Liu J. L. and Chou J. Y. 1994b Identification of mutations in the gene for glucose-6-phosphatase, the enzyme deficient in glycogen storage disease type 1a. J. Clin. Invest. 93, 1994–1999.
Liang C., Liu L., Sheng H., Jiang M. and Yin X. 2013 Geneotype and phenotype in 20 patients with glycogen storage disease type Ia. Int. J. Pediatr. Endocrinol. 1, 175.
Matern D., Seydewitz H. H., Bali D., Lang C. and Chen Y. T. 2002 Glycogen storage disease type I: diagnosis and phenotype/genotype correlation. Eur. J. Pediatr. 1, S10–S19.
Mogahed E. A., Girgis M. Y., Sobhy R., Elhabashy H., Abdelaziz O. M. and El-Karaksy H. 2015 Skeletal and cardiac muscle involvement in children with glycogen storage disease type III. Eur. J. Pediatr. 74, 1545–1548.
Motamed F., Monajemzadeh M., Seifirad S., Ashrafi M. and Rasti A. 2011 Liver storage disease in Iran: a ten year study of liver biopsies in children medical center hospital in Tehran, Iran. Hepat. Mon. 11, 652–655.
Mundy H. and Leeb P. J. 2004 The glycogen storage diseases. Curr. Pediatr. 14, 407–413.
Özen H. and Bayraktar Y. 2007 Glycogen storage diseases: new perspectives. World J. Gastroenterol. 13, 2541–2553.
Pan C. -J., Lei K. -J., Annabi B., Hemrika W. and Chou J. Y. 1998 Transmembrane topology of glucose-6-phosphatase. J. Biol. Chem. 273, 6144–6148.
Rake J. P., Berge A. M., Visser G., Verlind E., Niezen-Koning K. E., Buys C. H. et al. 2000 Glycogen storage disease type Ia: recent experience with mutation analysis, a summary of mutations reported in the literature and a newly developed diagnostic flowchart. Eur. J. Pediatr. 159, 322–330.
Stroppiano M., Regis S., Di Rocco M., Caroli F., Gandullia P. and Gatti R. 1999 Mutations in the glucose-6-phosphatase gene of 53 Italian patients with glycogen storage disease type Ia. J. Inherit. Metab. Dis. 22, 43–49.
Zheng B. X., Lin Q., Li M. and Jin Y. 2015 Three novel mutations of the G6PC gene identified in Chinese patients with glycogen storage disease type Ia. Eur. J. Pediatr. 174, 59–63.
Acknowledgements
We extend our sincere appreciation and thanks to those patients who helped us to accomplish this study. We thank the gastrointestinal research center of Tabriz University of Medical Sciences for their financial support (grant no. GT-668). No other external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Corresponding editor: Kunal Ray
Mahmoud S. K., Khorrami A., Rafeey M., Ghergherehchi R. and Sima M. D. 2017 Molecular analysis of glycogen storage disease type Ia in Iranian Azeri Turks: identification of a novel mutation. J. Genet. 96, xx–xx
Rights and permissions
About this article
Cite this article
MAHMOUD, S.K., KHORRAMI, A., RAFEEY, M. et al. Molecular analysis of glycogen storage disease type Ia in Iranian Azeri Turks: identification of a novel mutation. J Genet 96, 19–23 (2017). https://doi.org/10.1007/s12041-016-0734-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12041-016-0734-y