Abstract
The pathological characteristics of Alzheimer’s disease (AD) include formation of senile plaques resulting from amyloid-β (Aβ) deposition and neurofibrillary tangles caused by tau hyperphosphorylation. Reducing tau hyperphosphorylation is crucial for treatment of AD. Network pharmacology analysis showed that CTS may reduce tau hyperphosphorylation by regulating the phosphatidylinositol 3 kinases/protein kinase B/ glycogen synthase kinase-3β (PI3K/Akt/GSK3β) pathway. We investigated the ability of cryptotanshinone (CTS) to reduce Aβ-induced tau hyperphosphorylation and characterized the underlying mechanisms. Amyloid-β42 oligomers (AβO) were used to establish an AD model in HT22 cells. The expression levels of tau and related proteins in PI3K/Akt/GSK3β pathway were measured using western blot and immunofluorescence staining. The above-mentioned proteins were then evaluated in an okadaic acid (OKA)-induced AD cell model to verify the results. Synapse-associated proteins including post-synaptic density protein-95 (PSD95) and synaptophysin were also evaluated. We found that CTS significantly reduced tau hyperphosphorylation at Ser202, Ser404, Thr181, and Thr231 in AβO- and OKA-induced cell models. Moreover, we also found that CTS reversed AβO-induced reductions in the levels of PSD95 and synaptophysin. We used LY294002 to block PI3K and the results showed that CTS exerted neuroprotective effects through regulation of the PI3K/Akt/GSK3β signaling pathway. In summary, we showed for the first time that CTS inhibited AD-related tau hyperphosphorylation and reduced the effects of AβO on the expression levels of PSD95 and synaptophysin via the PI3K/Akt/GSK3β pathway in HT22 cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most common type of dementia. Alzheimer’s disease is characterized by progressive cognitive decline and loss of independent living ability. There were 50 million patients with dementia worldwide in 2018, and the number of cases is increasing rapidly [1]. However, there are few effective therapies to improve cognitive function and halt neurodegenerative changes of AD in the long term [2].
The discoveries of neurofibrillary tangles in 1963 [3] and amyloid-β (Aβ) in 1984 [4] have led to several hypotheses regarding the pathogenesis and underlying mechanisms of AD. These hypotheses include the classic Aβ hypothesis, the tau hypothesis, and the neurotransmitter hypothesis [5]. Tau and Aβ are key pathological markers of AD central to the most widely accepted hypotheses regarding AD pathogenesis. Memory loss and cognitive decline in AD have been shown to correlate with accumulation of senile plaques and neurofibrillary tangles caused by insoluble Aβ deposition and abnormal tau phosphorylation, respectively [6]. The amyloid hypothesis proposes that Aβ is upstream of tau, and pathological Aβ production causes tau hyperphosphorylation [7]. However, recent clinical trials have shown that anti-Aβ therapy did not significantly prevent cognitive decline in patients with AD [8]. Furthermore, Aβ clearance failed to reduce pathological tau deposition [9]. These findings suggested that Aβ may be an initiating factor in AD pathology, and that tau may play an important role in disease progression [10]. Recent studies have indicated that concurrently targeting tau and Aβ may be an effective therapeutic approach for AD [10]. Reducing tau pathology could counteract Aβ-induced neuronal injury and cognitive decline [11, 12], a strategy which was supported by a recent human study [13]. Therefore, prevention of tau hyperphosphorylation may be promising for treatment of AD.
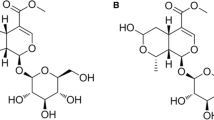
Traditional Chinese medicine (TCM) has been used for centuries in China. Salvia miltiorrhiza is a widely used traditional Chinese herbal medicine. It has been used for treatment of cardiovascular and cerebrovascular diseases for hundreds of years [14]. In recent decades, physician scientists have discovered that Salvia miltiorrhiza can be used for treatment of diabetes [15], osteoporosis [16], inflammation [17], and cancer [18]. Cryptotanshinone (CTS) (Fig. 1A), a natural quinone compound, is one of the main pharmacologically active components of Salvia miltiorrhiza. Previous pharmacological studies of CTS reported its anti-tumor, anti-inflammatory, neuroprotective, and cardioprotective properties, and its benefits for treatment of metabolic disorders [19]. Treatment with CTS has been shown to improve memory function in a scopolamine-induced AD rat model [20]. Studies have also shown that CTS could reverse glutamate-induced neuronal toxicity [21], reduce production of Aβ [22], and exert anti-neuroinflammatory effects [23] in animal models of AD. In vitro experiments showed that the anti-AD effects of CTS may be related to upregulation of α-secretase [24] and inhibition of Aβ aggregation [25]. Furthermore, CTS may exert anti-AD effects through inhibition of neuroinflammation [26] and Aβ production [27]. These studies suggested that CTS may be a potential treatment for human AD. However, the majority of these findings were based on the classic Aβ hypothesis. Few studies have evaluated the effects of CTS on tau hyperphosphorylation, which might be a key factor in drug efficacy.
Using network pharmacology, we identified CTS as a potential therapeutic drug for AD that regulates tau phosphorylation through the PI3K/Akt/GSK3β pathway. We induced AD models in cell culture using Aβ42 oligomer (AβO) and okadaic acid (OKA), to verify that treatment with CTS reversed tau hyperphosphorylation. We then characterized the underlying mechanisms of this effect. Our results showed that CTS may be a promising therapeutic agent for AD.
Materials and Methods
Network Pharmacology and Molecular Docking
We identified components of interest using network pharmacology and molecular docking. These procedures are described in detail in Supplementary Information. We extracted the components of the 10 most frequently used traditional Chinese medicinal drugs [28] from the Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform (TCMSP: https://www.tcmsp-e.com/) [29]. We then obtained the targets of the components that met our criteria from PubChem (https://pubchem.ncbi.nlm.nih.gov/) and matched the targets with the AD-related targets obtained from the DisGeNet database (https://www.disgenet.org/) [30]. The components with matching targets were selected for further protein–protein interaction (PPI) analysis, Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis, and Gene Ontology (GO) enrichment analysis. Finally, molecular docking was performed to determine which components to evaluate in subsequent experiments.
Cell Culture and Reagents
Immortalized hippocampal neurons (HT22) were obtained from LMAI Bio (Shanghai, China). Cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) containing 10% fetal bovine serum (FBS) and 1% penicillin–streptomycin (all Gibco) at 37 ℃ and 5% CO2. Unless otherwise specified, cells were seeded overnight and grown to 90% confluence in culture dishes or plates. Before treatment, the cells were starved with DMEM containing 2% FBS and 1% penicillin–streptomycin, for 2 h. To establish the AβO-induced AD cell model with tau hyperphosphorylation, we treated HT22 cells with 5 μM AβO (ChinaPeptides), as described in our previous study [31], for 3, 6, 12, or 24 h. The level of tau hyperphosphorylation was determined using western blot to select the best model induction time. Then, HT22 cells were treated with 2, 5, 10, or 20 μM AβO to determine the optimal AβO concentration to induce the AD model. Four experimental groups were used to evaluate the protective effects of CTS against AβO-induced neurotoxicity: (1) control group; (2) AβO-induced AD cell model; (3) AβO-induced AD cell model treated with CTS (the National Institutes for Food and Drug Control); and (4) cells pre-treated with PI3K inhibitor LY294002 (MedChemExpress) prior to cotreatment with AβO and CTS. We used another AD cell model to validate our findings. The three validation groups were as follows: (1) control group; (2) AD cell model induced by the PP2A inhibitor okadaic acid (OKA) (Yuanye) to generate tau pathology; (3) OKA-induced AD cells treated with CTS. Dimethylsulfoxide was added to the culture medium in the control groups at a volume equal to the highest volume included in the other treatment groups.
Preparation of AβO and CTS Solutions
One milligram of AβO powder was dissolved in 110 μL of DMSO (Sigma-Aldrich) to prepare a 2 mM stock solution. Twenty milligrams of CTS powder was dissolved in 6.75 mL of DMSO using ultrasonication to prepare a 10 mM stock solution. The stock solutions were diluted in complete medium to the desired concentrations at the time of use.
Cell Viability Using the MTT Assay
Cell viability was evaluated using the 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) (Sigma-Aldrich) assay after treatment with CTS or AβO. HT22 cells were seeded into 96-well microplates (Corning) at a density of 8 × 103 cells per well and cultured overnight. The cells were treated with 10 uL of MTT for 4 h, after which the media were replaced with 150 uL of DMSO. Optical density was recorded at 490, 570, and 630 nm.
Quantitative Reverse Transcription Polymerase Chain Reaction
Quantitative reverse transcription polymerase chain reaction (qRT-PCR) was used to determine the mRNA levels of postsynaptic density protein-95 (PSD95), synaptophysin (SYN), PI3K, Akt, GSK3β, and tau. HT22 cells were seeded in 6-well plates (corning) at a density of 7 × 105 cells per well. After serum starvation for 2 h, the cells were treated with 5 µM AβO for 6 h, 30 µM CTS for 6 h, or pre-treated with 30 µM CTS 3 h, then co-treated with 5 µM AβO and CTS for an additional 6 h. We extracted and reverse-transcribed the total ribonucleic acid (RNA) from HT22 cells into complementary deoxyribonucleic acid (cDNA) using the RNAsimple Total RNA Kit (Tiangen Tech) and the PrimeScript RT reagent Kit with gDNA Eraser (Takara Biotech). We used TB Green Premix® Ex Taq™ II to perform qRT-PCR on the StepOnePlus™ Real-time PCR System (Applied Biosystems) following the manufacturer’s instructions as follows: pre-incubation at 95 ℃ for 30 s for 1 cycle; denaturation at 95 ℃ for 5 s followed by annealing at 60 ℃ for 30 s for 40 cycles; and melting at 95 ℃ for 15 s, 60 ℃ for 1 min, and 95 ℃ for 15 s for 1 cycle. The oligonucleotide primer sequences used in this study are summarized in Table 1.
Western Blot
HT22 cells were cultured in 6-well plates at a density of 7 × 105 cells per well. The cells were treated as follows: (1) The control group was treated with media and DMSO; (2) the AβO-induced group was treated with 5 μM AβO for 6 h; (3) the treatment group was pre-treated with 30 μM CTS for 3 h and then co-treated with 5 μM AβO and 30 μM CTS for 6 h; (4) the inhibitor group was pre-treated with 10 μM LY294002 for 1 h and then co-treated with 10 μM LY294002 and 30 μM CTS for 3 h, and 10 μM LY294002, 30 μM CTS, and 5 μM AβO for another 6 h. Radioimmunoprecipitation assay buffer (RIPA) (Applygen) was used to extract total protein from the HT22 cells. The bicinchoninic acid protein assay kit (Beyotime) was used to measure the protein concentration, and all extracts were adjusted to the same concentrations using RIPA buffer. Mixed protein loading buffer (5X; WellBio) was added to the samples, and proteins were denatured by boiling at 100 ℃ for 5 min. Proteins were separated using sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) (SolarBio) and then electrotransferred onto polyvinylidene difluoride (PVDF) membranes (Millipore). The membranes were blocked with 5% non-fat milk for 2 h and then incubated overnight at 4 ℃ with the following primary antibodies: p-PI3K (1:500), PI3K (p85) (1:1,000), p-Akt (1:500), Akt (1:1,000), p-GSK3β (1:1,000), GSK3β (1:1,000), PSD95 (1:1,000), SYN (1:1,000), p-tau (Ser202) (1:500), p-tau (Ser404) (1:500), and tau (1:500), which were purchased from Cell Signaling Technology; p-tau (Thr231) (1:500) and p-tau (Thr181) (1:500), purchased from Abcam; and β-actin (1:2,000) purchased from ProteinTech. The membranes were incubated with secondary antibody (1:2,000) purchased from Cell Signaling Technology for 2 h after being washed with Tris–HCl buffer with 0.1% Tween 20 (TBST) 3 times. Finally, the protein blots were observed by enhanced chemiluminescence (ECL) (Millipore) using a Multi-Function Gel Image System (Bio Olympics) and analyzed using ImageJ software.
Immunofluorescence Staining
HT22 cells were seeded into poly-D-lysine-coated 24-well plates at a density of 6 × 104 cells per well. The cells were treated under the same condition as those used for western blot. The experiment was performed according to the manufacturer’s instructions. The cells were fixed in chilled 4% paraformaldehyde for 15 min and then blocked in blocking buffer for 1 h. Primary antibodies including anti-PSD95 and anti-p-tau (Ser404) purchased from Cell Signaling Technology, and anti-SYN purchased from Abcam were diluted in antibody dilution buffer (all 1:100) and incubated overnight at 4 ℃. The cells were then incubated with fluorochrome-conjugated secondary antibodies purchased from ProteinTech (all 1:200) for 1 h at room temperature and then incubated with DAPI for 10 min to label the nuclei. Images were collected by using a fluorescence microscope (Olympus). The average fluorescence intensity was analyzed using ImageJ software.
Statistical Analysis
All experiments were performed independently in triplicate. All data in this study are reported as the mean ± standard error of measurement (SEM). The normality of data distribution was assessed using the Shapiro–Wilk test. For normally distributed data, one-way analysis of variance (ANOVA) was used to detect differences among three or more groups, and Tukey’s post hoc test was used for pairwise comparisons when necessary. Nonparametric methods with Bonferroni correction for pairwise comparisons were used to analyze non-normally distributed data. P values < 0.05 were considered statistically significant. GraphPad Prism 8.0 (GraphPad Software Inc., California, USA) and SPSS software (version 22.0, SPSS, USA) were used to analyze the data and generate statistical charts.
Results
Network Pharmacology and Molecular Docking
The detailed results of the network pharmacology and molecular docking are summarized in Supplementary Information. Cryptotanshinone and imperatorin (IMP) were selected from a total of 1,232 components extracted from TCMSP. Kyoto Encyclopedia of Genes and Genomes Enrichment Analysis suggested CTS and IMP could exert therapeutic effects against AD through the PI3K/Akt/GSK3β pathway (Fig. 1B). Results from PPI analysis suggested that Akt occupied one of the most important positions in the PPI network, and GSK3β was also important in the PPI network (Fig. 1C). Molecular docking analysis showed that CTS was likely to bind to PI3K (Fig. 1D), Akt, and GSK3β. Therefore, the bioinformatics results indicated that CTS could exert therapeutic effects against AD via modulation of the PI3K/Akt/GSK3β pathway.
Amyloid-β42 Oligomer-Induced AD Cell Model with Tau Hyperphosphorylation
Cell viability analysis using the MTT assay showed that CTS exhibited no toxicity toward HT22 cells after 24 h at concentrations up to 30 μM (Fig. 2A). Therefore, we used 30 μM CTS as the therapeutic concentration for subsequent experiments. Treatment with 10 μM or higher concentrations AβO resulted in significant cytotoxicity in HT22 cells (Fig. 2B). Western blot analysis showed that 5 μM AβO induced the highest level of tau hyperphosphorylation at 6 h. The second-highest level of tau phosphorylation occurred at 12 h (Fig. 2C, E). Treatment with 5 μM AβO induced tau hyperphosphorylation at Ser202 to the greatest extent at 6 h (Fig. 2D, F). Based on these results, we treated cells with 5 μM AβO for 6 h in subsequent experiments.
Effect of CTS and AβO on cell viability and tau phosphorylation in HT22 cells. A) Cell viability after 24-h treatment of HT22 cells with CTS. B) Cell viability after 24-h treatment of HT22 cells with AβO. Tau phosphorylation at Ser202 after treatment of HT22 cells with AβO. C, E) Different treatment times and D, F) different concentrations were evaluated using western blot. * p < 0.005, n = 6 for MTT, n = 3 for western blot
Cryptotanshinone Attenuated AβO-Induced Tau Hyperphosphorylation in HT22 Cells
Quantitative RT-PCR showed that the levels of tau mRNA did not differ among the treatment groups (Figure S4A in Supplementary Information). However, the levels of tau phosphorylation at Ser202, Ser404, Thr181, and Thr231 were increased in response to AβO stimulation (Fig. 3A). To evaluate the effect of CTS on tau hyperphosphorylation in AD, we measured the levels of tau phosphorylation in the CTS pretreatment group and the AβO-stimulated group. Our results showed that pretreatment with 30 μM CTS for 3 h significantly inhibited AβO-induced tau hyperphosphorylation. Pretreatment with LY294002 (a PI3K inhibitor) prior to treatment with CTS resulted in higher levels of tau phosphorylation at Ser202, Ser404, Thr181, and Thr231 compared with those in the CTS group. To verify these results, tau phosphorylation at Ser404 was evaluated using immunofluorescence staining. The results were consistent with those from western blot analysis (Fig. 3F-G).
Effect of CTS treatment on AβO-induced HT22 cells. Western blot (A) showed the levels of tau phosphorylation at Ser202 (B), Ser404 (C), Thr181 (D), and Thr231 (E). Immunofluorescence staining showed the expression of p-tau at Ser404 in the different groups (F, G). Scale bar: 50 μm. * p < 0.005, n = 3 for western blot and immunofluorescence staining
Cryptotanshinone Regulated the PI3K/Akt/GSK3β Pathway in HT22 Cells
The PI3K/Akt pathway regulates a variety of physiological activities and associates with neurodegeneration [32]. The PI3K/Akt pathway is inhibited in the brain in AD, which may contribute to the pathological changes associated with AD [32]. Previous studies have indicated that AβO inhibited the PI3K/Akt pathway [33], which resulted in activation of GSK3β [34]. Increased GSK3β activity has been shown to play an important role in neuronal death and tau hyperphosphorylation. Quantitative RT-PCR results showed that the levels of PI3K, Akt, and GSK3β mRNA did not differ among the experimental groups (Figure S4B-D in Supplementary Information). To verify that CTS acted through the PI3K/Akt/GSK3β pathway to decrease tau hyperphosphorylation, we showed that the p-PI3K-Tyr458/total PI3K, p-Akt-Ser473/total Akt, and p-GSK3β-Ser9/total GSK3β ratios in HT22 cells were significantly lower in the AβO-induced AD cell model group compared with those in the control group. Administration of CTS significantly upregulated the three above-mentioned ratios in AβO-induced AD cell model, and LY294002 blocked the protective effect of CTS (Fig. 4).
Validation of the Effects of CTS Using OKA-Induced Tau Hyperphosphorylation in HT22 Cells
Protein phosphatase 2A (PP2A) is an important serine threonine phosphatase that can affect tau phosphorylation [35]. Okadaic acid is a specific PP2A inhibitor that can be used to generate AD models in animals or cells. Okadaic acid-induced AD models usually exhibit tau hyperphosphorylation and abnormal GSK3β phosphorylation [36]. Based on the findings in previous studies [37, 38], we treated HT22 cells with 40 nM OKA for 8 h to establish an AD cell model. In addition, we pretreated HT22 cells with 30 µM CTS for 3 h prior to treatment with OKA. Tau phosphorylation was significantly increased at Ser202, Ser404, Thr181, and Thr231 following treatment with OKA, which indicated establishment of the AD cell model (Fig. 5A-E). The ratios of p-Akt-Ser473/total Akt and p-GSK3β-Ser9/total GSK3β were also downregulated after OKA treatment. These effects were blocked by pretreatment with CTS (Fig. 5F-H).
Effect of CTS pre-treatment on OKA-induced HT22 cells. Western blot (A) showed the levels of tau phosphorylation at Ser202 (B), Ser404 (C), Thr181 (D), and Thr231 (E). The ratios of p-Akt-Ser473/total Akt (G) and p-GSK3β-Ser9/total GSK3β (H) were also determined using western blot (F). *p < 0.005, n = 3 for western blot
Cryptotanshinone Improved the Expression of Synapse-Associated Proteins
A typical pathological hallmark of AD is synaptic dysfunction [39]. Previous studies showed that AβO-induced neurotoxicity and synaptic dysfunction might be tau-dependent [40]. Therefore, we investigated the levels of the synapse-associated proteins (SYN [41] and PSD95 [42], which are indicators of synaptic function) using qRT-PCR and western blot to characterize the neuroprotective effects of CTS on the synapse. Quantitative RT-PCR results showed that the levels of SYN and PSD95 mRNA decreased significantly after AβO treatment, and these decreases were blocked by CTS pretreatment (Fig. 6A-B). Furthermore, SYN and PSD95 protein levels were significantly decreased in AβO-induced cells, and this effect was blocked by pre-treatment with CTS (Fig. 6C-E). The protective effects of CTS were blocked by LY294002. Immunofluorescence staining results agreed with those obtained using qRT-PCR and western blot (Fig. 6F-I). However, treatment with OKA did not alter the expression of SYN and PSD95 in HT22 cells (Figure S5 in Supplementary Information).
Effect of CTS treatment on AβO-induced HT22 cells. Levels of SYN (A) and PSD95 (B) mRNA were tested using qRT-PCR. Western blot (C) showed the protein levels of SYN (D) and PSD95 (E). Immunofluorescence staining showed the expression of SYN (F, H) and PSD95 (G, I) in the different groups. Scale bar: 50 μm. *p < 0.005, n = 4 for qRT-PCR, n = 3 for western blot and immunofluorescence staining
Discussion
Cryptotanshinone was selected as a candidate therapeutic agent for AD using bioinformatics and then evaluated in a series of experiments. This is the first study to investigate inhibition of tau hyperphosphorylation by CTS in AD cell models. The results showed that CTS inhibited AβO-induced tau hyperphosphorylation in HT22 cells through regulation of the PI3K/Akt/GSK3β pathway. This finding was validated in an OKA-induced AD cell model. In addition, CTS also protected synapse-associated proteins against AβO-induced downregulation in HT22 cells.
In recent decades, hundreds of drugs have been developed to treat AD, but few have succeeded in reversing pathological progression or cognitive decline [5]. Some experts have suggested that this lack of success may be due to these drugs being focused on a single target despite AD resulting from complex pathological mechanisms. Therefore, scientists have suggested adopting a multi-target approach [43]. Results from studies on drug combination therapy reported greater beneficial effects against cognitive and functional decline than monotherapies or placebo treatments, which supported the multi-target strategy [44, 45]. Compared with the conventional single-target therapeutic strategy, the multi-target strategy associated with TCM may provide dramatic benefits for AD treatment [46]. In this study, we screened components using network pharmacology with a multi-target strategy. Cryptotanshinone from Salvia miltiorrhiza was chosen for further evaluation. Cryptotanshinone had also been a candidate therapeutic agent in a previous network pharmacology study [47]. Salvia miltiorrhiza is a widely used herbal medicine for treatment of AD. The results of our network pharmacology analysis showed that CTS may be a promising therapeutic agent. In addition, molecular docking analysis showed that CTS could bind to PI3K. A literature review showed that CTS exerted therapeutic effects in AD cell or animal models via regulation of the MAPK pathway [26], regulation of the cellular response to peptides and inhibition of apoptosis [25], increased levels of neurotransmitters [20, 21], and regulation of PI3K-related pathways [21, 24]. The majority of previous studies focused on evaluation of the mechanisms of action of formulations comprised of multiple herbal medicines or a group of potentially beneficial components. However, previous studies did not evaluate the therapeutic potential or mechanisms of action of any individual components. In contrast, our study focused on a single component and characterized its mechanism of action.
Our study investigated the ability of CTS to reduce tau hyperphosphorylation, which is a key pathological feature of AD. Tau is the major neuronal microtubule-associated protein. Abnormal phosphorylation of tau is related to neurofibrillary tangles [48] and neuron death. According to the Aβ hypothesis, accumulation of Aβ precedes and induces development of neurofibrillary tangles and may require tau hyperphosphorylation to induce AD pathology [6]. A previous study showed that reduced tau phosphorylation ameliorated deficits induced by Aβ [11]. Therefore, inhibition of tau hyperphosphorylation might be critical to effective treatment of AD. Previous studies have identified drugs that can reverse the abnormal tau phosphorylation observed in AD models in vivo[49] and in vitro[50,51,52,53]. In this study, we showed that AβO-induced tau hyperphosphorylation at Ser202, Ser404, Thr181, and Thr231 was significantly inhibited by CTS pretreatment. Furthermore, our study verified this finding using immunofluorescence staining. In addition, OKA-induced tau hyperphosphorylation was inhibited by CTS pretreatment, which agreed with previous findings in studies that evaluated OKA-induced tau hyperphosphorylation in vivo [54] or in vitro [55]. Our results supported the hypothesis that CTS may reduce tau hyperphosphorylation.
The imbalance between protein kinases and protein phosphatases is considered a causal factor in tau hyperphosphorylation. Specifically, GSK3β and PP2A are considered to be the most important proteins in this imbalance [56]. The protein kinase GSK3β is regulated by phosphorylation (site Ser9 for inhibition and site Tyr216 for activation). Previous studies showed that PI3K and Akt were downregulated, and GSK3β was upregulated, in AD brains and AD models [57]. Several drugs have been identified that regulate this pathway [49, 51, 52, 55]. Network pharmacology analysis showed that Akt and GSK3β were key proteins, and that PI3K/Akt/GSK3β was the key pathway through which CTS inhibited tau hyperphosphorylation. We found that the ratios of p-PI3K-Tyr458/total PI3K, p-Akt-Ser473/total Akt, and p-GSK3β-Ser9/total GSK3β were decreased in the AβO-induced AD cell model, which was consistent with the results of previous studies [56]. These decreases were reversed by pretreatment with CTS, and the protective effect of CTS was blocked by LY294002 (a PI3K inhibitor). Our results showed that CTS blocked AβO-induced decreases in PI3K and downstream Akt and GSK3β activity in HT22 cells, resulting in inhibition of tau hyperphosphorylation. To validate our findings, we used OKA, a PP2A inhibitor, to establish another AD cell model for evaluation of the therapeutic effects of CTS. A previous study showed that PP2A was one of the most active protein phosphatases in dephosphorylation of tau in AD [58]. In a previous study, the activity of PP2A was downregulated, and the activity of GSK3β was upregulated in AD, which resulted in tau hyperphosphorylation [59]. In addition, the activity of GSK3β has been shown to be upregulated in OKA-induced AD models, which resulted in tau hyperphosphorylation [60]. In our study, the activity of Akt was downregulated and the activity of GSK3β was upregulated by OKA in HT22 cells. These changes were blocked by pretreatment with CTS, which was consistent with findings from studies of other drug candidates [37, 55, 61]. These results verified that CTS could improve tau hyperphosphorylation through activation of the PI3K/Akt/GSK3β pathway.
Loss of synapses is highly correlated with cognitive decline in AD progression [62]. Synaptic dysfunction is initiated by Aβ during the early stages of AD [63]. This synaptic dysfunction may be tau dependent [40]. Tau hyperphosphorylation may also cause synapse loss [64]. Neuron loss, synaptic dysfunction, and cognitive decline have been shown to be strongly associated with accumulation of Aβ and Aβ-induced reductions in the expression levels of SYN and PSD95 [65]. Postsynaptic density protein 95 is a major postsynaptic scaffold protein that has been shown to be critical to synaptic development of hippocampal neurons [66] and is required for long-term potentiation [67]. Preventing downregulation of PSD95 expression may preserve hippocampal neuron plasticity and cognitive function [68]. The expression of SYN is closely associated with the number of synapses [69], and SYN plays an important role in neuronal development [70]. Loss of SYN in the hippocampus has been shown to correlate with cognitive decline in AD [71]. Therefore, preservation of PSD95 and SYN expression may be crucial for protection of synaptic function and prevention of cognitive decline. Our results showed that the levels of SYN and PSD95 were decreased in response to AβO, and these decreases were blocked by CTS pretreatment, which indicated that CTS may protect synaptic function. The protective effect of CTS was blocked by LY294002, which indicated that CTS may preserve synaptic function through the PI3K pathway [72, 73]. The protective effects of CTS against synaptic dysfunction may be due to the negative effects of tau hyperphosphorylation on axonal transport of synaptic proteins [74, 75]. However, results from the OKA-induced cell model of AD indicated that hyperphosphorylated tau might play an intermediary role in Aβ-induced synaptic dysfunction in AD. A previous study reported results with no significant difference among groups in PSD95 in OKA-induced SY5Y cells, which agreed with the results of our study [76]. However, the results of an in vivo study showed that OKA downregulated the mRNA level of SYN in a rat model [77]. These contradictory results may indicate that hyperphosphorylated tau may have to persist for a longer period of time to cause synapse-associated protein loss. Additional in vivo studies are needed to clarify this discrepancy.
Synaptic dysfunction resulting from tau hyperphosphorylation- and AβO-induced dysregulation of Fyn and N-methyl-D-aspartate-receptor (NMDAR) r may also be a target of CTS [40]. However, synaptic dysfunction could be caused by many other factors. Synaptophysin and PSD95 are also regulated by other factors, including NMDAR, brain-derived neurotrophic factor (BDNF), mitochondrial dysfunction [39]. Therefore, CTS may improve synaptic function through other pathways, which should be the focus of future in vivo studies.
In the present study, we investigated the effects, and potential underlying mechanisms, of CTS on tau hyperphosphorylation in an AβO-induced AD cell model. We verified our findings in another OKA-induced cell model of AD. However, the results from the in vitro experiments were less reliable than those from in vivo experiments. In addition, characterization of the influence of OKA on synapse-associated proteins might also require in vivo experiments. Therefore, our future studies will include in vivo experiments to investigate the therapeutic effects and underlying mechanisms of CTS on AD.
Conclusion
This study showed that CTS inhibited AβO-induced tau hyperphosphorylation via the PI3K/Akt/GSK3β pathway. The expression of key synaptic proteins was upregulated by CTS in an AD cell model. Our results were strengthened by use of two typical AD cell models to verify our findings. CTS is an attractive candidate for treatment of AD due to its ability to inhibit tau hyperphosphorylation.
Data Availability
The datasets generated during and/or analyzed during this study are available from the corresponding author upon reasonable request.
References
Patterson C, International AsD (2018) World Alzheimer report 2018. Alzheimer’s Disease International
Cummings J, Lee G, Ritter A, Sabbagh M, Zhong K (2020) Alzheimer’s disease drug development pipeline: 2020. Alzheimer’s Dement 6(1):e12050. https://doi.org/10.1002/trc2.12050
Kidd M (1963) Paired helical filaments in electron microscopy of Alzheimer’s disease. Nature 197:192–193. https://doi.org/10.1038/197192b0
Glenner GG, Wong CW (1984) Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun 120(3):885–890. https://doi.org/10.1016/s0006-291x(84)80190-4
Liu PP, Xie Y, Meng XY, Kang JS (2019) History and progress of hypotheses and clinical trials for Alzheimer’s disease. Signal Transduct Target Ther 4:29. https://doi.org/10.1038/s41392-019-0063-8
Bloom GS (2014) Amyloid-β and tau: the trigger and bullet in Alzheimer disease pathogenesis. JAMA Neurol 71(4):505–508. https://doi.org/10.1001/jamaneurol.2013.5847
Götz J, Chen F, van Dorpe J, Nitsch RM (2001) Formation of neurofibrillary tangles in P301l tau transgenic mice induced by Abeta 42 fibrils. Science (New York, NY) 293(5534):1491–1495. https://doi.org/10.1126/science.1062097
Avgerinos KI, Ferrucci L, Kapogiannis D (2021) Effects of monoclonal antibodies against amyloid-β on clinical and biomarker outcomes and adverse event risks: A systematic review and meta-analysis of phase III RCTs in Alzheimer’s disease. Ageing Res Rev 68:101339. https://doi.org/10.1016/j.arr.2021.101339
Oddo S, Caccamo A, Shepherd JD, Murphy MP, Golde TE, Kayed R, Metherate R, Mattson MP et al (2003) Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron 39(3):409–421. https://doi.org/10.1016/s0896-6273(03)00434-3
Busche MA, Hyman BT (2020) Synergy between amyloid-β and tau in Alzheimer’s disease. Nat Neurosci 23(10):1183–1193. https://doi.org/10.1038/s41593-020-0687-6
Roberson ED, Scearce-Levie K, Palop JJ, Yan F, Cheng IH, Wu T, Gerstein H, Yu GQ et al (2007) Reducing endogenous tau ameliorates amyloid beta-induced deficits in an Alzheimer’s disease mouse model. Science (New York, NY) 316(5825):750–754. https://doi.org/10.1126/science.1141736
Vossel KA, Zhang K, Brodbeck J, Daub AC, Sharma P, Finkbeiner S, Cui B, Mucke L (2010) Tau reduction prevents Abeta-induced defects in axonal transport. Science (New York, NY) 330(6001):198. https://doi.org/10.1126/science.1194653
Arboleda-Velasquez JF, Lopera F, O’Hare M, Delgado-Tirado S, Marino C, Chmielewska N, Saez-Torres KL, Amarnani D et al (2019) Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: a case report. Nat Med 25(11):1680–1683. https://doi.org/10.1038/s41591-019-0611-3
Su CY, Ming QL, Rahman K, Han T, Qin LP (2015) Salvia miltiorrhiza: Traditional medicinal uses, chemistry, and pharmacology. Chin J Nat Med 13(3):163–182. https://doi.org/10.1016/s1875-5364(15)30002-9
Jia Q, Zhu R, Tian Y, Chen B, Li R, Li L, Wang L, Che Y et al (2019) Salvia miltiorrhiza in diabetes: A review of its pharmacology, phytochemistry, and safety. Phytomedicine 58:152871. https://doi.org/10.1016/j.phymed.2019.152871
Guo Y, Li Y, Xue L, Severino RP, Gao S, Niu J, Qin LP, Zhang D et al (2014) Salvia miltiorrhiza: an ancient Chinese herbal medicine as a source for anti-osteoporotic drugs. J Ethnopharmacol 155(3):1401–1416. https://doi.org/10.1016/j.jep.2014.07.058
Qin Y, Zheng B, Yang GS, Yang HJ, Zhou J, Yang Z, Zhang XH, Zhao HY et al (2020) Salvia miltiorrhiza-Derived Sal-miR-58 Induces Autophagy and Attenuates Inflammation in Vascular Smooth Muscle Cells. Mol Ther Nucleic Acids 21:492–511. https://doi.org/10.1016/j.omtn.2020.06.015
Wu CF, Bohnert S, Thines E, Efferth T (2016) Cytotoxicity of Salvia miltiorrhiza Against Multidrug-Resistant Cancer Cells. Am J Chin Med 44(4):871–894. https://doi.org/10.1142/s0192415x16500488
Wu YH, Wu YR, Li B, Yan ZY (2020) Cryptotanshinone: A review of its pharmacology activities and molecular mechanisms. Fitoterapia 145:104633. https://doi.org/10.1016/j.fitote.2020.104633
Wong KK, Ho MT, Lin HQ, Lau KF, Rudd JA, Chung RC, Fung KP, Shaw PC et al (2010) Cryptotanshinone, an acetylcholinesterase inhibitor from Salvia miltiorrhiza, ameliorates scopolamine-induced amnesia in Morris water maze task. Planta Med 76(3):228–234. https://doi.org/10.1055/s-0029-1186084
Zhang F, Zheng W, Pi R, Mei Z, Bao Y, Gao J, Tang W, Chen S et al (2009) Cryptotanshinone protects primary rat cortical neurons from glutamate-induced neurotoxicity via the activation of the phosphatidylinositol 3-kinase/Akt signaling pathway. Exp Brain Res 193(1):109–118. https://doi.org/10.1007/s00221-008-1600-9
Mei Z, Zhang F, Tao L, Zheng W, Cao Y, Wang Z, Tang S, Le K et al (2009) Cryptotanshinone, a compound from Salvia miltiorrhiza modulates amyloid precursor protein metabolism and attenuates beta-amyloid deposition through upregulating alpha-secretase in vivo and in vitro. Neurosci Lett 452(2):90–95. https://doi.org/10.1016/j.neulet.2009.01.013
Maione F, Piccolo M, De Vita S, Chini MG, Cristiano C, De Caro C, Lippiello P, Miniaci MC et al (2018) Down regulation of pro-inflammatory pathways by tanshinone IIA and cryptotanshinone in a non-genetic mouse model of Alzheimer’s disease. Pharmacol Res 129:482–490. https://doi.org/10.1016/j.phrs.2017.11.018
Mei Z, Situ B, Tan X, Zheng S, Zhang F, Yan P, Liu P (2010) Cryptotanshinione upregulates alpha-secretase by activation PI3K pathway in cortical neurons. Brain Res 1348:165–173. https://doi.org/10.1016/j.brainres.2010.05.083
Mei Z, Yan P, Situ B, Mou Y, Liu P (2012) Cryptotanshinione inhibits β-amyloid aggregation and protects damage from β-amyloid in SH-SY5Y cells. Neurochem Res 37(3):622–628. https://doi.org/10.1007/s11064-011-0652-6
Wu JS, Meng QY, Shi XH, Liu LX, Zhang ZK, Guan HS, Shao CL, Wang CY (2020) The oxygenated products of cryptotanshinone by biotransformation with Cunninghamella elegans exerting anti-neuroinflammatory effects by inhibiting TLR 4-mediated MAPK signaling pathway. Bioorg Chem 104:104246. https://doi.org/10.1016/j.bioorg.2020.104246
Durairajan SS, Liu LF, Lu JH, Koo I, Maruyama K, Chung SK, Huang JD, Li M (2011) Stimulation of non-amyloidogenic processing of amyloid-β protein precursor by cryptotanshinone involves activation and translocation of ADAM10 and PKC-α. J Alzheimer’s Dis 25(2):245–262. https://doi.org/10.3233/jad-2011-102085
Lu M, Zhou Y, Li X, Sun Q, Guo J, Wu B, Wu M (2021) Research on regularity of traditional Chinese medicine in treatment of Alzheimer’s disease based on data mining. China J Chin Mater Med 46(06):1558–1563. https://doi.org/10.19540/j.cnki.cjcmm.20200611.502
Ru J, Li P, Wang J, Zhou W, Li B, Huang C, Li P, Guo Z et al (2014) TCMSP: a database of systems pharmacology for drug discovery from herbal medicines. J Cheminform 6:13. https://doi.org/10.1186/1758-2946-6-13
Piñero J, Bravo À, Queralt-Rosinach N, Gutiérrez-Sacristán A, Deu-Pons J, Centeno E, García-García J, Sanz F et al (2017) DisGeNET: a comprehensive platform integrating information on human disease-associated genes and variants. Nucleic Acids Res 45(D1):D833-d839. https://doi.org/10.1093/nar/gkw943
Zhang H, Jia L, Jia J (2020) Oxiracetam Offers Neuroprotection by Reducing Amyloid β-Induced Microglial Activation and Inflammation in Alzheimer’s Disease. Front Neurol 11:623. https://doi.org/10.3389/fneur.2020.00623
Razani E, Pourbagheri-Sigaroodi A, Safaroghli-Azar A, Zoghi A, Shanaki-Bavarsad M, Bashash D (2021) The PI3K/Akt signaling axis in Alzheimer’s disease: a valuable target to stimulate or suppress? Cell Stress Chaperones 26(6):871–887. https://doi.org/10.1007/s12192-021-01231-3
Singh AK, Kashyap MP, Tripathi VK, Singh S, Garg G, Rizvi SI (2017) Neuroprotection Through Rapamycin-Induced Activation of Autophagy and PI3K/Akt1/mTOR/CREB Signaling Against Amyloid-β-Induced Oxidative Stress, Synaptic/Neurotransmission Dysfunction, and Neurodegeneration in Adult Rats. Mol Neurobiol 54(8):5815–5828. https://doi.org/10.1007/s12035-016-0129-3
Gabbouj S, Ryhänen S, Marttinen M, Wittrahm R, Takalo M, Kemppainen S, Martiskainen H, Tanila H et al (2019) Altered Insulin Signaling in Alzheimer’s Disease Brain - Special Emphasis on PI3K-Akt Pathway. Front Neurosci 13:629. https://doi.org/10.3389/fnins.2019.00629
Seshacharyulu P, Pandey P, Datta K, Batra SK (2013) Phosphatase: PP2A structural importance, regulation and its aberrant expression in cancer. Cancer Lett 335(1):9–18. https://doi.org/10.1016/j.canlet.2013.02.036
Kamat PK, Rai S, Nath C (2013) Okadaic acid induced neurotoxicity: an emerging tool to study Alzheimer’s disease pathology. Neurotoxicology 37:163–172. https://doi.org/10.1016/j.neuro.2013.05.002
Ma XH, Duan WJ, Mo YS, Chen JL, Li S, Zhao W, Yang L, Mi SQ et al (2018) Neuroprotective effect of paeoniflorin on okadaic acid-induced tau hyperphosphorylation via calpain/Akt/GSK-3β pathway in SH-SY5Y cells. Brain Res 1690:1–11. https://doi.org/10.1016/j.brainres.2018.03.022
Li Y, Dai S, Huang N, Wu J, Yu C, Luo Y (2021) Icaritin and icariin reduce p-Tau levels in a cell model of Alzheimer’s disease by downregulating glycogen synthase kinase 3β. Biotechnol Appl Biochem. https://doi.org/10.1002/bab.2114
Tu S, Okamoto S, Lipton SA, Xu H (2014) Oligomeric Aβ-induced synaptic dysfunction in Alzheimer’s disease. Mol Neurodegener 9:48. https://doi.org/10.1186/1750-1326-9-48
Ittner LM, Ke YD, Delerue F, Bi M, Gladbach A, van Eersel J, Wölfing H, Chieng BC et al (2010) Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer’s disease mouse models. Cell 142(3):387–397. https://doi.org/10.1016/j.cell.2010.06.036
Becher A, Drenckhahn A, Pahner I, Margittai M, Jahn R, Ahnert-Hilger G (1999) The synaptophysin-synaptobrevin complex: a hallmark of synaptic vesicle maturation. J Neuroscience 19(6):1922–1931. https://doi.org/10.1523/jneurosci.19-06-01922.1999
El-Husseini AE, Schnell E, Chetkovich DM, Nicoll RA, Bredt DS (2000) PSD-95 involvement in maturation of excitatory synapses. Science (New York, NY) 290(5495):1364–1368
Carreiras MC, Mendes E, Perry MJ, Francisco AP, Marco-Contelles J (2013) The multifactorial nature of Alzheimer’s disease for developing potential therapeutics. Curr Top Med Chem 13(15):1745–1770. https://doi.org/10.2174/15680266113139990135
Zhu CW, Livote EE, Scarmeas N, Albert M, Brandt J, Blacker D, Sano M, Stern Y (2013) Long-term associations between cholinesterase inhibitors and memantine use and health outcomes among patients with Alzheimer’s disease. Alzheimer’s Dement 9(6):733–740. https://doi.org/10.1016/j.jalz.2012.09.015
Lopez OL, Becker JT, Wahed AS, Saxton J, Sweet RA, Wolk DA, Klunk W, Dekosky ST (2009) Long-term effects of the concomitant use of memantine with cholinesterase inhibition in Alzheimer disease. J Neurol Neurosurg Psychiatry 80(6):600–607. https://doi.org/10.1136/jnnp.2008.158964
Li S, Wu Z, Le W (2021) Traditional Chinese medicine for dementia. Alzheimer’s Dement 17(6):1066–1071. https://doi.org/10.1002/alz.12258
Fang J, Wang L, Wu T, Yang C, Gao L, Cai H, Liu J, Fang S et al (2017) Network pharmacology-based study on the mechanism of action for herbal medicines in Alzheimer treatment. J Ethnopharmacol 196:281–292. https://doi.org/10.1016/j.jep.2016.11.034
Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI (1986) Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci USA 83(13):4913–4917. https://doi.org/10.1073/pnas.83.13.4913
Qi Y, Jing H, Cheng X, Yan T, Xiao F, Wu B, Bi K, Jia Y (2020) Alpinia oxyphylla-Schisandra chinensis Herb Pair Alleviates Amyloid-β Induced Cognitive Deficits via PI3K/Akt/Gsk-3β/CREB Pathway. NeuroMol Med 22(3):370–383. https://doi.org/10.1007/s12017-020-08595-2
Zhang LF, Zhou ZW, Wang ZH, Du YH, He ZX, Cao C, Zhou SF (2015) Coffee and caffeine potentiate the antiamyloidogenic activity of melatonin via inhibition of Aβ oligomerization and modulation of the Tau-mediated pathway in N2a/APP cells. Drug Des Dev Ther 9:241–272. https://doi.org/10.2147/dddt.S71106
Lin CI, Chang YC, Kao NJ, Lee WJ, Cross TW, Lin SH (2020) 1,25(OH)(2)D(3) Alleviates Aβ(25–35)-Induced Tau Hyperphosphorylation, Excessive Reactive Oxygen Species, and Apoptosis Through Interplay with Glial Cell Line-Derived Neurotrophic Factor Signaling in SH-SY5Y Cells. Int J Mol Sci 21(12):4215. https://doi.org/10.3390/ijms21124215
Sun ZK, Yang HQ, Pan J, Zhen H, Wang ZQ, Chen SD, Ding JQ (2008) Protective effects of erythropoietin on tau phosphorylation induced by beta-amyloid. J Neurosci Res 86(13):3018–3027. https://doi.org/10.1002/jnr.21745
Wang C, Hao J, Liu X, Li C, Yuan X, Lee RJ, Bai T, Wang D (2020) Isoforsythiaside Attenuates Alzheimer’s Disease via Regulating Mitochondrial Function Through the PI3K/AKT Pathway. Int J Mol Sci 21(16):5687. https://doi.org/10.3390/ijms21165687
Chou CH, Yang CR (2021) Neuroprotective Studies of Evodiamine in an Okadaic Acid-Induced Neurotoxicity. Int J Mol Sci 22(10):5347. https://doi.org/10.3390/ijms22105347
Jiang W, Luo T, Li S, Zhou Y, Shen XY, He F, Xu J, Wang HQ (2016) Quercetin Protects against Okadaic Acid-Induced Injury via MAPK and PI3K/Akt/GSK3β Signaling Pathways in HT22 Hippocampal Neurons. PLoS ONE 11(4):e0152371. https://doi.org/10.1371/journal.pone.0152371
Ma RH, Zhang Y, Hong XY, Zhang JF, Wang JZ, Liu GP (2017) Role of microtubule-associated protein tau phosphorylation in Alzheimer’s disease. J Huazhong Univ Sci Technolog Med Sci 37(3):307–312. https://doi.org/10.1007/s11596-017-1732-x
Kumar M, Bansal N (2021) Implications of Phosphoinositide 3-Kinase-Akt (PI3K-Akt) Pathway in the Pathogenesis of Alzheimer’s Disease. Mol Neurobiol. https://doi.org/10.1007/s12035-021-02611-7
Wang JZ, Gong CX, Zaidi T, Grundke-Iqbal I, Iqbal K (1995) Dephosphorylation of Alzheimer paired helical filaments by protein phosphatase-2A and -2B. J Biol Chem 270(9):4854–4860. https://doi.org/10.1074/jbc.270.9.4854
Iqbal K, Grundke-Iqbal I (2008) Alzheimer neurofibrillary degeneration: significance, etiopathogenesis, therapeutics and prevention. J Cell Mol Med 12(1):38–55. https://doi.org/10.1111/j.1582-4934.2008.00225.x
Zhang H, Wang X, Xu P, Ji X, Chi T, Liu P, Zou L (2020) Tolfenamic acid inhibits GSK-3β and PP2A mediated tau hyperphosphorylation in Alzheimer’s disease models. J Physiol Sci 70(1):29. https://doi.org/10.1186/s12576-020-00757-y
Huang L, Lin M, Zhong X, Yang H, Deng M (2019) Galangin decreases p-tau, Aβ42 and β-secretase levels, and suppresses autophagy in okadaic acid-induced PC12 cells via an Akt/GSK3β/mTOR signaling-dependent mechanism. Mol Med Rep 19(3):1767–1774. https://doi.org/10.3892/mmr.2019.9824
Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, Hansen LA, Katzman R (1991) Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol 30(4):572–580. https://doi.org/10.1002/ana.410300410
Yin X, Qiu Y, Zhao C, Zhou Z, Bao J, Qian W (2021) The Role of Amyloid-Beta and Tau in the Early Pathogenesis of Alzheimer’s Disease. Med Sci Monit 27:e933084. https://doi.org/10.12659/msm.933084
Dejanovic B, Huntley MA, De Mazière A, Meilandt WJ, Wu T, Srinivasan K, Jiang Z, Gandham V et al (2018) Changes in the Synaptic Proteome in Tauopathy and Rescue of Tau-Induced Synapse Loss by C1q Antibodies. Neuron 100(6):1322-1336.e1327. https://doi.org/10.1016/j.neuron.2018.10.014
Oakley H, Cole SL, Logan S, Maus E, Shao P, Craft J, Guillozet-Bongaarts A, Ohno M et al (2006) Intraneuronal beta-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer’s disease mutations: potential factors in amyloid plaque formation. J Neuroscience 26(40):10129–10140. https://doi.org/10.1523/jneurosci.1202-06.2006
Mardones MD, Jorquera PV, Herrera-Soto A, Ampuero E, Bustos FJ, van Zundert B, Varela-Nallar L (2019) PSD95 regulates morphological development of adult-born granule neurons in the mouse hippocampus. J Chem Neuroanat 98:117–123. https://doi.org/10.1016/j.jchemneu.2019.04.009
Zhao JP, Murata Y, Constantine-Paton M (2013) Eye opening and PSD95 are required for long-term potentiation in developing superior colliculus. Proc Natl Acad Sci USA 110(2):707–712. https://doi.org/10.1073/pnas.1215854110
Bustos FJ, Ampuero E, Jury N, Aguilar R, Falahi F, Toledo J, Ahumada J, Lata J et al (2017) Epigenetic editing of the Dlg4/PSD95 gene improves cognition in aged and Alzheimer’s disease mice. Brain: J Neurol 140(12):3252–3268. https://doi.org/10.1093/brain/awx272
Calhoun ME, Jucker M, Martin LJ, Thinakaran G, Price DL, Mouton PR (1996) Comparative evaluation of synaptophysin-based methods for quantification of synapses. J Neurocytol 25(12):821–828. https://doi.org/10.1007/bf02284844
Ferreira A, Chin LS, Li L, Lanier LM, Kosik KS, Greengard P (1998) Distinct roles of synapsin I and synapsin II during neuronal development. Mol Med 4(1):22–28
Sze CI, Troncoso JC, Kawas C, Mouton P, Price DL, Martin LJ (1997) Loss of the presynaptic vesicle protein synaptophysin in hippocampus correlates with cognitive decline in Alzheimer disease. J Neuropathol Exp Neurol 56(8):933–944. https://doi.org/10.1097/00005072-199708000-00011
Fan W, Zhang Y, Li X, Xu C (2021) S-oxiracetam Facilitates Cognitive Restoration after Ischemic Stroke by Activating α7nAChR and the PI3K-Mediated Pathway. Neurochem Res 46(4):888–904. https://doi.org/10.1007/s11064-021-03233-0
Lian WW, Zhou W, Zhang BY, Jia H, Xu LJ, Liu AL, Du GH (2021) DL0410 ameliorates cognitive disorder in SAMP8 mice by promoting mitochondrial dynamics and the NMDAR-CREB-BDNF pathway. Acta Pharmacol Sin 42(7):1055–1068. https://doi.org/10.1038/s41401-020-00506-2
Katsuse O, Lin WL, Lewis J, Hutton ML, Dickson DW (2006) Neurofibrillary tangle-related synaptic alterations of spinal motor neurons of P301L tau transgenic mice. Neurosci Lett 409(2):95–99. https://doi.org/10.1016/j.neulet.2006.09.021
Kopeikina KJ, Wegmann S, Pitstick R, Carlson GA, Bacskai BJ, Betensky RA, Hyman BT, Spires-Jones TL (2013) Tau causes synapse loss without disrupting calcium homeostasis in the rTg4510 model of tauopathy. PLoS ONE 8(11):e80834. https://doi.org/10.1371/journal.pone.0080834
Leuba G, Walzer C, Vernay A, Carnal B, Kraftsik R, Piotton F, Marin P, Bouras C et al (2008) Postsynaptic density protein PSD-95 expression in Alzheimer’s disease and okadaic acid induced neuritic retraction. Neurobiol Dis 30(3):408–419. https://doi.org/10.1016/j.nbd.2008.02.012
Xu AH, Yang Y, Sun YX, Zhang CD (2018) Exogenous brain-derived neurotrophic factor attenuates cognitive impairment induced by okadaic acid in a rat model of Alzheimer’s disease. Neural Regen Res 13(12):2173–2181. https://doi.org/10.4103/1673-5374.241471
Acknowledgements
We wish to thank Dr. Heng Zhang, Dr. Yan Li, Dr. Yuqing Shi for their selfless help on performing experiments and suggestions on revising the manuscript. We wish to thank Yana Pang and Bingqiu Li for their guidance.
Funding
This study was supported by the Innovation Center for Neurological Disorders and Department of Neurology, Xuanwu Hospital. This study was supported by the Key Project of the National Natural Science Foundation of China (81530036), the National Key Scientific Instrument and Equipment Development Project (31627803), Beijing Scholars Program, Beijing Brain Initiative from Beijing Municipal Science and Technology Commission (Z2011000 05520016 and Z201100005520017), and the Key Project of the National Natural Science Foundation of China (U20A20354).
Author information
Authors and Affiliations
Contributions
JJ contributed to the research concept and the study design. DL designed the study, performed experiments, analyzed data, drawn figures, and wrote the manuscript. JJ revised the manuscript critically and obtained funding. All authors contributed to the article and approved the submitted manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lyu, D., Jia, J. Cryptotanshinone Attenuates Amyloid-β42-induced Tau Phosphorylation by Regulating PI3K/Akt/GSK3β Pathway in HT22 Cells. Mol Neurobiol 59, 4488–4500 (2022). https://doi.org/10.1007/s12035-022-02850-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02850-2