Abstract
Schizophrenia is a severe and highly heritable neuropsychiatric disorder. Recent genetic analyses including genome-wide association studies (GWAS) have implicated multiple genome-wide significant variants for schizophrenia among European populations. However, many of these risk variants were not largely validated in other populations of different ancestry such as Asians. To validate whether these European GWAS significant loci are associated with schizophrenia in Asian populations, we conducted a systematic literature search and meta-analyses on 19 single nucleotide polymorphisms (SNPs) in Asian populations by combining all available case-control and family-based samples, including up to 30,000 individuals. We employed classical fixed (or random) effects inverse variance weighted methods to calculate summary odds ratios (ORs) and 95 % confidence intervals (CIs). Among the 19 GWAS loci, we replicated the risk associations of nine markers (e.g., SNPs at VRK2, ITIH3/4, NDST3, NOTCH4) surpassing significance level (two-tailed P < 0.05), and three additional SNPs in MIR137 and ZNF804A also showed trend associations (one-tailed P < 0.05). These risk associations are in the same directions of allelic effects between Asian replication samples and initial European GWAS findings, and the successful replications of these GWAS loci in a different ethnic group provide stronger evidence for their clinical associations with schizophrenia. Further studies, focusing on the molecular mechanisms of these GWAS significant loci, will become increasingly important for understanding of the pathogenesis to schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a complex psychiatric disorder which involves multiple susceptibility variants [1]. The lifetime prevalence of schizophrenia is about 0.5–1.5 % in general populations worldwide [2]. Previous family, twin, and adoption studies have implicated a strong genetic component in the risk of schizophrenia, and the heritability has been estimated to be about 80 % [3]. These findings imply that the application of genetic analyses in schizophrenia is plausible and timely. Recent genome-wide association studies (GWAS) have provided unbiased assessments of common sequence variations across the whole genome and may robustly map the loci involved in the pathology of complex diseases such as schizophrenia.
In the past 10 years, a number of GWAS of schizophrenia have been published. Briefly, after the identification of a genome-wide significant locus rs1344706 at ZNF804A mainly in European populations by O’Donovan et al. [4], later GWAS by Stefansson et al. [5] in European populations discovered single nucleotide polymorphisms (SNPs) at major histocompatibility complex (MHC) region, NRGN, TCF4 and VRK2 showing genome-wide significance. There are also additional GWAS using independent primary screening samples and identified other genome-wide significant risk loci, such as rs11819869 in AMBRA1 and rs11098403 in NDST3 [6, 7]. In 2011, the Schizophrenia Psychiatric Genomics Consortium (PGC) has reported a large schizophrenia GWAS in Europeans [8]. In this study, the authors conducted a meta-analysis of the combined GWAS genotyping data from 21,856 individuals of European ancestry from 17 separate studies and then performed a replication study in a total of 29,839 participants from 19 samples on the top hits. This GWAS study revealed seven risk regions showing genome-wide significance, including two previously reported loci (MHC region and TCF4) and the other five novel loci: 1p23.3 (MIR137), 2q32.3 (PCGEM1), 8p23.2 (CSMD1), 8q21.3 (MMP16), and a broad 10q24.32–q24.33 region. Subsequently, Hamshere et al. [9] tested 78 of the 81 SNPs highlighted by the PGC1 [8] in an independent UK “CLOZUK” sample and replicated significant associations for 37 of the SNPs. Remarkably, in their study, genetic variants in three novel loci (ITIH3/4, CACNA1C, and SDCCAG8) reached genome-wide significance after combining the new schizophrenia data with those of the PGC1 [9]. Later in 2013, the PGC performed a second-stage GWAS by adding more genome-wide data from Swedish samples and reported 13 new schizophrenia risk loci including TSNARE1 and ZEB2 [10]. In 2014, the PGC conducted the largest scale GWAS (named PGC2) in 36,989 schizophrenia cases and 113,075 controls and identified 128 independent risk associations spanning 108 conservatively defined loci that meet genome-wide significance [1].
These promising GWAS findings of common variants further support the theory of “common disease-common variations” and make impressive progresses in the dissection for the genetic architectures of schizophrenia. However, most of these genetic discoveries were obtained via studies in European samples but not yet largely validated across populations of different ancestry, such as Asians. Regarding schizophrenia, many of the risk associations are population specific; but in some cases, the associations may exhibit convergence of risk genes or even same risk alleles across populations. Recognition of shared genetic risk components across different ethnic groups is vital and necessary for our understanding mechanism of common pathogenesis to schizophrenia and discovery of potential therapeutic and drug targets. It is therefore of great interest to investigate whether the European GWAS risk loci are also associated with schizophrenia in Asian populations.
After the European GWAS, several subsequent studies attempted to replicate some of the specific GWAS loci in Asian samples [11–13], but the results varied between individual samples, such as rs1344706 in ZNF804A [13, 14]. The inconsistent replications across samples were not surprising given the different methodologies utilized in each study. More importantly, it should be noted that most schizophrenia risk SNPs exhibit small effect sizes and collectively explain only a small fraction of heritable variation. Replication analyses, especially in small samples, would easily lead to a false negative result (i.e., type II error) given the lack of statistical power compared to the initial larger GWAS. By using all available data to increase statistical power, it is hypothesized that meta-analysis might allow plausible candidate risk genes to be identified (or excluded) with reliability. Therefore, to give a more conclusive answer regarding whether the European GWAS loci confer risk of schizophrenia in Asians as well, we conducted a comprehensive literature search and noticed that 19 GWAS SNPs have been studied in two or more individual Asian samples. We then utilized the genetic data from multiple independent Asian samples to perform a systematic meta-analysis of these GWAS loci in up to 30,000 individuals.
Methods
Search Strategy
We have comprehensively read through all published schizophrenia GWAS in European populations, and the genome-wide significant variants that are also polymorphic in Asians are potential candidates for our meta-analyses. These candidate variants were then searched via PubMed (1966–present), Web of Science (1899–present), Embase (1974–present), and CNKI (www.cnki.net) to examine if they have ever been studied in Asian populations. Such searching strategy returned considerable replication studies of schizophrenia loci, but other studies that conducted analysis of multiple SNPs without showing individual SNP name in either titles or abstracts should also be considered. In order for this, we carefully examined all the replication studies of schizophrenia risk loci in Asian populations, especially for those studies analyzing many SNPs at one time. Once these records were collected, their bibliographies were then retrieved for additional references. All articles identified through the search were evaluated based on the titles and abstracts. Clearly, irrelevant studies were excluded from further consideration. The remaining articles received a full-text review. The last search was performed on January 29, 2016.
Eligibility Criteria
The following criteria were set for eligible studies in the meta-analysis: (1) Case-control or family-based studies were included, while case-only studies were excluded; (2) eligible studies should have case status defined with having a diagnosis of schizophrenia according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) or the International Classification of Diseases 10 (ICD-10), while control subjects having no history of mental or other neurological disorder, alcohol dependence, or drug dependence; (3) only studies having no overlap with the other included studies were eligible; and (4) other factors such as Hardy-Weinberg equilibrium (P < 0.05) among healthy control samples were also considered.
Data Extraction
The data from each study was extracted using a standardized data extraction form. Descriptive information was extracted from each study including (1) basic information with the name of the first author and year of publication; (2) methods including study design, sample size, and definition of case status; (3) sample characteristics such as collection area, gender ratio, and mean age; and (4) results for the GWAS loci (odds ratio (OR), standard error (SE), and P value). Where the required data were not available in the published study or from web-based supplementary information, we contacted the authors of the studies by email to request access to the data.
Assessment of Publication Bias
A Begg’s funnel plot was made using “metafor” package in R to examine if there is any publication bias among the selected studies. In brief, the plot shows the observed effect sizes (i.e., OR) on the X-axis against some measure of precision (e.g., SE) of the observed OR on the Y-axis. In the absence of publication bias, one would then expect to see the points forming a funnel shape, with the majority of the points falling inside of the pseudo-confidence region with bounds OR ± 1.96SE. With other measures of precision (e.g., variance) for the Y-axis, the expected shape of the funnel can be different.
Statistical Analysis
We used OR and SE from each individual study to estimate heterogeneity between samples and to calculate the pooled OR and 95 % confidence interval (CI) in the combined samples. To combine the results from individual sample, we used the Cochran’s (Q) χ 2 test to calculate the heterogeneity between studies. This test is a weighted sum of the squares of deviations of individual OR estimates from the overall estimate. When the ORs were homogeneous, Q followed a χ 2 distribution with degrees of freedom, while otherwise, ORs were heterogeneous. If P Q < 0.10, the heterogeneity was considered statistically significant. In the presence of heterogeneity among individual studies, we used random effects models to combine the samples and to calculate the OR and the corresponding 95 % CIs; for homogeneous studies, a fixed-effect model was used. The meta-analyses were performed using the classical inverse variance weighted methods. The pooled ORs and the 95 % CIs were graphically presented using a forest plot. Each study and its weight were represented by a square with the corresponding size in the plot.
“Leave-one-out” sensitivity analysis was conducted to assess the potential influences of any one single study on the pooled ORs. Within each meta-analysis, included studies were removed one at a time to check for significant alterations to pooled ORs and associated P values.
Results
Literature Search and Eligible Studies
A flowchart describing the literature search and selection process is presented in Fig. 1. After a comprehensive examination of European GWAS, we identified that 19 European GWAS SNPs have ever been analyzed in two or more Asian samples; thus, we selected these 19 SNPs into our meta-analysis, including loci at SDCCAG8, MIR137, ZNF804A, VRK2, ZEB2, ITIH3/4, NDST3, NOTCH4, CSMD1, MMP16, TSNARE1, CNNM2, NT5C2, AMBRA1, NRGN, and CACNA1C. The original statistics of European GWAS reports of the 19 SNPs are shown in Table 1.
Briefly, the initial literature search identified 98 references of these 19 GWAS SNPs. After removing 24 references with obviously irrelevant titles, the abstracts of the rest 74 references were then screened, leaving 54 potentially eligible studies in Asian populations. The full texts of the 54 literatures were reviewed to examine their eligibilities based on the inclusion and exclusion criteria. Among them, 10 studies were further excluded due to overlapped samples or data unavailable from the publications. Therefore, 44 independent studies were then considered eligible for the present meta-analysis. Characteristics of the included Asian samples for each GWAS SNP are listed in Tables S1–S19, including collection area, sample size, mean age and gender ratio, etc.
Before performing meta-analysis, publication bias on each SNP was assessed according to the Begg’s funnel plot through using metafor package in R, as described in our previous studies [15, 16]. None of the analyzed SNPs showed significant publication bias (data not shown), which is suitable for meta-analysis.
VRK2 rs2312147
In 2009, by conducting a GWAS in European populations, Stefansson et al. [5] reported several SNPs conferring risk of schizophrenia in 47,536 subjects, and rs2312147 located about 50 kb upstream of VRK2 was identified as a potential susceptibility SNP (P = 3.0 × 10−7). In 2011, Steinberg et al. [17] confirmed this association in a larger European sample (N = 60,742, P = 1.9 × 10−9). In the present study, our meta-analysis included six independent Asian samples (Table S1) comprising of a total of 3431 schizophrenia patients and 5215 healthy controls, and the results showed that rs2312147 was significantly associated with schizophrenia (P = 8.52 × 10−3, OR = 1.177, 95 % CIs = 1.042–1.329). Of note, we used to report a meta-analysis of positive associations for rs2312147 in smaller Asian samples [18], and in this larger meta-analysis with increasing sample size (containing two additional cohorts), we further confirmed the associations of rs2312147 with schizophrenia. The forest plot of the meta-analysis for rs2312147 is presented in Fig. 2a. Although the sample size in Asians is smaller compared with that in European groups, the effect sizes (i.e., OR) are similar between these populations (OR = 1.177 in Asians versus OR = 1.090 in Europeans), suggesting that rs2312147 is likely a common risk SNP for schizophrenia in both populations. A meta-analysis including both Asian and European samples showed a genome-wide significant association of rs2312147 with schizophrenia (P = 7.25 × 10−15, OR = 1.104, Figure S1).
However, it should be noted that the test of heterogeneity among individual samples for rs2312147 yielded a nominal significant association (P = 0.03, I 2 = 60 %), which is an indication of potential heterogeneity between these samples. To identify the possible explanations for this heterogeneity, we performed leave-one-out sensitivity analysis, which omitted one study each time, and re-analyzed using the remaining samples. This analysis showed that removal of any individual sample did not alter the meta-analytic results significantly (data not shown); more importantly, when the sample from Saito et al. (2014) study was omitted, test of heterogeneity became non-significant (P heterogeneity > 0.10, I 2 = 48 %), and meta-analysis using the remaining samples still yielded significant associations (P = 1.36 × 10−3, OR = 1.223). Saito et al. (2014) used a case-control sample from Japanese ancestry, while other included samples were mainly from Chinese population. Although the allele frequencies of rs2312147 between Japanese and Chinese are similar (C allele, 0.716 versus 0.714), other possibilities such as different genetic background, environmental factors, and phenotypic heterogeneity may also lead to the inconsistent associations between regional Asian populations.
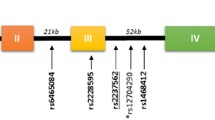
ITIH3/4 rs2239547
In 2012, Hamshere et al. [9] performed an association analysis of the PGC1 GWAS [8] top hits in their CLOZUK sample of European ancestry, and their study identified several novel risk loci for schizophrenia including rs2239547 in ITIH3/4. In 2015, Li and colleagues successfully replicated the rs2239547’s association in a Chinese case-control sample (P = 1.17 × 10−10 in 3585 cases and 5496 controls) [11]. In this meta-analysis, in addition to Li’s sample, we also collected three additional Asian samples (including two family-based and one case-control cohorts), and the meta-analytic results in the four combined samples (including a total of 4617 cases, 6489 controls, and 1115 families, Table S2) yielded a genome-wide significant association (P = 9.29 × 10−12, OR = 1.194, 95 % CIs = 1.135–1.256) without any heterogeneity (P heterogeneity = 0.4, I 2 = 0). To exclude the possibility that this significant association might be caused by Li et al.’s data [11], we then conducted a leave-one-out sensitivity analysis. This analysis showed that even after removal of Li et al.’s data, meta-analysis using the remaining Asian samples still yielded a significant association (P = 0.0052, OR = 1.127), supporting the conclusion that rs2239547 is likely an authentic risk SNP for schizophrenia in Asian populations. The forest plot of the meta-analysis is presented in Fig. 2b. We also performed a meta-analysis by combining both Asian and European samples and identified a genome-wide significant association of rs2239547 with schizophrenia (P = 9.03 × 10−20, OR = 1.142, Figure S2). Notably, rs2239547 is located in an extensive linkage disequilibrium (LD) block region that contained many genes and numerous high-linked SNPs [9]. In addition to schizophrenia, these risk loci also confer risk of bipolar disorder [19–21]. Although showing strong associations with broader psychosis spectrum, the underlying molecular mechanism of these risk associations are yet to be determined. Previous studies have shown that the risk SNPs are associated with expression of GLT8D1, ITIH4, or STAB1 in different studies [20, 22], and further investigations are needed.
NDST3 rs11098403
In 2013, Lencz et al. conducted a GWAS in a Ashkenazi Jewish case-control sample followed by independent replications in diverse datasets and identified a SNP rs11098403 in NDST3 showing genome-wide significant association with schizophrenia [7]. Recently, two individual small replication studies in Chinese samples confirmed the association [23, 24], and in this meta-analysis, we included two additional Asian cohorts, resulting in a total of six independent samples that comprised of 2654 schizophrenia patients and 2898 healthy controls (Table S3). This meta-analysis showed a significant association between rs11098403 and schizophrenia in Asian samples (P = 9.50 × 10−8, OR = 1.300, 95 % CIs = 1.180–1.431). The forest plot of the meta-analysis is presented in Fig. 2c.
We note that there is nominal significant heterogeneity between these included samples (P = 0.02, I 2 = 63 %). We thus performed leave-one-out sensitivity analysis through removing each sample at one time. This analysis showed that removal of any individual sample did not alter the meta-analytic results significantly (data not shown); more importantly, when the sample from Lencz et al. (2013) study was omitted, test of heterogeneity became non-significant (P = 0.42, I 2 = 0), and meta-analysis using the remaining samples still yielded significant associations (P = 8.25 × 10−10, OR = 1.458). Lencz et al. (2013) used a case-control sample from Japanese ancestry, while other included samples were all from Chinese population, suggesting a potential genetic heterogeneity between regional Asian populations on this genetic locus.
NOTCH4 rs3131296
In 2009, by a GWAS study in 47,536 subjects of European descent, Stefansson et al. found rs3131296 within NOTCH4 gene (in the MHC region) conferring risk of schizophrenia (P = 2.30 × 10−10, OR = 1.190) [5]. This association was previously replicated by Li et al. study in a Han Chinese case-control sample [25], but negative association has also been observed [26]. A likely reason for the inconsistent replications in Asians is the lower frequency of rs3131296 in this population (minor allele frequency (MAF) is 0.031 in Asians), which is different from that in Europeans (MAF is 0.103) (Table 1), and thus requires larger samples to obtain more stable results. This meta-analysis includes six independent Asian case-control samples, yielding a total of 4657 schizophrenia patients and 8247 healthy controls (Table S4), and results in a significant association (P = 2.91 × 10−6, OR = 1.345, 95 % CIs = 1.188–1.522). The forest plot of the meta-analysis is presented in Fig. 2d. After adding the data from Stefansson et al. study in Europeans [5], rs3131296 shows a stronger association with schizophrenia (P = 1.63 × 10−13, OR = 1.213). Although it has been reported that there is visible population differentiation on the MHC loci between European and Asian samples, rs3131296 in NOTCH4 is likely a common risk SNP for schizophrenia in both populations. Of note, another NOTCH4 SNP rs2071287, which is in low LD with rs3131296 in Asians (r 2 = 0), though not analyzed in the present study, showed genome-wide significant association with schizophrenia in Japanese populations (P = 3.40 × 10−8) [27] and is also significantly associated with schizophrenia in a recent GWAS mainly including European descent (P = 7.46 × 10−7) [1]. These convergent lines of evidence suggest that NOTCH4 remains one of the strongest candidate susceptibility genes for schizophrenia.
10q24.32−33 Region
In 2011, the PGC1 GWAS reported SNPs in 10q24.32−33 region significantly associated with schizophrenia in European populations, including CNNM2 rs7914558 and NT5C2 rs11191580 [8], and this genomic region remains one of the most significant loci for schizophrenia in the later larger GWAS of schizophrenia in European populations [1, 10]. In our meta-analysis of Asian samples, rs7914558 shows a nominal significant association with schizophrenia in a total of 4092 cases, 3572 controls, and 1115 families (P = 2.96 × 10−2, OR = 1.059, 95 % CIs = 1.006–1.116, Table S5), and rs11191580 is also significantly associated with schizophrenia in Asian samples comprising of 12,580 cases, 17,837 controls, and 1115 families (P = 1.24 × 10−4, OR = 1.074, 95 % CIs = 1.036–1.115, Table S6). Both SNPs are in the same consistency with the results in PGC European GWAS [8]. Notably, rs7914558 and rs11191580 are in low LD in Asian populations (r 2 = 0.186), suggesting that they are likely independent association signals in this genomic region. The meta-analysis of rs11191580 is also one of the largest scale study on schizophrenia risk genes ever analyzed in Asian populations. The forest plots of the meta-analyses are presented in Fig. 3.
CACNA1C Variants
CACNA1C (12p13.3) has been implicated as a susceptibility gene for schizophrenia by several GWAS in Europeans [1, 9, 10]. Three SNPs (rs1006737, rs4765905, and rs2007044) in CACNA1C showed genome-wide significant associations in different studies respectively [1, 9, 10]. Among these three SNPs in Europeans, rs1006737 and rs4765905 are in perfect LD (r 2 = 1.000), while rs2007044 shows modest LD with them (both r 2 = 0.788). In Asian populations, rs1006737 and rs4765905 are still in high LD (r 2 = 1.000), but rs2007044 is in low LD with the two SNPs (both r 2 = 0.168). Intriguingly, these three SNPs (Tables S7–S9) are all significantly associated with schizophrenia in the meta-analyses of Asian samples (P < 0.05). The ORs of rs1006737 and rs4765905 in Asian meta-analyses are similar, but the included sample sizes for each SNP are not identical, resulting in the differences of associating P values. The forest plots of the meta-analyses of these SNPs are presented in Fig. 4.
MIR137 GWAS SNPs
MIR137 locus is one of the strongest association signals outside of the MHC region in PGC schizophrenia GWAS [1, 8, 10], and two SNPs (rs1625579 and rs1198588) in high LD (r 2 = 0.778 in Europeans) in this genomic region have been reported as the top risk loci in different GWAS, respectively [8, 10]. In Asian populations, rs1625579 and rs1198588 are in modest LD (r 2 = 0.655) and both have been analyzed in several samples (Tables S10–S11). In this meta-analyses, these two SNPs are in marginal associations with schizophrenia (rs1625579, P = 0.059 in 4552 cases, 4696 controls, and 579 families; rs1198588, P = 0.097 in 7419 cases, 12,027 controls, and 579 families) with the same direction of allelic effects as European GWAS results. The forest plots of the meta-analyses are presented in Fig. 5. Considering the relative large samples we used, the MIR137 might confer a smaller effect of risk for schizophrenia in Asians compared with in European populations.
Other GWAS Loci
We also analyzed eight additional SNPs in other genes that showed genome-wide significance in European GWAS studies (Tables S12–S19). Among these eight SNPs, rs1344706 in ZNF804A, which has been analyzed in multiple Asian samples (Table S12), was marginally associated with schizophrenia in our meta-analyses including a total of 13,542 cases, 17,826 controls, and 680 families (Figure S3). However, the other seven SNPs were not associated with schizophrenia in our meta-analyses of Asian populations (Figures S4–S10). These inconsistencies might be due to either genetic heterogeneity on these GWAS loci between continental populations or other potential confounding factors, such as phenotypic heterogeneity.
Discussion
The understanding about genetic architectures of schizophrenia has greatly increased during recent years. As of now, many common risk alleles have been reported in large-scale association studies [1]. However, a major rising problem in genetic studies of schizophrenia is that risk polymorphisms identified in one population are not always reproducible in another population. Moreover, the fact that most common risk variants show relatively low effect size in the risk of mental illnesses calls for large samples with sufficient statistical power and extensive international collaborations. As a result, pooling data from a range of studies via meta-analysis has been successful in understanding the risk of certain SNPs in schizophrenia.
In this comprehensive meta-analysis, we analyzed 19 SNPs that showed genome-wide significant associations with schizophrenia in populations of European ancestry. Among them, nine SNPs are also associated with schizophrenia in Asian populations, suggesting that they are likely common risk genes in both populations, and provide further evidence that overlapping polygenic variation exists between ethnically divergent populations. However, the other 10 SNPs are not associated with schizophrenia in our Asian meta-analyses. As the non-significant result is unlikely attributable to influential factors of age, gender, or geography, it likely reflects the usually observed genetic heterogeneity in genetic association analyses for complex diseases, probably as a result of differential population histories. Other exogenous factors specific to different populations (culture, lifestyle, or environmental exposure) may also contribute to this observed heterogeneity. All of these phenomena highlight the genetic complexity of schizophrenia, and some susceptibility for schizophrenia is likely to result from population-specific variants.
However, extra caution should be taken in the interpretation of the results considering limitations of the data. First, we only selected the European top GWAS loci in this Asian meta-analysis, and we did not perform a fine-grained analysis for those reported regions of high susceptible SNP coverage density. Other SNPs, than the reported top GWAS loci, in the candidate genes may account for the association with schizophrenia in different regional populations. Therefore, our study should be taken as a non-replication of the European GWAS hit in Asians rather than a reflection of the whole genomic region. Second, we lacked detailed clinical information for each participant among our patients and previous GWAS cohorts and thus were not able to perform stratified analysis for each SNP in specific psychiatric phenotypes. Aggregating all patients with different subtypes together as a schizophrenia population may increase the sample size and statistical power but sometimes at the cost of camouflaging associations between SNPs and subtypes.
In summary, in large Asian samples, we independently confirmed the associations of several GWAS loci with schizophrenia, providing stronger evidence for their roles in disease development, and their biological mechanisms will become increasingly important for understanding of the etiology of schizophrenia. Our study also highlights the genetic complexity of schizophrenia. For schizophrenia, phenotypic heterogeneity of clinical symptoms still remains a major confounder for genetic association results between different ethnic populations. Consequently, the present study points out potential problems in inferring replication results of complex psychiatric disorders, such as schizophrenia, across different ethnic populations. Further studies by collecting more samples and launching extensive collaborations are needed.
References
Schizophrenia Working Group of the Psychiatric Genomics Consortium (2014) Biological insights from 108 schizophrenia-associated genetic loci. Nature 511:421–427
Saha S, Chant D, Welham J, McGrath J (2005) A systematic review of the prevalence of schizophrenia. PLoS Med 2, e141
Sullivan PF, Kendler KS, Neale MC (2003) Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60:1187–1192
O’Donovan MC, Craddock N, Norton N, Williams H, Peirce T et al (2008) Identification of loci associated with schizophrenia by genome-wide association and follow-up. Nat Genet 40:1053–1055
Stefansson H, Ophoff RA, Steinberg S, Andreassen OA, Cichon S et al (2009) Common variants conferring risk of schizophrenia. Nature 460:744–747
Rietschel M, Mattheisen M, Degenhardt F, Genetic R, Outcome in P et al (2012) Association between genetic variation in a region on chromosome 11 and schizophrenia in large samples from Europe. Mol Psychiatry 17:906–917
Lencz T, Guha S, Liu C, Rosenfeld J, Mukherjee S et al (2013) Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat Commun 4:2739
Schizophrenia Psychiatric Genome-Wide Association Study Consortium (2011) Genome-wide association study identifies five new schizophrenia loci. Nat Genet 43:969–976
Hamshere ML, Walters JT, Smith R, Richards AL, Green E et al (2013) Genome-wide significant associations in schizophrenia to ITIH3/4, CACNA1C and SDCCAG8, and extensive replication of associations reported by the Schizophrenia PGC. Mol Psychiatry 18:708–712
Ripke S, O’Dushlaine C, Chambert K, Moran JL, Kahler AK et al (2013) Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet 45:1150–1159
Li Z, Xiang Y, Chen J, Li Q, Shen J et al (2015) Loci with genome-wide associations with schizophrenia in the Han Chinese population. Br J Psychiatry 207:490–494
Takahashi S, Glatt SJ, Uchiyama M, Faraone SV, Tsuang MT (2015) Meta-analysis of data from the Psychiatric Genomics Consortium and additional samples supports association of CACNA1C with risk for schizophrenia. Schizophr Res 168:429–433
Li M, Luo XJ, Xiao X, Shi L, Liu XY et al (2011) Allelic differences between Han Chinese and Europeans for functional variants in ZNF804A and their association with schizophrenia. Am J Psychiatry 168:1318–1325
Zhang R, Lu SM, Qiu C, Liu XG, Gao CG et al (2011) Population-based and family-based association studies of ZNF804A locus and schizophrenia. Mol Psychiatry 16:360–361
Huang L, Ohi K, Chang H, Yu H, Wu L et al (2016) A comprehensive meta-analysis of ZNF804A SNPs in the risk of schizophrenia among Asian populations. Am J Med Genet B Neuropsychiatr Genet 171:437–446
Liu Z, Huang L, Luo XJ, Wu L, Li M (2015) MAOA Variants and Genetic Susceptibility to Major Psychiatric Disorders. Mol Neurobiol.
Steinberg S, de Jong S, Irish Schizophrenia Genomics Consortium, Andreassen OA, Werge T et al (2011) Common variants at VRK2 and TCF4 conferring risk of schizophrenia. Hum Mol Genet 20:4076–4081
Li M, Wang Y, Zheng XB, Ikeda M, Iwata N et al (2012) Meta-analysis and brain imaging data support the involvement of VRK2 (rs2312147) in schizophrenia susceptibility. Schizophr Res 142:200–205
Psychiatric Gwas Consortium Bipolar Disorder Working Group (2011) Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nat Genet 43:977–983
Witt SH, Juraeva D, Sticht C, Strohmaier J, Meier S et al (2014) Investigation of manic and euthymic episodes identifies state- and trait-specific gene expression and STAB1 as a new candidate gene for bipolar disorder. Transl Psychiatry 4, e426
McMahon FJ, Akula N, Schulze TG, Muglia P, Tozzi F et al (2010) Meta-analysis of genome-wide association data identifies a risk locus for major mood disorders on 3p21.1. Nat Genet 42:128–131
Sasayama D, Hori H, Yamamoto N, Nakamura S, Teraishi T et al (2014) ITIH3 polymorphism may confer susceptibility to psychiatric disorders by altering the expression levels of GLT8D1. J Psychiatr Res 50:79–83
Gu LZ, Jiang T, Cheng ZH, Zhang YC, Ou MM et al (2014) rs11098403 polymorphism near NDST3 is associated with a reduced risk of schizophrenia in a Han Chinese population. Neurosci Lett 581:42–45
Zhang C, Lu W, Wang Z, Ni J, Zhang J et al (2016) A comprehensive analysis of NDST3 for schizophrenia and bipolar disorder in Han Chinese. Transl Psychiatry 6, e701
Li T, Li Z, Chen P, Zhao Q, Wang T et al (2010) Common variants in major histocompatibility complex region and TCF4 gene are significantly associated with schizophrenia in Han Chinese. Biol Psychiatry 68:671–673
Su L, Long J, Liang B, Gu L, Pan R et al (2014) Association between the NOTCH4 gene rs3131296 polymorphism with schizophrenia risk in the Chinese Zhuang population and Chinese Han population. Acta Neuropsychiatr 26:240–245
Ikeda M, Aleksic B, Yamada K, Iwayama-Shigeno Y, Matsuo K et al (2013) Genetic evidence for association between NOTCH4 and schizophrenia supported by a GWAS follow-up study in a Japanese population. Mol Psychiatry 18:636–638
Acknowledgments
The authors are deeply grateful for the authors of the included studies to share their results. This work was supported by CAS Pioneer Hundred Talents Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors report no conflicts of interest.
Additional information
Xiao Xiao, Xiong-jian Luo and Hong Chang contributed equally to this work.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 693 kb)
Rights and permissions
About this article
Cite this article
Xiao, X., Luo, Xj., Chang, H. et al. Evaluation of European Schizophrenia GWAS Loci in Asian Populations via Comprehensive Meta-Analyses. Mol Neurobiol 54, 4071–4080 (2017). https://doi.org/10.1007/s12035-016-9990-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-9990-3