Abstract
The aim of the present study was to evaluate inflammatory, oxidative, and nitrosative stress (IO&NS) blood markers as possible predictors of multiple sclerosis (MS) and its clinical forms. This study included 258 MS patients (175 with relapsing-remitting MS (RRMS) and 83 with progressive MS clinical forms) and 249 healthy individuals. Peripheral blood samples were obtained to determine serum levels of albumin, ferritin, C-reactive protein (CRP), total protein, lipid hydroperoxide by tert-butyl hydroperoxide-initiated chemiluminescence (CL-LOOH), carbonyl protein content, advanced oxidation protein products (AOPP), nitric oxide metabolites (NOx), and total radical-trapping antioxidant parameter (TRAP). MS patients showed higher ferritin (p < 0.001) and CL-LOOH (p < 0.001) and lower albumin (p = 0.001), TRAP (p < 0.001), AOPP (p = 0.013), and NOx values (p < 0.001) than controls. Difference was not observed in CRP, total protein, and carbonyl proteins between patients and controls. In the logistic regression age-adjusted, ferritin and CL-LOOH showed positive association with MS and were predictors of MS development (OR: 1.006, 95 % CI: 1.003–1.009, p < 0.001 and OR: 1.029, 95 % CI: 1.007–1.052, p = 0.009, respectively). Albumin, TRAP, AOPP, and NOx were negatively associated with MS (p = 0.019, p = 0.003, p = 0.001, and p = 0.003, respectively). Moreover, other logistic regression age-adjusted showed that MS patients with progressive clinical forms had lower albumin and higher AOPP than those with RRMS (p = 0.037). In conclusion, ferritin, albumin, and biomarkers of IO&NS, such as CL-LOOH, AOPP, TRAP, and NOx were predictors of MS diagnosis, whereas albumin and AOPP were predictors that differentiated RRMS from the progressive clinical forms of MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is an inflammatory and degenerative neurological disease in which damage to the central nervous system (CNS) causes widespread dysfunction [1]. In early disease, active bouts of demyelination are followed by periods of remission. The clinical form in which relapses are associated with the appearance of new lesions or reactivation of old lesions in the white matter of the brain and spinal cord and alternated with remission periods is named relapsing-remitting MS (RRMS) [2]. Over time, RRMS is followed by a phase of uninterrupted disease progression, termed secondary progressive MS (SPMS). However, in 10–20 % of patients, RRMS is not present, but instead experience unremitting disease progression, named as primary progressive MS (PPMS) [3].
A growing body of evidences has shown that activated immune-inflammatory response, oxidative, and nitrosative stress (IO&NS) pathways play an important role in MS pathophysiology [4–6]. In all forms or stages of the disease, inflammation mediated by T cells, B cells, macrophages, activated microglia, and reactive oxygen and nitrogen species seem to drive demyelination and neurodegeneration. Furthermore, in the progressive stages, inflammation is increased in its extent and becomes, at least in part, trapped within the CNS behind the blood-brain-barrier (BBB) [6, 7]. Increased inflammatory status in MS patients has been demonstrated by elevation in pro-inflammatory cytokines in serum and cerebrospinal fluid (CSF) [8]. In addition, previous study from our group demonstrated that oxidative stress biomarkers were associated with clinical disability evaluated by Expanded Disability Status Scale (EDSS) [5].
MS is a disabling disease with a considerable unexplained heterogeneity in outcomes. Furthermore, the classification of MS clinical forms is still difficult [9]. We are not aware of any study, to date, in which IO&NS biomarkers were used to predict MS diagnosis and to differentiate its clinical forms in MS patients. Therefore, the objective of this study was to examine whether IO&NS biomarkers could be used as predictors of MS diagnosis and its clinical forms.
Materials and Methods
Subjects
The study included 258 MS patients, who were recruited from the Demyelinating Diseases Outpatient Department of the University of Londrina, Londrina, Paraná, Southern Brazil. The MS diagnosis was established according to the McDonald criteria [10], and the patients were classified as with RRMS (n = 175) or with MS progressive clinical forms, including PPMS and SPMS (n = 83); 220 MS patients were treated with interferon (IFN) β or other immunosuppressive drugs, and 38 were unmedicated for MS. The patients were clinically evaluated for disability using the Extended Disability Status Scale [11]. The control group consisted of 249 healthy individuals from the same geographic area. All the subjects were controlled for age, sex, ethnicity, body mass index (BMI), and waist circumference (WC). The nutritional status of the patients was similar to that of the control group. All of the individuals enrolled in the study did not drink alcohol or practiced physical activity regularly. None of them presented clinical symptoms or laboratory markers of heart, thyroid, renal, hepatic, gastrointestinal, or oncological diseases. None of the subjects were placed on a specific diet and were receiving antioxidant supplements. The protocol was approved by the Institutional Research Ethics Committees of University of Londrina, Paraná, Brazil, and all of the individuals invited were informed in detail about the research and gave written informed consent.
Demographic, anthropometric, epidemiological, and clinical characteristics, as well the use of any therapeutic drugs before the inclusion in the study were obtained using a standard questionnaire on admission. The ethnicity was self-reported as Caucasians and non-Caucasians (Black, Afro-Brazilian, and Asiatic) [12].
Anthropometric Measurements
Body weight was measured to the nearest 0.1 kg by using an electronic scale, with individuals wearing light clothing, but no shoes, in the morning; height was measured to the nearest 0.1 cm by using a stadiometer. BMI was calculated as weight (kilogram) divided by height (meter) squared. WC was measured with a tape measure, by the same professional and expressed in centimeter.
Blood Collection
Peripheral blood samples were collected without anticoagulant after fasting for 12 h. For oxidative stress evaluation, peripheral blood samples were collected with EDTA as anticoagulant. All of the samples were immediately centrifuged at 3000 rpm for 15 min, and the sera aliquots were stored in −80 °C until use.
Biochemical and Inflammatory Markers
Ferritin levels were determined by chemiluminescent microparticle immunoassay (CMIA; Architect, Abbott Laboratory, Abbott Park, IL, USA). Uric acid, albumin, and total protein were evaluated by a biochemical auto-analyzer (Dimension Dade AR Dade Behring, Deerfield, IL, USA). Serum levels of high sensitivity CRP (hsCRP) were determined using a turbidimetric assay (ARCHITECT c8000, Architect, Abbott Laboratory, Abbott Park, IL, USA).
Oxidative Stress Biomarkers
Tert-butyl Hydroperoxide-initiated Chemiluminescence (CL-LOOH)
Lipid hydroperoxides in plasma were evaluated by CL-LOOH as described previously [13], a method with higher sensitivity and specificity than the thiobarbituric acid reactive substances (TBARS) measurement, the usual method to determine lipid oxidation. The results were expressed in counts per minute (cpm).
Determination of Advanced Oxidation Protein Products (AOPP)
AOPP was determined in the plasma samples using the semi-automated method [14]. AOPP results from oxidation of amino acid residues such as tyrosine, leading to the formation of dityrosine-containing protein cross-linking products detected by spectrophotometry. AOPP concentrations were expressed as micromoles per Liter (umol/L) of chloramines-T equivalents.
Carbonyl Protein Content
Carbonyl content was measured as an estimate of protein oxidative injury. Carbonyl protein content was determined as described previously by [15]. The results are expressed in nmol/mL/mg total proteins.
Nitric Oxide (NO)
Serum NO metabolite (NOx) levels were assessed by nitrite (NO2 −) and nitrate (NO3−) concentration according to the Griess reaction, supplemented by the reduction of nitrate to nitrite with cadmium [15]. The values were expressed as micrometer.
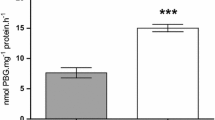
Total Radical-trapping Antioxidant Parameter (TRAP)
The TRAP was determined as reported previously [16]. This method detects hydrosoluble and/or liposoluble plasma antioxidants by measuring the chemiluminescence inhibition time induced by 2,2-azobis(2-amidinopropane). The system was calibrated with the vitamin E analog TROLOX, and the values of TRAP were expressed in equivalent of micrometer Trolox/UA mg/dL.
Statistical Analyses
Analyses of contingency tables (x 2 test) were used to evaluate the associations between the characteristics of two study groups (patients and controls). Differences in demographic, clinical, and blood marker data between MS patients and controls were ascertained using analyses of variance (ANOVAs). Fisher’s protected least significant difference (LSD at p < 0.05) was used to examine multiple comparisons between three study groups (RRMS, progressive MS, and controls). Bivariate logistic regression analysis was used to define the significant predictor, with odds ratio (OR) and 95 % confidence intervals (CI) of MS versus controls using the markers and other significant characteristic data. Multinomial logistic regression analysis was employed to delineate the significant predictors of RRMS and other MS clinical forms (progressive MS) versus controls using the markers and other significant characteristic data. Tests for homogeneity of variance were carried out when appropriate (Levene test). Degree of freedom (df) was also demonstrated. All tests were two-tailed, and a p value of 0.05 was used for statistical significance.
Results
Characteristics of the MS Patients and Controls
Table 1 shows the baseline characteristics of the MS patients and controls included in this study. We did not use Bonferroni p-corrections to interpret the multiple statistical analyses listed in Table 1 that examines the differences in demographic, anthropometric, and clinical characteristics between the two groups. Indeed, the results of these univariate statistical analyses were used to delineate the significant explanatory variables to be used as determinants of independent association with diagnostic groups in subsequent logistic regression analyses. Without p-correction, we found that controls were younger than MS patients and subsequently age was used as an additional explanatory variable in logistic regression analyses. As expected, there were no significant differences in female:male ratio, self-reported ethnicity, BMI, and WC between the two groups, since these variables were controlled.
Blood Marker Differences Between MS Patients and Controls
Table 2 shows the outcome of ANOVAs performed on the different blood markers that were evaluated in the present study. We found no significant differences in hsCRP, total protein, and carbonyl protein levels when MS patients and controls were compared. MS patients showed lower albumin (p = 0.001), TRAP (p < 0.001), AOPP (p = 0.013), and NOx (p = 0.001) values, but higher ferritin (p < 0.001) and CL-LOOH (p < 0.001) values than controls. General linear model (GLM) analyses with sex as a second factor and age as covariate did not change any of these results.
Table 3 shows the outcome of a logistic regression analysis with MS group as dependent variable and the controls as the reference group and the significant blood markers shown in Table 2 as explanatory variables (x 2 = 91.15, df = 6, p < 0.001; Nagelkerke = 0.412). We found that ferritin and CL-LOOH were significantly and positively associated with MS, whereas albumin, TRAP, AOPP, and NOx were significantly and negatively associated with MS. Using this regression analysis, 82.7 % of all subjects were correctly classified with a sensitivity of 73.6 % and a specificity of 89.5 %.
Effects of Background Variables
Because there were differences in age between the two diagnostic groups, the logistic regression analysis was re-run with age as additional covariate. Table 4 shows that all significances reported in Table 3 remained significant (x 2 = 97.41, df = 7, p < 0.001; Nagelkerke = 0.435). Forced entry of BMI (Wald = 0.32, df = 1, p = 0.572), ethnicity (Wald = 1.15, df = 1, p = 0.282), and sex (Wald = 1.93, df = 1, p = 0.165) showed that these variables were not significant in predicting MS and did not change the associations between the biomarkers and MS. Since the drug state of the patients could be another possible factor modulating biomarker levels, their effects were evaluated on the results using ANOVA. This analysis showed no significant differences between MS patients treated or unmedicated in the levels of ferritin (F = 3.34, df = 1/160, p = 0.069), albumin (F = 0.01, df = 1/162, p = 0.935), TRAP (F = 0.13, df = 1/126, p = 0.723), CL-LOOH (F = 1.79, df = 1/123, p = 0.183), AOPP (F = 0.01, df = 1/106, p = 0.955), NOx (F = 1.55, df = 1/113, p = 0.216), carbonyl proteins (F = 0.95, df = 1/112, p = 0.332) (data not shown).
Characteristics of RRMS patients
As shown in Table 1, we included 175 patients with RRMS and 83 with progressive clinical forms of MS, named as other subtypes, and the values of the biomarkers between these two MS subgroups and controls were compared. Table 5 shows the outcome of ANOVAs and protected LSD tests (performed at p < 0.05). All the biomarkers evaluated, except carbonyl protein groups, were significantly different between the RRMS, other subtypes, and controls. Ferritin and CL-LOOH were significantly higher in both MS subgroups than in controls (p < 0.001); albumin was significantly lower in MS patients with progressive forms than in controls and those with RRMS (p < 0.001); TRAP and NOx were significantly lower in both MS subgroups than in controls (p = 0.002 and p < 0.001, respectively); and AOPP was significantly lower in RRMS than in controls (p = 0.013).
Table 6 shows the outcome of a multinomial logistic regression analysis with the two subgroups of MS patients and controls as dependent variable and the biomarkers and age as explanatory variables. The overall regression was highly significant (x 2 = 116.20, df = 14, p < 0.001; Nagelkerke = 0.446). Patients with other MS subtypes were significantly differentiated from controls by increased ferritin and lowered albumin levels. Patients with RRMS were significantly differentiated from controls by increased ferritin and CL-LOOH and lowered TRAP, AOPP, and NOx. Albumin and AOPP were significantly different between patients with RRMS versus those with other MS clinical forms.
Discussion
The main finding of the present study was that ferritin and albumin and some oxidative stress blood markers (CL-LOOH, AOPP, NOx, and TRAP) may be considered as predictors of MS, independently of sex, age, and treatment of the patients. In this model of analysis, 82.7 % of MS patients were correctly classified with MS, with sensitivity of 73.6 % and specificity of 89.5 %. The second major finding of this study was that patients with progressive clinical forms of MS presented lower levels of albumin and higher AOPP levels than those with RRMS.
In the current study, patients with MS showed significant increase in lipid hydroperoxides, measured using plasma chemiluminescent method, and this result is in agreement with other studies, which demonstrated increased lipid peroxidation, but using different methods [4, 17]. Previous study [5] showed an association between oxidative stress measured by plasma chemiluminescence and disability of the MS patients and that lipid peroxidation was present even in patients in clinical remission, suggesting that at least at the molecular level the neurological damage process could be continuous and could lead to the progression of the disease.
Unexpectedly, AOPP was lower in MS patients when compared in controls and between the MS clinical forms. The decreased AOPP in MS patients could be explained by several factors. Some pro-oxidant decreased levels may be related to MS pathophysiology and to the role of reactive substances and their metabolites in redox signaling. For instance, irreversible modifications induced by oxidative stress, such as protein oxidation, are generally associated with permanent loss of protein function and may lead to the progressive accumulation of damage proteins. In cells, the level of progressive accumulation of modified proteins reflects the balance between the rate of protein oxidation and the rate of oxidized protein degradation, and is dependent of multiple factors that influence the levels of pro- and antioxidant and the levels of proteases that catalyze the degradation of oxidized protein residues [18, 19]. Thus, different diseases in different phases may present a different profile in oxidative stress markers.
Our data also showed that the serum levels of NOx were lower in MS patients compared in controls. There have been conflicting results regarding the role of nitric oxide (NO) in the pathophysiology of MS [20, 21]. While some studies demonstrated elevated NOx levels among the MS patients [21], others showed lower levels [5, 20]. These conflicting results could be explained by some factors, including the effect of therapies on NO, such as IFN-β, which can decrease induced-NO synthesis in a dose-dependent manner by the inhibition of inducible NO synthase (iNOS) [22]. In this study, 158 patients were treated with IFN-β, which may influence the results obtained. It is also likely that the reduction in NOx levels is associated with redox imbalance demonstrated in this study. It is known that inflammation elevates reactive oxygen species levels and that increased NO consumption occurs with high inflammatory activity, resulting in decreased serum NOx bioavailability. Furthermore, NO is consumed when it reacts with superoxide anion, producing the strong oxidant species peroxynitrite (ONOOH−) [5, 23] that is toxic for oligodendrocytes and axons and seems to be a key molecule of IO&NS involved in the pathophysiological mechanisms of MS [24].
Antioxidant deficiencies may occur during the clinical course of MS as result of chronic inflammation that is accompanied by increased oxidative stress [25]. Taken together our results show changes in the redox status in MS patients. Our group has already demonstrated significant increased plasma lipid oxidation and a strong decrease in plasma total antioxidant capacity in patients with MS [5]. Similar results were obtained in the present study; however, with an additional result suggesting that these markers could be predictors of MS development.
Elevated serum levels of ferritin during the inflammatory response are due to release from damaged tissues, increased synthesis, as well as decreased clearance of this positive acute phase protein; therefore, it may play an important role as pro-oxidant molecule [19, 26]. In addition, IFN-β therapy increases ferritin concentration in MS patients [27]. Among the MS patients included in the present study, 61.2 % were in treatment with IFN-β; however, the analysis showed that significant differences were not observed in the serum levels of ferritin and other blood markers among those treated or unmedicated patients. Nevertheless, controversy exists whether ferritin has pro- or antioxidant properties. Oligodendrocytes have high concentrations of ferritin and iron [1, 28], and elevated ferritin levels could be a defense mechanism against iron-induced oxidative injury. However, observations that superoxide can mobilize iron from ferritin suggest that exposure to oxygen radicals may, in fact, increase the pool of reactive iron and exacerbate oxidant injury [29]. Taken together with the other data verified in the oxidative status of MS patients, our study is in agreement with the later hypothesis.
In the present study, ferritin and CRP did not differ when the MS clinical forms were compared, contrasting from higher levels of ferritin obtained in CSF samples of patients with progressive forms of MS [1]. The variability among different ethnic populations, degree of disability of MS patients, time for sample collection in the long-term evolution of the disease, and different assays used by previous studies, also could contribute to some divergent results.
Albumin is a negative acute phase reactant and constitutes an important extracellular antioxidant defense in blood plasma. This protein possesses antioxidant properties, such as binding copper tightly and iron weakly, scavenging free radicals, hypochlorous acid (HOCl) and peroxynitrite, and providing thiol group [30]. In the present study, it is possible that the decreased albumin levels could contribute to oxidative and nitrosative stress verified in MS patients. The reduced levels of albumin and AOPP were the only biomarkers capable of differentiating RRMS from the other clinical forms.
The change verified in the levels of acute phase proteins, ferritin, and albumin, in the present study may have contributed to the redox imbalance and immune-inflammatory burden in MS. The interplay between all of these factors leads to self-amplifying feed forward loops causing a chronic state of activated IO&NS, immune-inflammatory and autoimmune pathways, which may sustain the disease.
There are limitations in the current study that may be considered. First, the single-point measurement of the IO&NS markers since repeated measures should be necessary to define the variance of our findings, as well as the predictive nature of a biomarker. However, in support to our findings, several studies previously reported the usefulness of a single-point measurement of these markers in MS. Second is the relative small number of individuals with progressive MS clinical forms. In contrast, strengths of our study are the adjusted results performed for many potential confounders, including age, sex, ethnicity, and MS therapy. In addition, this study evaluated the IO&NS with several different methodologies making possible to find biomarkers, which could be adequate and useful as predictive model for evaluating MS patients.
In conclusion, we have constructed a model of MS diagnosis in which IO&NS biomarkers, such as ferritin, albumin, CL-LOOH, AOPP, TRAP, and NOx were the main predictors, whereas albumin and AOPP were the predictors that differentiated RRMS from the MS progressive clinical forms. Further studies with large number of patients are warranted to confirm the present results.
References
LeVine SM, Lynch SG, Ou CN, Wulser MJ, Tam E, Boo N (1999) Ferritin, transferrin and iron concentrations in the cerebrospinal fluid of multiple sclerosis patients. Brain Res 821:511–515
Scalfari A, Neuhaus A, Daumer M, Muraro PA, Ebers GC (2014) Onset of secondary progressive phase and longterm evolution of multiple sclerosis. J Neurol Neurosurg Psychiatry 85:67–75
Lublin FD, Reingold SC (1996) Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology 46:907–911
Ferretti G, Bacchetti T, Principi F, Di Ludovico F, Viti B, Angeleri VA, Danni M, Provinciali L (2005) Increased levels of lipid hydroperoxides in plasma of patients with multiple sclerosis: a relationship with paraoxonase activity. Mult Scler 11:677–682
Oliveira SR, Kallaur AP, Simão AN, Morimoto HK, Lopes J, Panis C, Petenucci DL, da Silva E et al (2012) Oxidative stress in multiple sclerosis patients in clinical remission: association with the expanded disability status scale. J Neurol Sci 321:49–53
Haider L (2015) Inflammation, Iron, Energy Failure, and Oxidative Stress in the Pathogenesis of Multiple Sclerosis. Celular Oxid Med Longev 2015:725.370
Rossi S, Motta C, Studer V, Barbieri F, Buttari F, Bergami A, Sancesario G, Bernardini S et al (2014) Tumor necrosis factor is elevated in progressive multiple sclerosis and causes excitotoxic neurodegeneration. Mult Scler 3:304–312
Matsushita T, Tateishi T, Isobe N, Yonekawa T, Yamasaki R, Matsuse D, Murai H, Kira J (2013) Characteristic cerebrospinal fluid cytokine/chemokine profiles in neuromyelitis optica, relapsing remitting or primary progressive multiple sclerosis. PLoS One 4, e61835
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, McFarland HF, Paty DW et al (2001) Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 50:121–127
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Brazil IBGE (2011) Brazilian Institute of Geography and Statistics. Characteristics of the Population and Households: Results of the Universe. Available in://http://www.ibge.gov.br/english/estatistica/populacao/censo2010/caracteristicas_da_populacao/default_caracteristicas_da_populacao.shtm. Accessed 16 July, 2013.
Gonzales-Flecha BG, Llesuy S, Boveris A (1991) Hydroperoxide-initiated chemiluminescence: an assay for oxidative stress in biopsies of heart, liver and muscle. Free Radic Biol Med 10:93–100
Witko-Sarsat V, Friedlander M, Nguyen Khoa T, Capeillère-Blandin C, Nguyen AT, Canteloup S, Dayer JM, Jungers P et al (1998) Advanced oxidation protein products as novel mediators of inflammation and monocyte activation in chronic renal failure. J Immunol 161:2524–2532
Panis C, Herrera AC, Victorino VJ, Campos FC, Freitas LF, De Rossi T, Colado Simão AN, Cecchini AL et al (2012) Oxidative stress and hematological profiles of advanced breast cancer patients subjected to paclitaxel or doxorubicin chemotherapy. Breast Cancer Res Treat 133:89–97
Repetto M, Reides C, Gomez Carretero ML, Costa M, Griemberg G, Llesuy S (1996) Oxidative stress in blood of HIV infected patients. Clin Chim Acta 255:107–117
Koch M, Mostert J, Arutjunyan AV, Stepanov M, Teelken A, Heersema D, De Keyser J (2007) Plasma lipid peroxidation and progression of disability in multiple sclerosis. Eur J Neurol 14:529–533
Grune T, Merker K, Sandig G, Davies KJ (2003) Selective degradation of oxidatively modified protein substrates by the proteasome. Biochem Biophys Res Commun 3:709–718
Lozovoy MA, Simão AN, Oliveira SR, Iryioda TM, Panis C, Cecchini R, Dichi I (2013) Relationship between iron metabolism, oxidative stress, and insulin resistance in patients with systemic lupus erythematosus. Scand J Rheumatol 4:303–310
de Bustos F, Navarro JA, de Andrés C, Molina JA, Jiménez-Jiménez FJ, Ortí-Pareja M, Gasalla T, Tallón-Barranco A et al (1999) Cerebrospinal fluid nitrate levels in patients with multiple sclerosis. Eur Neurol 41:44–47
Danilov AI, Andersson M, Bavand N, Wiklund NP, Olsson T, Brundin L (2003) Nitric oxide metabolite determinations reveal continuous inflammation in multiple sclerosis. J Neuroimmunol 136:112–118
Guthikonda P, Baker J, Mattson DH (1998) Interferon-beta-1-b (IFN-β) decreases induced nitric oxide (NO) production by a human astrocytoma cell line. J Neuroimmunol 82:133–139
Simão AN, Lozovoy MA, Simão TN, Venturini D, Barbosa DS, Dichi JB, Matsuo T, Cecchini R et al (2011) Immunological and biochemical parameters of patients with metabolic syndrome and the participation of oxidative and nitroactive stress. Braz J Med Biol Res 44:606–728
Gonsette RE (2008) Neurodegeneration in multiple sclerosis: the role of oxidative stress and excitotoxicity. J Neurol Sci 274:48–53
van Meeteren ME, Teunissen CE, Dijkstra CD, van Tol EA (2005) Antioxidants and polyunsaturated fatty acids in multiple sclerosis. Eur J Clin Nutr 59:1347–1361
Wang W, Knovich MA, Coffman LG, Torti FM, Torti SV (2010) Serum ferritin: past, present and future. Biochim Biophys Acta 1800:760–769
Strupp M (2010) News on multiple sclerosis: induction of immune tolerance, a biomarker for predicting disease activity, and CSF ferritin levels. J Neurol 257:2114–2116
Connor JR, Boeshore KL, Benkovic SA, Menzies SL (1994) Isoforms of ferritin have a specific cellular distribution in the brain. J Neurosci Res 37:461–465
Arosio P, Levi S (2002) Ferritin, iron homeostasis, and oxidative damage. Free Radic Biol Med 33:457–463
Sitar ME, Aydin S, Cakatay U (2013) Human serum albumin and its relation with oxidative stress. Clin Lab 59:945–949
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oliveira, S.R., Kallaur, A.P., Reiche, E.M.V. et al. Albumin and Protein Oxidation are Predictors that Differentiate Relapsing-Remitting from Progressive Clinical Forms of Multiple Sclerosis. Mol Neurobiol 54, 2961–2968 (2017). https://doi.org/10.1007/s12035-016-9860-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-9860-z